Case example 1: A border collie with a possible foreign body
A 5-year-old 37.6-lb (17.1-kg) neutered male border collie has a three-day history of vomiting.
Signalment and history: A 5-year-old 37.6-lb (17.1-kg) neutered male border collie has a three-day history of vomiting. A surgical abdominal exploration for a gastrointestinal foreign body is scheduled. The patient's baseline arterial blood gas results are shown to the left.
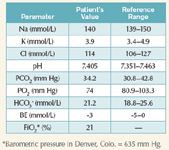
Interpretation: The patient's acid-base status and arterial blood gases are normal. The PO2 suggests relative hypoxemia, but when barometric pressure (PB) is considered and the alveolar-arterial oxygen difference is calculated, the value is normal. The alveolar gas equation is used to estimate expected partial pressure of oxygen in the alveolus (PAO2).
PAO2 = (PB – PH2O) x FiO2 – (PaCO2/0.8)
= (635 mm Hg – 47 mm Hg) X 0.21 – (34 mm Hg/0.8)
= 81 mm Hg
PH2O is the partial pressure of water vapor in the inspired air. The value depends on body temperature and is usually assumed to be 47 mm Hg at 37 C.
Next the A-a oxygen difference can be calculated to help differentiate between pulmonary and extrapulmonary causes.
P(A-a)O2 = PAO2 – PaO2
= 81 mm Hg – 74 mm Hg
= 7 mm Hg
The normal A-a oxygen difference in an animal breathing room air is less than 15 mm Hg at sea level, although up to 25 mm Hg is considered normal. This result suggests that the cause of the low PaO2 is extrapulmonary (decreased atmospheric oxygen).
Fifteen minutes after anesthetic premedication with 0.1 mg/kg intravenous hydromorphone, induction with 6 mg/kg intravenous propofol, and maintenance with isoflurane in oxygen (spontaneous ventilation) the patient's arterial blood gas results are shown to the right.
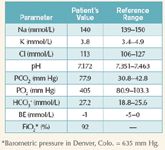
Interpretation: The pH indicates an acidemia. Analysis of the PCO2 indicates significant hypercapnea that would result in a respiratory acidosis. The HCO3 - change is in the opposite direction to the primary problem, suggesting it is compensation for a primary problem. The traditional interpretation would be a respiratory acidosis with incomplete (early) metabolic compensation. Oxygen partial pressure is much increased over baseline, but the difference is due to an increase in FiO2.
This is an example of significant respiratory acidosis due to anesthetic respiratory depression. Treatment of the acidosis in this case is by controlled positive pressure ventilation. Restoring normal PCO2 will rapidly correct the acidosis; however, if CO2 continues to rise, the anesthetic effect of the carbon dioxide will add to the inhalant anesthetic effect and cause excessively deep anesthesia.
Sodium bicarbonate administration is contraindicated in this and all primary respiratory acidosis cases. Treatment is to improve ventilation.
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen