Stabilizing companion birds in an emergency
Avian medicine in the United States and abroad tends to be more focused on crisis and intervention than on preventive care and wellness. Therefore, in this article I discuss some of the basic considerations of emergency medical care in pet birds.
Avian medicine in the United States and abroad tends to be more focused on crisis and intervention than on preventive care and wellness. Therefore, in this article I discuss some of the basic considerations of emergency medical care in pet birds. I focus on initially stabilizing such patients to allow referral or follow-up for diagnostics and treatment. However, your role is not only to initially treat these birds but also to help guide clients toward information on what can be done at home to prevent further emergencies and to encourage clients to seek wellness care to enhance their birds' quality of life.
FACTORS CONTRIBUTING TO EMERGENCY VISITS
Even though a pet bird's position in the typical home has changed dramatically over the past three decades—from a caged bird to a true family member—preventive health measures have not kept up with the increase in the public's perceived value of pet birds. For example:
- Most pet birds still receive virtually no veterinary medical care during their lives.1
- Many birds that do receive medical care only receive emergency or crisis-intervention veterinary care.
- Wellness care—including behavior counseling, annual examinations, and environmental and husbandry improvements—remains the exception to the rule in the average small-animal practice that provides avian care. Many veterinary practices that provide avian care do not send reminders for annual examinations. Those that do implement a wellness-based reminder system often quote an appallingly low percentage of compliance with return visits, strongly suggesting that true wellness practice is not occurring, as compared with companion canine medicine.
- The general public still often regards the role of an avian veterinarian as one of diagnosing and treating disease rather than maintaining and enhancing the wellness and quality of life of pet birds.
- Birds often enter the pet trade less-than-ideally positioned for a normal life expectancy. Unweaned birds may go to naïve buyers, birds may be habituated to eating a seed-based diet, birds often have not been socialized and prepared for existence as companion birds, birds may be clinically or subclinically afflicted with infectious diseases, and erroneous husbandry or even medical advice may be provided to the purchasers.
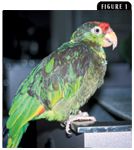
Figure 1. This Amazon parrot was presented for evaluation of acute anorexia. The diagnosis was advanced obesity due to chronic malnutrition, hepatic lipidosis, and dehydration. Supportive care with parenteral fluids followed by dietary management, including conversion to a formulated diet and weight reduction, and better integration of the bird into the owners daily activities resulted in an excellent outcome.
Considering these points, it can be concluded that inadequate home care can contribute to or exacerbate emergencies (Figures 1, 2, 3A, & 3B). For example, chronically malnourished birds (fed long-standing inappropriate seed-based diets), regardless of their emergency, may carry a poorer prognosis for survival simply because of their already declining condition. So the clinical picture may be more complicated than it initially seems.

Figure 2. Not all emergency presentations require immediate definitive treatment. This Goffin's cockatoo was presented for evaluation of an acute rhinitis. Emergency personnel supported the bird with subcutaneous fluids, kept it overnight for observation, and referred it for diagnosis. The definitive diagnosis was Aspergillus species sinusitis. Hypovitaminosis A and inappropriate husbandry most likely predisposed the bird to infection.
All of these challenges illustrate the importance of properly caring for birds when they are brought to your clinic for an emergency, as well as proper follow-up. Follow-up care becomes much more of a necessity compared with that needed in mammalian emergencies. Many of these avian patients, when stabilized, will require extensive follow-up evaluation to complete the diagnostic picture, correct any husbandry deficits, improve the birds' nutritional status, and implement other actions to avoid future crises.


Figure 3A. & 3B. The excessively short clipped wings of this young Umbrella cockatoo (3A) were likely responsible for its uncontrolled fall, which resulted in the split skin of the ventral tail base (3B). Unfortunately, these types of wing-clip-associated injuries are common. The wound was surgically repaired, but the follow-up was key in the ultimate resolution and prevention of the problem. The bird was trained to perch only on the hand, where a fall was easiest to prevent, and owners were made aware of the risks associated with excessive wing clipping. The bird began its juvenile molt at about 10 months of age and ultimately replaced all of those feathers successfully.
