Pre-emptive pain management utilizing local and regional nerve blocks (Proceedings)
What is pain? Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. All potential and actual tissue damage in animals should be considered to cause pain. Pain can be experienced with or without accompanying signs of stress (e.g., tachycardia, hypertension). The first step in treating pain is to recognize the signs and symptoms.
What is pain? Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. All potential and actual tissue damage in animals should be considered to cause pain. Pain can be experienced with or without accompanying signs of stress (e.g., tachycardia, hypertension). The first step in treating pain is to recognize the signs and symptoms.
Pain commonly arises from activation of a physiological process that results in nociception. This process involves receptors and neural pathways that carry a noxious stimulus from transduction, transmission, modulation and perception.
Physiologically, pain is divided into two classifications, nociceptive or neuropathic. Nociceptive pain is further divided in tow two categories, somatic and visceral. Neuropathic pain is either central or peripheral, depending on the origin of the stimulus (i.e. direct damage to peripheral nerves or the spinal cord).
Peripheral nociceptors respond to noxious stimuli, the impulse is altered from physical energy to chemical (transduction), and is transmitted along peripheral neurons (transmission) to the dorsal horn of the spinal cord. Here the neurons synapse with neurons in the spinothalamic tract (modulation), which carry the impulse to the brain resulting in conscious recognition (perception) of pain.
Somatic pain, which in humans, has been described a localized, sharp, aching, or throbbing, originates from skin, connective tissue, muscle, joint and bone.
Visceral pain, described as dull or hard to localize, originate from receptors in the heart, lungs, kidneys, liver, gastrointestinal tract, uterus or bladder.
If pain is left untreated or under treated, animals can become depressed, lethargic, withdrawn, and eventually immobile. Early recognition and aggressive treatment is necessary to prevent these experiences. Patients being treated for pain during the perioperative period return to normal function sooner that those individuals who are left untreated.
Recognition of pain in veterinary patients is dependent on behavioral and physiologic responses. Behavioral signs of pain can very widely among patients. Some individuals and certain breeds are known for their stoic behavior while other patients seem to more readily present behavioral changes.
Physiological response to and consequences of pain are identical to those attributed to shock (sympathetic stimulation, atelectesis,, hypoxemia, vasospasm, localized tissue ischemia, decreased gut motility, increased myocardial oxygen consumption, increased metabolic rate, increased insulin resistance, sodium retention, decreased urine output, reduced socialization and increased anxiety.
Mild pain usually presents as a nuisance type pain that is easily tolerated and manipulation of the affected area may cause concern and adverse reaction on the part of the patient, but does not seem to be painful when not being stimulated.
Moderate pain is thought to be present when a patient has a disease or has undergone a surgical procedure that is known to cause pain in human patients.
Severe pain is such that a patient howls cries or screams unprovoked. Self mutilation may be seen, as may be violent thrashing around in the cage.
It may not be possible to totally eliminate all pain but rather the goal should be to reduce or eliminate the pathological pain.Nursing care can greatly improve the pain tolerance of most of our patients. Remember to clean all blood from the surgical area and if warranted, express the bladder of post-operative patients. Provide external heat sources to prevent hypothermia or to aid in active rewarming. This can be done by utilizing forced warm air blankets, circulating water pads or in-line fluid warmers if the patient is to be on IV fluids. Warm, dry bedding to cushion and support the patient will bring some relief. If possible, during the immediate re-emergency phase of anesthesia, a quiet room with dimmed lighting can reduce anxiety. The human touch is greatly reassuring to the majority of our patients.
While general anesthesia prevents the conscious perception of pain, it does not stop the nociception of pain during surgery. Pre-emptive analgesia reduces the input from the peripheral nerves during anesthesia and may reduce the amount of drug required to provide patient comfort in the post-operative area. Additionally, pre-emptive analgesics have been shown to be advantageous in being able to decrease the amount of inhalant anesthetic necessary to achieve surgical anesthesia.
Pharmacological intervention can be delivered in multiple routes of administration. As previously stated one can be pre-emptive and utilize local or regional blocks in addition to systemic administration. This mult-modal approach allows for a more balanced analgesia.
