"Uh-oh... maybe I should have referred that"
Five case studies that highlight the importance of timely veterinary dental referrals.
Next >
We all have those moments in our practice when we think we may have gotten in over our heads. When that happens, referral is the best option to avoid patient discomfort or complications from neglecting to resolve the problem.
Here are five of many cases I've seen as a dental specialist. All but the first one-a mandibular canine extraction attempt that resulted in a rostral mandibular fracture-failed to refer at the time of the mishap.

Figure 1A
Case 1: Rostral mandibular fracture
Performing surgical extractions in dogs and cats requires advanced training that includes attending lectures and labs led by board-certified veterinary dentists. Initial instruction should be followed by extensive practice on cadavers until your speed and competency are consistent. During training in dogs, the mandibular first molar and maxillary fourth premolar extractions should routinely take less than 25 minutes each to complete before you perform these procedures on a live patient. It's crucially important to achieve this level of competency with cadavers first.
Mandibular canine teeth are particularly challenging because of the density of cortical bone and the inability to extend bone removal to the apical extent of the tooth. Figure 1A demonstrates a rostral mandibular fracture secondary to an attempt to extract a partially erupted canine tooth. Referral was correctly sought at the time of fracture.
Case 1 cont'd
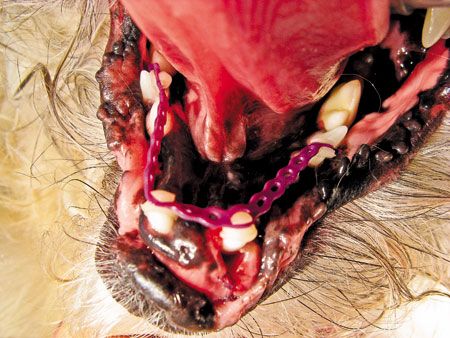
Figure 1B
A splint made of composite buttons, Masel chain and acrylic (Figure 1B) stabilized the fracture in correct occlusion (Figure 1C, see next page), and healing progressed without incident. The splint was removed after radiographic confirmation of adequate callous formation in four to six weeks. The canine teeth did not require extraction and were treated with apically positioned flaps.
Case 1 cont'd

Figure 1C

Figure 2A
Case 2: Oronasal fistula
Oronasal fistulas result from inadequate exposure and closure of maxillary extraction sites. They occur most commonly because of maxillary canine extractions, as in the dog in Figure 2A.
Case 2 cont'd

Figure 2B
Chronic nasal discharge (Figure 2B) and sneezing are common results of oral and nasal communication.
In this case of bilateral oronasal fistulas in a dog, closure was attempted at the time of the initial extraction. Dehiscence resulted in two additional attempts before referral. Flap tension due to inadequate exposure is the reason for most oronasal fistula repair failures.
Case 2 cont'd

Figure 2C
As in this case, adequate exposure, débridement (Figure 2C) and closure (Figure 2D, see next page) by a board-certified veterinary dentist is the recommended approach to resolve oronasal fistulas. Analgesics and perhaps a short course (five days) of antibiotics can complete treatment.
Bacterial culture and antimicrobial sensitivity testing may be needed in the occasional case of a patient with persistent signs. Also consider allergic rhinitis in some persistent cases.
Case 2 cont'd

Figure 2D

Figure 3A
Case 3: Chronic facial lesion
Often, chronic facial lesions are a result of oral pathology. The most common manifestation is a suborbital fistula secondary to periodontal disease or endodontic disease associated with the maxillary fourth premolar.
This patient's right maxillary fourth premolar was extracted one year before presentation (Figure 3A). A chronically recurring lesion periodically responsive to antibiotics was noted rostral and ventral to the classic suborbital location. The patient was lethargic and anorectic. Neoplasia was a consideration.
Case 3 cont'd

Figure 3B
Radiographs revealed a root tip that was left from the extraction (Figure 3B).
Case 3 cont'd
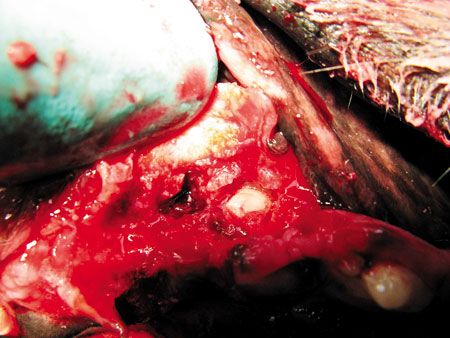
Figure 3C
Extraction of the tip (Figure 3C) resulted in fast resolution of the defect and clinical signs. Root tips always should be removed to prevent this common problem. Cases in which tooth fragments left after extraction lead to complications such as facial lesions often result in litigation, so preoperative and postoperative radiographs are essential in every patient undergoing an extraction to ensure complete removal.