EMERGENCY CARE PRINCIPLES
As in any emergency, the ABCs—airway, breathing, and circulation—must be addressed in pet birds before you initiate diagnostic testing and further treatment. Samples for pretreatment laboratory tests may be collected in many cases, but in most emergency situations, stabilization is the primary goal. Although radiography may be helpful in some cases, in inexperienced hands, an effort to obtain a detailed radiographic diagnosis can sometimes be as life-threatening as the patient's medical condition. Take time to learn proper avian handling and restraint techniques before you're faced with an emergency. Avoid causing excessive fear, pain, or discomfort and be efficient with your technique. Frequently, a towel is used to help restrain companion birds, but this is not mandatory. Avoid, if possible, pouncing on your patient, similar to the way a predator may attack, and try to be respectful of the patient's instinctual predator or prey behavioral differences.
Airway
Quickly assess the adequacy and pattern of respiration, and auscultate the chest and air sacs. If a bird is not breathing adequately, place an endotracheal tube. The glottis of birds, located at the base of the tongue, is not covered by an epiglottis. This anatomical feature makes endotracheal intubation much easier than in mammalian patients of similar size. Hold the beak open and pull the tongue rostrally to easily see the glottis. Most of the common pet bird species have complete tracheal rings, so be careful when inflating the cuff of an endotracheal tube or use an uncuffed endotracheal tube.
To bypass the trachea in patients with a tracheal obstruction, cannulate the abdominal or caudal thoracic air sacs. Place the bird in right (preferred) or left lateral recumbency, incise the skin caudal to the last rib, and use a curved or right-angled hemostat to penetrate the body wall. Choose a tube that is nearly equal to the size of the trachea, and place the tube through the hemostat jaws and into the caudal thoracic or abdominal air sac. Cut the tube to a comfortable length for the bird, and then tape and suture it into place just as you would suture a tomcat catheter. Ventilate intubated birds with slow, deep respirations (10 to 20 breaths/min for birds weighing less than 100 g [3.5 oz]). 2
Breathing
If airway patency is adequate, observe the rate, depth, and quality of respiration. Rapid, shallow respirations may be due to pain from rib trauma. Birds with head trauma may have slow, shallow respirations. Hypoventilation commonly occurs with hypovolemic shock and acid-base disturbances. A tail bob is commonly observed when there is a marked abdominal component to expiration, often seen with pulmonary disease or obstructive tracheal disease. If the patient is conscious and breathing, oxygen may be delivered through a face mask or by placing the bird in an oxygen-rich environment.
Circulation
Assess an avian patient's cardiovascular status in a manner similar to that used in mammals. Evaluate mucous membrane color by observing the conjunctiva, the everted cloaca, or the choanal slit. Common clinical signs of hypoperfusion and diminished cardiac output include weakness, depression, pale mucous membranes, prolonged basilic vein (located along the ventral aspect of the elbow) refill time, tachycardia, and weak pulses. In the event of cardiac arrest, cardiopulmonary resuscitation may be attempted, but the success of cardiopulmonary resuscitation in birds is generally poor in most emergency situations. To perform cardiopulmonary resuscitation, place an endotracheal or air sac breathing tube, administer positive-pressure ventilation, and give an intramuscular injection of doxapram (0.2 ml for a large bird and 0.1 ml for a small bird).3 If the heart is not beating, perform 60 to 80 sternum compressions per minute.3 Epinephrine and atropine can be given intravenously, intraosseously, or endotracheally.3

Relieving pain in companion birds
Fluid replacement therapy is essential in birds with signs of hypoperfusion or hypovolemic shock. Fluids may be administered through an intravenous or intraosseous catheter or subcutaneously. Corticosteroid use in birds is, at best, controversial; it is contraindicated in many cases. There are many concerns about immunosuppression and suppression of the hypothalamic-pituitary-adrenal system in birds, so consider the side effects of glucocorticoid use to be at least as frequent and severe in birds as they are in mammals, if not more.4
Intravenous catheters may be placed in the jugular vein, the basilic vein, or the medial metatarsal vein. Intraosseous catheters may be placed in the proximal tibiotarsus or distal ulna. The humerus and femur are not acceptable sites for intraosseous fluid administration because they are pneumatic and connect to the bird's respiratory system. Keep in mind that receiving intraosseous fluids is most likely quite painful in birds, as it is in people. A slow fluid infusion rate of intraosseous fluids may help defray discomfort. In addition, consider initial intraosseous catheter and fluid bolus administration in a patient that is already anesthetized.
