Injectable Robenacoxib for Pain Relief After Soft Tissue Surgery in Dogs
In a recent study, robenacoxib injected subcutaneously at a dosage of 2.0 mg/kg/day for 3 days controlled pain associated with soft tissue surgery in dogs.
The drug was also well tolerated, say the authors of the report, which was published last month in the Journal of Veterinary Internal Medicine.
Robenacoxib is a nonsteroidal anti-inflammatory drug (NSAID) that selectively inhibits cyclooxygenase-2. Its advantages for surgical procedures, say the authors, are its rapid onset of action, availability in both oral and injectable forms, and safety in healthy dogs.
Credit: 365vet.co.uk
In Europe, robenacoxib is registered for the treatment of surgery-associated pain in dogs. This prospective, randomized, multicenter, placebo-controlled, masked, parallel-group study was conducted in support of Food and Drug Administration approval of robenacoxib in the United States.
The trial included 317 client-owned dogs undergoing soft tissue surgical procedures at 12 veterinary clinics in the United States. Dogs included in the study were healthy dogs 6 months or older who weighed at least 2.5 kg and met none of the exclusion criteria (such as various illnesses, conditions that could interfere with pain assessments, and concurrent treatments that could affect pain scores).
All dogs received butorphanol 0.2 mg/kg IM or IV prior to anesthesia. The 159 dogs in the treatment group received robenacoxib 2 mg/kg SC at the time of anesthetic premedication and once a day for 2 days after the surgical procedure (a total of 3 injections given 24 hours apart). The 158 dogs in the control group received injections of a placebo rather than robenacoxib.
Dogs could receive rescue pain treatment or be withdrawn from the study at any time at the discretion of the attending veterinarian. The most common surgical procedures were removal of a dermal mass 8 cm or larger, ovariohysterectomy, gastropexy, and cystotomy. Anesthetic protocols varied (although all dogs received butorphanol premedication); most dogs received propofol for induction and isoflurane for maintenance anesthesia.
The study’s primary efficacy variable was treatment failure, defined as the need for rescue pain treatment or withdrawal from the trial because of adverse events likely related to treatment. Secondary efficacy variables were total and individual component scores on the short form of the Glasgow Composite Measure Pain Scale. Each dog received pain assessments prior to anesthesia, 4 times after surgery on the day of the procedure, and 3 times on the second and third days after the procedure (11 assessments for each dog).
Significantly more treatment successes occurred in the robenacoxib group (108 of 151 dogs, 73.7%) than in the placebo group (85 of 152 dogs, 58.1%). All of the treatment failures in the robenacoxib group and all but 2 of the treatment failures in the placebo group were due to administration of rescue pain therapy. Two treatment failures in the placebo group were due to adverse events.
The most common adverse events in both groups were pain on injection, diarrhea, and vomiting. The authors report that nearly all adverse events were mild. Mean serum chemistry, hematology, and urinalysis values were within reference ranges in both groups at the end of the study. Significant differences between groups included serum potassium levels, absolute lymphocytes, and absolute monocytes (higher in the robenacoxib group) and urine pH (higher in the placebo group), none of which the investigators considered clinically relevant.
Slightly over one-fourth of dogs receiving robenacoxib required rescue pain medication. Other studies have also indicated that NSAIDs alone are insufficient to control perioperative pain in some patients, note the authors. “Therefore, multimodal therapy is needed for optimal control of pain,” they write.
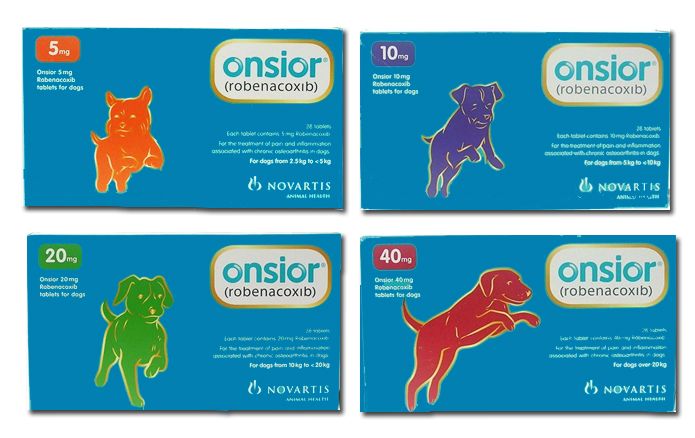
Elanco Animal Health Inc, the manufacturer of robenacoxib (Onsior), funded the study and employs all of the authors.
Dr. Laurie Anne Walden received her doctorate in veterinary medicine from North Carolina State University. After an internship in small animal medicine and surgery at Auburn University, she returned to North Carolina, where she has been in small animal primary care practice for over 20 years. Dr. Walden is also a board-certified editor in the life sciences and owner of Walden Medical Writing, LLC. She works as a full-time freelance medical writer and editor and continues to see patients a few days each month.
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen