Clinical Exposures: Intervertebral disk disease in a dog with agenesis of a cervical vertebra
A 65-lb (29.5-kg) 6-year-old spayed female Doberman pinscher was presented for evaluation of a one-month history of progressive left forelimb lameness.
A 65-lb (29.5-kg) 6-year-old spayed female Doberman pinscher was presented for evaluation of a one-month history of progressive left forelimb lameness. The physical examination revealed a weightbearing lameness of the left forelimb with mild muscle atrophy in the left forelimb, especially over the spine of the scapula. No swelling, joint effusion, or pain was detected on palpation of the limb. Pain was elicited on cervical extension. A neurologic examination revealed delayed conscious proprioception of the left forelimb, with slightly delayed conscious proprioception in the left hindlimb. All segmental spinal reflexes and all other neurologic responses were normal. No other abnormalities were noted on the remainder of the physical examination. Differential diagnoses for the dog's condition included cervical intervertebral disk extrusion, cervical vertebral malformation-malarticulation, and neoplasia involving the spine, vertebrae, or brachial plexus.

Figure 1 : Lateral radiograph of the cervical spine of the dog in this case. Note the incomplete formation and separation of C3.
Diagnostic tests
Our diagnostic plan included a complete blood count, a serum chemistry profile, survey spinal radiography, and myelography with possible cerebrospinal fluid analysis. The results of the complete blood count and serum chemistry profile were normal.

Figure 2 : Ventrodorsal radiograph of the cervical spine of the dog in this case. Note the incomplete formation and separation of the elongated body of C4.
We premedicated the dog with morphine sulfate and glycopyrrolate, both administered subcutaneously. General anesthesia was induced with thiopental sodium, given intravenously. Anesthesia was maintained with isoflurane. A survey spinal radiographic examination revealed only six distinct cervical vertebrae, with apparent incomplete separation of the second and third cervical vertebrae (Figures 1 & 2). The fourth cervical vertebral body was elongated.
Myelography was performed by injecting 0.3 ml/kg iohexol (240 mg iodine/ml) at the cisterna magna. The myelogram revealed marked extradural ventral spinal cord compression over the C5-C6 disk space (Figures 3 & 4). No change in the lesion was noted radiographically in response to traction, flexion, or extension.
Diagnosis and treatment
The static ventral cord compression was highly indicative of a prolapsed intervertebral disk at C5-C6. The other vertebral abnormalities were consistent with cervical vertebral malformation-malarticulation. Because there was no dynamic component and the lesion was nontraction-responsive, we performed a ventral slot fenestration at C5-C6 immediately after the myelography. A large amount of degenerative disk material was removed from the spinal canal.
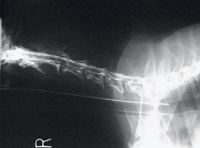
Figure 3 : Lateral myelogram of the cervical spine. Note the marked ventral extradural compression at C5.
Postoperatively, the dog was given intravenous fluids at a maintenance rate, and 0.5 mg/kg morphine was administered subcutaneously every four to six hours or as needed for pain. We administered intravenous methylprednisolone sodium succinate intraoperatively at a dose of 30 mg/kg, followed by a 15-mg/kg dose two hours later and then every six hours for 24 hours. This was followed by administration of 0.5 mg/kg prednisone twice a day for five days and then 0.5 mg/kg every other day for five days. Famotidine was given at 0.5 mg/kg twice a day while the dog was in the hospital. Fluids were discontinued after two days, once the dog was eating and drinking normally.
Twenty-four hours after surgery, the dog was nonambulatory and tetraparetic. While recumbent, the dog was turned over every four hours and later assisted to rise with a sling. Three days later, the dog was able to stand and walk unassisted and was discharged from the hospital with strict exercise restrictions for four weeks and harness walks only. The dog was clinically normal two weeks after surgery. Six months after surgery, the dog remained normal, with no recurrence of lameness, ataxia, or neck pain.