The most popular site for subcutaneous fluid administration is the inguinal region, but the interclavicular space and propatagial web sites can also be used. These sites have much more limited volume capacity for fluid compared with the inguinal region. If fluid pools in the ventral abdominal area, discontinue subcutaneous fluid therapy.
Initially, fluids may be infused at a rate of up to 1 blood volume of fluid over one hour. Lactated Ringer's and normal saline solution are common choices for fluid administration in birds. The total blood volume in birds ranges from 6% to 11% of body weight,5 with 8% to 10% used as an average in psittacines. Therefore, an initial intravenous infusion rate of up to 90 ml/kg/hr has been suggested for birds with suspected hypovolemic shock.6 Closely monitor birds for signs of overhydration or fluid extravasation. As perfusion improves, adjust the infusion rate until a maintenance rate of 10 ml/kg/hr is reached.6 Subcutaneous fluids can be given at a rate of 50 to 100 ml/kg and can be delivered into multiple sites as needed.
COMMON EMERGENCY PRESENTATIONS
Once the patient is stabilized, you can initiate additional treatment (Table 1). Some common problems you may face are hemorrhaging, lacerations, bite wounds, fractures, seizures, and hypothermia or hyperthermia.

Table 1. Possible Contributing Factors in Common Bird Emergencies
Hemorrhaging
Hemorrhage resulting from traumatic injury may quickly become life-threatening. Although birds can tolerate substantial blood loss over longer periods of time and appear to be more tolerant of acute blood loss compared with other companion animals, the loss of 20% to 25% of the total blood volume in a few moments can be fatal.7 The total blood volume in birds is generally estimated to be about 10% of their body weight. Common causes of potentially lethal hemorrhage include lacerations, long bone fractures, contusions in the region of the pectoral muscles, and beak fractures.
Contrary to a long-held belief, broken pinfeathers or toenails in healthy birds rarely result in fatal hemorrhage. However, broken pinfeathers or toenails in subclinically ill or malnourished birds have a greater potential for continued bleeding. Hemorrhage from toenails and beaks may be controlled with chemical or electric cautery. Do not use chemical cautery agents in soft tissue wounds, including pinfeathers, as these substances may cause severe tissue irritation and necrosis.
As mentioned above, birds appear to be more tolerant of acute blood loss than mammals are. After hemorrhage, baroreceptor and catecholamine-induced arteriolar vasoconstriction appear to rapidly shift extracellular fluid to the vascular space.5 Birds also appear to rapidly mobilize large numbers of immature red blood cells and lack many autonomic responses to hemorrhage that contribute to shock.8,9 According to one report, healthy birds seem to be able to lose as much as 30% of their blood volume (3% body weight) without any deleterious effects.10 In one study in pigeons, blood removal of up to 9% of body weight (equal to 90% of blood volume) was performed before significant mortality occurred.11 In another study, pigeons that lost 70% of blood volume had a normal packed cell volume within six days.12
One study indicates that transfusions may be of limited benefit in treating birds with acute blood loss. Raptors transfused with heterologous pigeon red blood cells had a red blood cell survival time of only 12 hours, and homologous transfusions of pigeon red blood cells into other pigeons had a survival time of only 7.1 days.13 In this study, pigeons losing 70% of their blood volume recovered from anemia after receiving fluid replacement with lactated Ringer's solution as quickly as or more rapidly than did birds receiving heterologous or homologous blood transfusions. This study suggests that, if needed, a homologous transfusion from the same species of bird would be most appropriate. Volume replacement with colloid or crystalloid solutions appears to be sufficient in treating many cases of acute blood loss. Using products such as polymerized bovine hemoglobin solution (Oxyglobin—Biopure) may also be helpful in avian patients with severe and acute blood loss.14
Lacerations
Lacerations may usually be sutured closed if the patient is presented within six to 12 hours after injury. Older wounds may require more cleaning and débridement before closure. Most lacerations should be repaired while the patient is anesthetized. Pluck, clean, and débride the area, and prepare the smallest surgical site possible to minimize heat loss. Most of the common products used for wound care in domestic mammals can be used in birds. Popular products include chlorhexidine or dilute povidone-iodine. Carefully maintain thermal support while cleaning and repairing lacerations, as hypothermia is easy to induce in an anesthetized and wet patient. Use taper needles and small suture materials (3-0 to 6-0). Polydioxanone (PDS) is commonly used for wound closure, as a recent study has demonstrated that it provides strong closure with the least amount of tissue reaction.15 I and many other clinicians use polyglactin 910 (Vicryl) for skin sutures. In my experience, antibacterial treatment of lacerations in many avian species seems to be required less often than in dogs or cats with similar lacerations.