Local blocks are more effective if used prior to surgical stimulation. The local anesthesia decreases the intensity of postoperative pain. It is not always possible to provide local anesthetics prior to surgical stimulation but you can incorporate their use intra-operatively.
1. infiltration of a wound
a. nerve root stumps
b. wound edges
c. ear ablations
2. line blocks
3. intercostals neural blocks
4. intrapleural analgesia
5. brachial plexus blocks
6. Epidurals
Lidocaine has a rapid onset (5-10 minutes) and is of short duration (1-2 hours). The total dose should not exceed 4-7 mg/kg. Toxic effects can be seen with a dose of 11mg/kg. These side effects include: restlessness, muscle tremors, seizures, cardiopulmonary depression, coma and death.
Bupivicaine has a longer onset of action (20-30 minutes) and a longer duration of action (4-6 hours). The dose should not exceed 2.2 mg/kg. Toxic side effects can be seen with a dose of 4-5 mg/kg and are similar to those of Lidocaine.
Epidurals should not be administered to patients with pre-existing neurological dysfunction, coagulopathies, sepsis or affected skin areas involved with the epidural site.
COMPLICATIONS AND TOXICITY OF LOCAL ANESTHETIC AGENTS
• Local anesthetic overdose
• Intravascular administration
• Cardiovascular and central nervous system toxicity
• Toxicity is potency dependent
• CNS excitation or depression, unconsciousness
• Centrally mediated muscle contraction/seizures
• Respiratory center depression = apnea
Drugs used for epidurals
Epidural administration of local anesthetics, but not opioids, is contraindicated in those patients suffering from hypovolemia. Local anesthetic administration produces no or very mild sedation, minimal nausea and vomiting and occasionally urinary retention. Local anesthetic administration may produce a decreased heart rate, cardiac output and hypotension, but does not appear to impair the respiratory system. Opioid administration may cause marked sedation, nausea, vomiting urinary retention and or pruritis. At appropriate doses, it may also cause minimal change in heart rate, cardiac output, or blood pressure but may cause early and late respiratory depression. The respiratory depression can be antagonized. Total volume to be injected into the epidural space should not exceed 6 mls in the canine or 1.5mls in the feline patient.
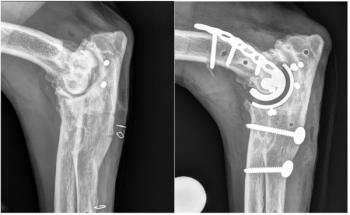
Brachial Plexus Block
This block is effective for procedures below the elbow as it will provide a block to the radial, median, musculcutaneous and axillary nerves. Indicated surgical procedures would include: carpal arthrodesis, digital amputation, mass removal distal to the elbow, stabilization of radial/ulnar fractures.
The shoulder area should be surgically clipped and prepped prior to proceeding. Grasp the forelimb firmly cranial to the elbow. The brachial artery may be palpated with the fingers to provide a landmark. The limb is gently rotated to facilitate palpation of the greater tubercle of the humerus, a 22 gauge, 2.5" spinal needle is inserted medially toward the costochrondral junction remaining parallel to the vertebral column. The stylet is removed from the spinal needle and the preloaded syringe with the calculated dose is firmly attached. Advance the needle distal to the palpated brachial artery in the area of the nerve bundle arising from T1 (Median, ulnar, musculocutaneous), aspirate and deliver ½ of the agent. Gently drag the needleback until the bevel is estimated to be proximal to the palpated brachial artery, aspirate and deliver the remaining ½ of the anesthetic agent in the area of the radial nerve. Some individuals prefer to start delivering the agent after passing the needle distal to the radial artery and to continue to infuse as the needle is withdrawn. The most common complications seen with this block would include inadvertant entrance into the thoracic cavity, accidental puncturing of the brachial artery which emphasizes the need to aspirate before injecting any agent, sensitivity to the agent used. There should be no known infected tissue in the area that will be approached.