Figure 4A
Case 4: Pathologic mandibular fracture
Noninvasive repair is readily accomplished in most mandibular fractures by using existing teeth to construct splints that normalize occlusion and provide stabilization for healing. Pathologic fractures secondary to periodontal disease pose considerable challenges. They occur most commonly because of improper extraction techniques in which periodontal disease has compromised bone to the point of near fracture (Figure 4A). Most occur as a result of failure to obtain radiographs before extraction. These cases always should be referred to a veterinary dentist for definitive care.
In cases of pathologic mandibular fracture, severe bone compromise and an edentulous mandible are often present. Further compromise of bone occurs when plates are used for repair. Tooth roots and inferior alveolar neurovascular damage are common secondary to improper screw placement.
Case 4 cont'd

Figure 4B
This patient presented 2 1/2 years after repair of a pathologic fracture secondary to an extraction attempt on the left mandibular first molar. Mobility of the plate due to the lack of screw purchase in severely compromised bone resulted in inevitable failure (Figure 4B).
Case 4 cont'd

Figure 4C
Because of the severe compromise of this patient's bone (Figures 4C and 4D, see next page), mandibulectomy was the treatment of choice.
Case 4 cont'd

Figure 4D
Case 4 cont'd

Figure 4E
Only board-certified veterinary dentists or surgeons should attempt plate placement for any mandibular fracture. Mini-plates are available for this purpose, but splints are the noninvasive procedure of choice. The patient in Figure 4E (a different one than that pictured in Figures 4A-4D) had bilateral mandibular fractures. Both mandibles had only the mandibular canines present. Two circum-mandibular wires were placed rostral and caudal to each fracture site, and a device similar to that in Case 1 was constructed. This case, among others, was presented in detail in “Bilateral mandibular fractures due to periodontal disease,” available at dvm360.com/MandibularFracture.
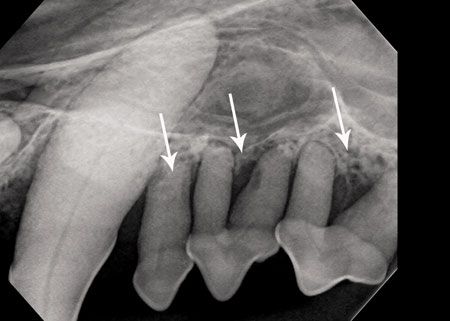
Figure 5A
Case 5: Occult periodontal disease
By far the most common reason for referral is the failure to take dental radiographs when performing a dental cleaning. Skull radiographs are not diagnostic for dental pathology and should not be considered as part of the workup for periodontal disease. Rather, full-mouth dental radiographs are the standard of care for any patient receiving a dental cleaning.
The patient in Figures 5A and 5B (see next page) had a dental prophylaxis just four months before presentation. Persistent odor and inflammation led the owner to seek referral, which was not originally offered by the referring veterinarian. The figures show only two regions where multiple extractions were indicated; 24 teeth in all required extraction because of stage three or four periodontal disease.
Litigation is on the rise in cases just like this, which happen every day in practice. Dental radiography of the entire mouth is indicated in every dentistry case. Occult periodontal disease is the rule, not the exception.
Case 5 cont'd
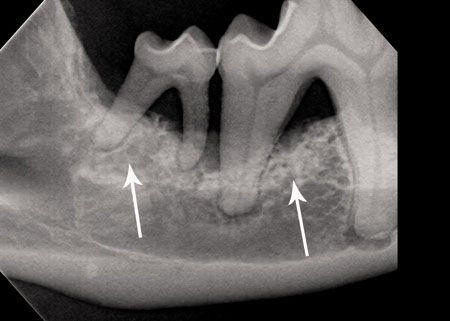
Figure 5B