The importance of taking a complete dermatologic history
And how to do it right-including a comprehensive downloadable client history form.
Taking a thorough patient history is fundamental in assessing patients with skin disease. The clinical signs, age of onset, duration, location and extent of pruritus, treatments already used, and many more factors are often valuable clues for diagnosis. Obtaining all of the necessary information is a time-consuming task that may seem impossible to accomplish in a brief office visit.
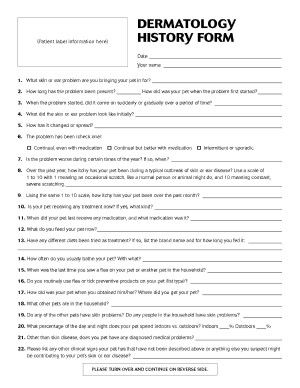
Using a dermatology history form is greatly helpful in this regard (
Major client complaint
Is it itching? Hair loss? Lesions? All of the above? Regardless of your overall findings, make sure to address the client's major concern.
Description of disease onset
When, where, and how did it start? Did the itch come first and then the lesions? Or was it the reverse? Or both at the same time?
• Parasites or infections can occur at any age. A young onset may favor allergy. An older onset may signify underlying systemic, metabolic, or autoimmune disease. Geriatric patients may lead you to consider skin neoplasia or a paraneoplastic syndrome.
• Itch first without lesions tends to favor allergic causes. Lesion appearance first or at the same time as itch tends to favor parasitic or infectious causes.
• Parasites or infections are typically a sudden onset, while allergic causes are usually gradual onset.
Description of skin disease progression
Be sure to note any changes with season or with medication. Seasonality may suggest environmental allergy, and a response (or lack of response) to prior treatments may provide clues.
Degree and location of pruritus
The distribution may be highly suggestive. For example, a dorsal lumbosacral focus can often be assumed to be flea allergy until proven otherwise, while pedal or pinnal pruritus is suggestive of environmental or food allergy. For dogs, some history forms may incorporate the Favrot criteria for clinical evidence of atopic dermatitis.1
Current and prior treatments and response
Be sure to ask about different diets that have been tried. Was a complete and proper hypoallergenic diet trial performed (i.e. with strict compliance and a veterinary therapeutic diet)?
Parasite history and current parasite control-or lack thereof
For pruritic skin disease in dogs and cats, instituting regular parasite control is a standard recommendation.
Evidence of contagion to other animals or people
Any evidence of contagion signals a parasite or dermatophyte infection.
Clinical signs the owner has observed
Be sure to assess the severity of the signs as well. Using a grid- or table-like form enables you to quickly scan down to see the signs that are “moderate” or “severe.”
Evidence of concurrent disease
Is there any suggestion of underlying disease? Gastrointestinal signs that may encourage consideration of food allergy as a cause?
Owner's thoughts on the cause of the disease
At the very least, you may be able to assure the owner of what is not causing the pet's illness, such as allergy to carpet fibers, perfumed laundry detergent, fabric softener sheets, or other urban myths.
Closing thoughts
The other big advantage of a history form is that you now have all the information for every patient all in the same location in the record. Months later, if you need to look back to see how the client rated the dog's pruritus or whether other diets were tried, you'll know exactly where to find the information.
Reference
1. Favrot C, Steffan J, Seewald W, et al. A prospective study on the clinical features of chronic canine atopic dermatitis and its diagnosis. Vet Dermatol 2010;21(1):23-31.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.