Bite wounds
Predatory pets, such as cats or dogs, may inflict serious wounds that can lead to sepsis. Attacks by other pet birds in the household can also be severe. Patients with respiratory compromise, shock, severe hemorrhage, or alterations in neurologic status require immediate attention. If a wound is known or suspected to be caused by a bite from a mammalian predator (cat, dog, raccoon), administer a broad-spectrum antibiotic as soon as possible and continue it for seven to 14 days. Many potentially pathogenic oral bacteria, especially Pasteurella multocida, contaminate wounds. Death due to septicemia may occur within 24 hours if appropriate antibiotic therapy is not initiated.16 Birds without skin wounds have also been known to develop Pasteurella species septicemia by grooming their feathers after contact with cat saliva. The choice of antibiotic and route of administration should be based on the organism suspected to be involved. Dosages can be found in exotic-animal formularies.17
Fractures
Most avian long bones are covered by a small amount of skeletal muscle. When fractures occur, sharp bone edges often lie just below the skin surface. This predisposes birds to a greater risk of open fractures or more serious soft tissue injury than may be encountered in dogs or cats. In addition, fracture ends are often near large vessels or nerves. For these reasons, it is imperative to stabilize these fractures with some form of external fixation as soon as possible. Fractures requiring open reduction should be temporarily splinted until surgery can be done. Many fractures in pet birds, however, are amenable to closed reduction and external fixation. Anesthesia with isoflurane is necessary during reduction and stabilization. Try to stabilize the fractures with the lightest and most comfortable type of bandage or splint.
Fractures of the wing distal to the elbow may be immobilized by using a simple figure-of-eight bandage or wing wrap. Fractures of the humerus, coracoid, clavicle, or scapula may be immobilized or supported by using a combination of a figure-of-eight wing wrap and a wing-to-body wrap. Fractures of the pelvic limb distal to the femur may be immobilized by using an Altman tape splint. (To create this splint, apply multiple layers of white tape cranially to caudally across the fracture from the proximal tibiotarsal region across the ankle to the tarsometatarsal area.) Femoral fractures are more difficult to manage with bandages or splints because of the proximity of the body wall.18,19 If a bird has a femoral fracture, immobilize the bird with a leg-to-body wrap, and promptly refer it for surgical stabilization.
Surgical fracture repair techniques are beyond the scope of this article. In general, light-weight and comfortable fixation is accomplished by using positive profile pins because of the comparatively thin and more brittle nature of the cortices of bird bones.
Seizures
The most commonly documented seizure disorder in birds is heavy metal toxicosis (lead, zinc). Suspect this condition in a well-muscled patient that presents with a history of an acute onset of seizures. Treatment generally includes parenteral fluids, edetate calcium disodium (CaEDTA) (10 to 40 mg/kg intramuscularly b.i.d.), and possibly diazepam (0.5 to 1 mg/kg intramuscularly). Seizures in a patient that is markedly underweight or has signs suggestive of other conditions may be more likely related to progressing health problems. In such patients, supportive care and prompt referral for diagnostics and treatment may be more appropriate.