Ring blocks for the distal forelimb
This block may also be referred to as the digital block and is probably most often used in veterinary practices for the onchectomy. The nerves affected are the median and palmar branch of the ulnar nerve, the dorsal branch of the ulnar nerve and the superficial radial nerve branches. This block will provide intra-operative and post-operative analgesia. The duration of the block will be dependent on the agent used. A combination of lidocaine and bupivicaine will provide a block with rapid onset and longer duration. Please see drug chart for epidurals for time of onset and legnth of duration for each agent. It is recommended that lidocaine without epinephrine be used for those blocks that potentially lack collateral circulation i.e. the digits to prevent any possible disruption of adequeate blood supply.
The median and palmar branches of the ulnar nerve are approached medially to the accessory carpal pad The dorsal branch of the ulnar nerve is approached latral and proximal to the accessory carpal pad. The superficial radial nerve branches are approached at the dorso-medial aspect of the proximal carpus.
The feet should be prepped with an antiseptic agent, either povidine or chlorhexidine. If laser eqipment is to be used for the procedure, NEVER use alcolhol due to the risk of fire. The calculated dose of agent(s) may be combined in a 3cc syringe equiped with a 25ga needle. If the volume is extremely small, the dose may be diluted using 0.9% sodium chloride to facilitate delivery. After prepping the foot (feet), identify the landmarks and aseptically introduce the needle to the location, always aspirating prior to injection. Typically a volume of 0.1 – 0.3ml is injected into each site. The needle and syringe whould be fairly parallel to the limb during injection and the agent delivered into the subcuatneous tissue.
Five Types of Dental blocks:
1. Local Infiltration: This method can be employed when only a small area requires anesthesia. The anesthetic agent can be injected into the gingiva, mucosa or periodontal ligament. When radiographs show bone loss around a specific tooth, a local anesthetic agent can be infiltrated apical to that tooth. Also, as an adjunct to an infraorbital block, the maxillary teeth can be blocked by infiltration palatal to that specific tooth.
2. Infraorbital Nerve Block: The infraorbital foramen is easily palpated in the dog and cat. It can be found apical to the maxillary third premolar. Through this foramen passes several nerves that supply innervation to the maxillary arcade. Insert the needle through the buccal mucosa where it forms a crease and direct it towards the foramen in a rostrocaudal direction. Pass the needle until it is at the opening of the foramen. Aspirate in several planes. Slowly inject the agent in an attempt to bathe the exiting nerves supplying the rostral structures. When the more caudal teeth are to be blocked, finger pressure is held over the wheal of local to "force" the agent deeper into the foramen, thus blocking those structures.
Other sources recommend actually passing the needle just inside the foramen and instilling agent to block rostral structures and then advancing the needle gently into the foramen to instill more through the foramen (aspirating frequently). Digital pressure is used to prevent the local agent from then exiting from the foramen.
3. Maxillary Nerve Block: This is performed to block the palatal tissue and bone in the maxilla. Visualize the midline of the palate. Then visualize the palatal root of the upper fourth premolar. Draw an imaginary line from that root perpendicular to the midline. Half way across that perpendicular line is the opening of the major palantine foramen. The needle is inserted in a dorsocaudal direction, but very parallel to the palate. Great care should be taken not to enter this foramen. The palate is rather firm tissue. It is safest to aspirate, then inject a bleb of local into the palatal tissue until you see it blanche. At that point, use digital pressure for 1 minute to "force" the agent around the nerves exiting this foramen.
4. Mandibular Block: When attempting to block the mandibular structures, the mandibular nerve needs to be blocked. There are two ways to accomplish this. To block this nerve intraorally, slide your index finger along the mandible caudal to the last molar until you feel an indentation. With the other hand, introduce the syringe until the needle is at the opening of the foramen. Aspirate then inject.
5. Mental Block: There are three mental foramina. The middle mental foramen is the largest. In large dogs this can be palpated apically between the first and second premolars. The needle is inserted under the submucosa just to the entrance of the foramen. Aspirate and inject. If the interest is in blocking the rostral mandibular structures put a minute's worth of finger pressure to ensure the agent anesthetizes the incisors and canine.In the cat, the needle is introduced through the submucosa into the labial frenulum and directed caudally. Aspirate and inject.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.