Pain management for oral surgery in dogs and cats
After oral surgery, nociceptor response is expected to be greatly enhanced.
Pain from tissue insult involves a complicated array of physiologic and chemical changes that lead to perception in the brain.

Brett Beckman
Understanding the terminology and physiology and managing oral pain in our patients is the focus of this series.
This month, the concepts of nociception, peripheral sensitization and central sensitization will be discussed as they relate to patient management.
These mechanisms allow the practitioner to make analgesic choices for individual patients, taking into account the type, duration and severity of the pain. Consistent, reliable results can be obtained using pre-emptive and multimodal analgesia

The second part of the series will provide a detailed description of regional nerve blocks for oral surgery. The third will describe agents commonly used for analgesia. A discussion of chronic-and cancer-pain management and clinical use of constant-rate infusions will conclude the series.
Nociception
Nociception involves the processing of noxious stimuli, resulting in the brain's perception of pain (Figure 1). Transduction, transmission and modulation are the components.
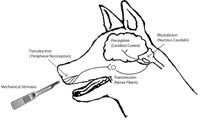
Figure 1: Transduction, transmission and modulation are components of nociception, the processing of noxious stimuli, which results in the brain's perception of pain.
The conversion of a noxious stimulus (mechanical, chemical or thermal) into electrical energy by a peripheral nociceptor or free afferent nerve ending is termed transduction. The propagation of the impulse from the site of oral injury through primarily trigeminal afferents is referred to as transmission. The nerve fibers responsible for sharp pain are the fast A-delta fibers. Dull, throbbing pain is caused by stimulation of slow C fibers. A-beta nerve fibers are tactile and consequently have a much lower threshold. Neurons from these fibers synapse with nociceptive-specific and wide-dynamic-range neurons in the medulla's nucleus caudalis, resulting in modulation. Nucleus caudalis tissue is very similar to that of the spinal cord dorsal horn that modulates pain from areas other than the oral cavity. Exitory neuropeptides, like glutamate and substance P, are active in the synapse and facilitate the pain signals by binding to their receptors on these neurons. Concurrently, endogenous (opioid, serotonergic and noradrenergic), descending analgesic systems serve to decrease the nociceptive response.
Peripheral sensitization
Following surgical manipulation of the oral cavity we can expect a greatly enhanced postoperative nociceptor response to any additional stimulation. The resulting enhanced response is termed peripheral sensitization (hyperalgesia).
Primary hyperalgesia is the term for peripheral hyperalgesia at the actual site of the injury. The damaged tissue releases a number of compounds, including ATP, potassium ions, hydrogen ions, prostaglandins, bradykinin and nerve growth-factors. Lymphocytes, monocytes, macrophages and mast cells are attracted to the site. These inflammatory cells then release cytokines that amplify and potentiate inflammation. Histamine is among the list of cytokines released that enhance vasodilation, causing plasma extravasation into surrounding tissues. As a result this "sensitizing soup" of substances extends beyond the actual site of tissue injury into the surrounding normal tissue, producing secondary hyperalgesia. Now even non-noxious stimuli, such as touch, can produce pain at and around the site of injury (allodynia).
Central sensitization
Left untreated, peripheral sensitization produces similar changes in the wide dynamic range neurons of the nucleus caudalis producing a state called central sensitization or "windup."
Numerous chemicals react to increase the sensitivity of these neurons, exaggerating the frequency and intensity of nociception. Glutamate is partly responsible, in that it acts to bind to the NMDA receptor on the wide dynamic range neuron, making it a primary substance involved in central hypersensitization (Figure 2).

Figure 2: Binding to the NMDA receptor on the wide-dynamic-range neuuron, glutamate becomes a primary substance involved in central hypersensitization.
Drugs that bind preferentially to the NMDA receptor in the nucleus caudalis can help us manage central sensitization associated with oral pain states. Traditional pain medications will not be effective for this component of chronic pain. NMDA antagonists and other analgesic agents will be covered in the third part of this series.
Pre-emptive analgesia
Pre-emptive analgesia is the administration of analgesics prior to a painful stimulus, to decrease the anticipated post-stimulus pain. Administering analgesics prior to inducing a painful stimulus is more effective than giving the same drug after the stimulus is induced. Once established, especially when central sensitization is involved, pain becomes very difficult to control, emphasizing the importance of providing pain management preoperatively.
Some common conditions of chronic severe oral pain, such as feline LPGS, refractory stomatitis in dogs and oral cancer, all should receive special attention in preoperative pain management. Failure to do so will make it likely that management will be very difficult post-operatively, requiring additional hospitalization, additional administration of injectable analgesics and feeding assistance. Figure 3 outlines the result of a pre-emptive analgesic given to prevent central and peripheral sensitization.

Figure 3: Preoperative pain management is recommended in some instances. This outlines the result of a pre-emptive analgesic given to prevent central sensitization.
Multimodal pain management is defined as use of two or more analgesics in combination to minimize or eliminate patient pain.
Often this approach allows the practitioner the luxury of decreasing the dose for each analgesic, making the combination safer than a higher dose of a single agent. Using different analgesics in this multi-modal manner allows clinicians to block pain in different portions of the pathway of nociception. Table 1 demonstrates the effect of different drug classes on transduction, transmission and modulation. As you can see, the local anesthetics block pain in all three nociceptive pathways.

Table 1. Drug classes affecting varying portions of the nociceptive pathway
Environmental comfort
Manipulation of the environment is important in providing maximal comfort for painful patients postoperatively. Monitoring patient temperature is particularly essential in oral surgery. All patients, but particularly small ones, are subject to cooling from the cool-water spray from ultrasonic and high-speed devices.
Intravenous fluids should be properly warmed and safe external warming devices utilized to maximize patient comfort and minimize intraoperative hypothermia. During recovery, warm towels and blankets should be used continually for comfortable padding. To decrease postoperative stress, consideration should be given to separating dogs and cats or even isolating individual patients. Noise should be minimized. Verbal and tactile interaction with patients can be comforting in some, whereas others recover better with passive observation. Soothing music also may be beneficial.
Brett Beckman, DVM, FAVD, Dipl. AVDC practices referral dentistry at Affiliated Veterinary Specialists, Orlando, Fla.; Noah's Animal Hospitals in Indianapolis; and at Florida Veterinary Dentistry and Oral Surgery in Punta Gorda, Fla. He is president-elect of the American Veterinary Dental Society and diplomate of the American Academy of Pain Management.
REFERENCES
- Tranquilli WJ, Grimm KA, Lamont LA. Pain Management for The Small Animal Practitioner, Jackson, Wyoming: Teton NewMedia, 2000; 6.
- Beckman, BW Pain Management for Oral Surgery in Dogs and Cats, J Vet Dent, March 2006 23(1): 50-60.
- Muir WW. Physiology and Pathophysiology of Pain. In: Gaynor JS, Muir W W. Handbook of Veterinary Pain Management. St. Louis: Mosby, 2002; 13-45.
- Hargreaves KM, Hutter JW. Endodontic Pharmacology. In: Cohen S, Burns RC: Pathways of The Pulp St. Louis: Mosby, 2002; 665-681.
- Tranquilli WJ, Grimm KA, Lamont LA. Pain Management for The Small Animal Practitioner, Jackson, Wyo.: Teton NewMedia, 2000; 10.