Figure 4 : Ventrodorsal myelogram of the cervical spine. Note the marked ventral extradural compressionat C6.
Discussion
Cervical intervertebral disk disease is typically divided into disk extrusions (Hansen type I), in which degenerated disk material is herniated into the spinal canal, and disk protrusions (Hansen type II), in which the dorsal annulus of the disk is hypertrophied and compresses the spinal canal. In large-breed dogs, cervical intervertebral disk disease is usually associated with disk protrusion at disk spaces C5-C7.1 Seventy-six percent of cases of cervical intervertebral disk disease extrusions occur in small, chondrodystrophic dogs, with only 24% occurring in large-breed dogs.2 Dogs with cervical intervertebral disk disease usually present with neck pain and minimal neurologic deficits.1
Cervical vertebral malformation-malarticulation is also known as wobbler syndrome, cervical spondylopathy, caudal cervical spondylomyelopathy, and cervical vertebral instability. It is a common condition in young great Danes and older Doberman pinschers.3 Cervical vertebral malformation-malarticulation consists of a variety of clinical malformations, including ligamentum flavum hypertrophy, vertebral malformations, vertebral tipping with inappropriate movement between adjacent vertebrae, and cervical disk protrusion with hypertrophy of the dorsal annulus fibrosus.4 Hansen type I disk prolapse into the vertebral canal is unusual. Spinal cord compression is most frequently caused by bulging of the annulus fibrosus.5 Cervical vertebral malformation-malarticulation lesions can be either static or dynamic. Dynamic lesions secondary to vertebral instability on cervical flexion are seen most commonly.3,6
Dogs with this condition usually present with ataxia and conscious proprioceptive deficits. The hindlimbs are more severely affected than the forelimbs because of the anatomical location of the nerve tracts in the caudal cervical region. Neck pain is a rare presenting sign.3 The speculated pathophysiology of cervical vertebral malformation-malarticulation in older Doberman pinschers is that of subtle primary bone malformations resulting in chronic instability and disk hypertrophy and degeneration later in life.6 In this case, the only evident problems were cervical pain and forelimb lameness resulting from the disk prolapse.
Treatment decisions are based on the patient's history, neurologic status, and radiographic signs, including the nature of the compressive lesion. For either intervertebral disk disease or cervical vertebral malformation-malarticulation, surgery is usually recommended in dogs with severe neck pain, progressive neurologic deficits, or both. Without surgical treatment, cervical vertebral malformation-malarticulation progresses in most dogs, leading to spinal cord atrophy.7 In chronic cases, often the best possible outcome after surgery is arrest of the disease's progression, rather than return to normal function.
With surgery, two broad treatment categories exist: direct access decompression, and distraction and stabilization techniques.8 Clinical improvement after surgery results from immediate spinal cord decompression, elimination of dynamic compression through increased vertebral stability, or gradual decompression as hypertrophied soft tissues atrophy after increased stability.9 The technique of choice for osseous compressions is a dorsal laminectomy. The preferred technique for ventral, soft tissue, nontraction-responsive lesions (including cervical disk prolapse) remains a ventral slot fenestration. The controversy lies in the treatment of traction-responsive, soft tissue lesions.10 These dynamic lesions are treated with a variety of techniques including ventral slot decompression, disk fenestration, vertebral body fusion, continuous dorsal cervical laminectomy, dorsal laminectomy, and distraction and fusion.7-12 With cervical intervertebral disk disease, success rates of 99% have been reported.2 With cervical vertebral malformation-malarticulation, the short-term success rate is about 80%, regardless of the procedure performed.7 About 20% of dogs with cervical vertebral malformation-malarticulation will have a recurrence, often from protrusion of additional intervertebral disks (i.e. domino lesions) or recurrence at the same site.7,10
This case demonstrates an intervertebral disk extrusion and cervical vertebral abnormalities in the form of incomplete formation and separation of the third cervical vertebra, with resulting abnormalities of the second and fourth cervical vertebrae. Radiographically, the ventral compression at the site of the disk rupture was static with no dynamic component. However, alterations in forces upon the intervertebral disk at C5-C6 due to the adjacent vertebral abnormalities may have existed. Studies have suggested that abnormal physical forces induce changes in disk composition, which could predispose disk extrusion.13 This may represent an interesting variant of cervical vertebral malformation-malarticulation not previously reported.
The photographs and information for this case were provided by Stephanie Lister, DVM, 920 Yonge St., Suite 117, Toronto, ON M4W 3C7; and Bradley R. Coolman, DVM, MS, DACVS, and Roy A. Coolman, DVM, 5818 Maplecrest Road, Fort Wayne, IN 46835.
REFERENCES
1. Coates JR. Intervertebral disk disease. Vet Clin North Am Small Anim Pract 2000;30:77-110.
2. Cherrone KL, Dewey CW, Coates JR, et al. A retrospective comparison of cervical intervertebral disk disease in nonchondrodystrophic large dogs versus small dogs. J Am Anim Hosp Assoc 2004;40:316-320.
3. Lewis DG. Cervical spondylomyelopathy ('wobbler' syndrome) in the dog: A study based on 224 cases. J Small Anim Pract 1989;30:657-665.
4. Chambers JN, Oliver JE, Bjorling DE, et al. Update on ventral decompression for caudal cervical disk herniation in Doberman pinschers. J Am Anim Hosp Assoc 1986;22:775-778.
5. Seim HB, Withrow SJ. Pathophysiology and diagnosis of caudal cervical spondylomyelopathy with emphasis on the Doberman pinscher. J Am Anim Hosp Assoc 1982;18:241-251.
6. VanGundy TE. Disc-associated wobbler syndrome in the Doberman pinscher. Vet Clin North Am Small Anim Pract 1988;18:667-696.
7. Jeffery ND, McKee WM. Surgery for disc-associated wobbler syndrome in the dog—An examination of the controversy. J Small Anim Pract 2001;42:574-581.
8. Rusbridge C, Wheeler SJ, Torrington AM, et al. Comparison of two surgical techniques for the management of cervical spondylomyelopathy in Dobermans. J Small Anim Pract 1998;39:425-431.
9. Queen JP, Coughlan AR, May C, et al. Management of disc-associated wobbler syndrome with a partial slot fenestration and position screw technique. J Small Anim Pract 1998;39:131-136.
10. McKee WM, Butterworth SJ, Scott HW. Management of cervical spondylopathy-associated intervertebral disc protrusions using metal washers in 78 dogs. J Small Anim Pract 1999;40:465-472.
11. Dixon BC, Tomlinson JL, Kraus KH. Modified distraction-stabilization technique using an interbody polymethyl methacrylate plug in dogs with caudal cervical spondylomyelopathy. J Am Vet Med Assoc 1996;208:61-68.
12. De Risio L, Munana K, Murray M, et al. Dorsal laminectomy for caudal cervical spondylomyelopathy: Postoperative recovery and long-term follow-up in 20 dogs. Vet Surg 2002;31:418-427.
13. Chambers JN, Oliver JE Jr, Kornegay JN, et al. Ventral decompression for caudal cervical disk herniation in large- and giant-breed dogs. J Am Vet Med Assoc 1982;180:410-414.