Hypothermia or hyperthermia
Birds are generally efficient homeotherms. Normal core body temperatures are around 105 F (40.5 C). In an emergency situation, however, heat loss is often exacerbated in birds, particularly those that are in shock, very ill, or undergoing treatment for trauma with administration of fluids, oxygen, or general anesthesia. Most trauma patients should be maintained in environmental temperatures of 80 to 90 F (26.6 to 32.2 C). Monitor birds closely for signs of hyperthermia, such as panting and holding the wings away from the body, and adjust the temperature as needed. Humidify the environment to limit fluid losses. House traumatized birds in a darkened, quiet area during recovery.
Exceptions to these general warmth recommendations include birds with marked abdominal distention, obesity, or severe respiratory distress. When heated excessively, obese birds are less able to cool themselves normally and more vulnerable to hyperthermia. Birds with marked abdominal distention or respiratory disease may be unable to achieve evaporative cooling through the respiratory tract.
NUTRITION
An important component of supportive care is nutritional support. Most birds that have not been eating well and are losing pectoral muscle mass should be tube fed or receive other nutritional support. Common tube feeding diets include commercial hand-feeding formula and other critical care diets. Consider adding dextrose or hetastarch to intravenous or intraosseous fluids, particularly in smaller patients. Patients that have marked gastrointestinal stasis or severe respiratory distress should not receive nutritional support through gavage feeding. A primary focus on initial stabilization, other supportive care, and prompt referral for diagnostics and treatment will often be indicated.
Offer a variety of foods to an ill bird in a calm setting, and allow it to eat on its own before force-feeding. If the hospital environment that the bird is kept in is maintained somewhat lit through the night, many birds will eat on their own overnight. Offer food at the same level the bird is perched at. Birds that can see and have easy access to their food will be more likely to eat. However, not all birds should have a perch available, depending on their physical strength and clinical condition.
FOLLOW-UP
Regardless of the diagnosis and treatment, most avian emergency patients should be referred to a primary care provider sooner than mammal emergency patients. Because of the interwoven nature of the avian emergency presentation and the potential primary causes involved, a controlled system of follow-up in most cases will effectively resolve the problem, prevent its recurrence, and improve the patient's quality of life.
If a patient dies or is euthanized, it is more common to recommend and perform a postmortem examination in avian practice than in small-animal practice. For this reason, most experienced avian practitioners request that the emergency clinician hold the body, refrigerated, pending the recommendation of the primary care veterinarian for the client. Necropsy is often warranted because of contagious disease concerns and the risk to other companion birds in the home, needed changes or improvement in husbandry, or zoonotic risks to the owners.
Brian L. Speer, DVM, DABVP (avian practice), DECAMS
Medical Center for Birds
3805 Main St.
Oakley, CA 94561
REFERENCES
1. US Census Bureau. Statistical abstract of the United States. Released Feb 11, 2003.
2. Sinn LC. Anesthesiology. In: Ritchie BW, Harrison GJ, Harrison LR, eds. Avian medicine: principles and application. Lake Worth, Fla: Wingers Publishing, 1994;1066-1080.
3. Lichtenberger M. Emergency care of birds, in Proceedings. Western Veterinary Conference 2002.
4. Westerhof I, Van den Brom WE, Mol JA, et al. Sensitivity of the hypothalamic-pituitary-adrenal system of pigeons (Columba livia domestica) to suppression by dexamethasone, cortisol, and prednisolone. Avian Dis 1994;38:435-445.
5. Sturkie PD. Heart and circulation: anatomy, hemodynamics, blood pressure, blood flow. In: Sturkie PD, ed. Avian physiology. New York: Springer-Verlag, 2000;154-190.
6. Quesenberry KE, Hillyer EV. Supportive care and emergency therapy. In: Ritchie BW, Harrison GJ, Harrison LR, eds. Avian medicine: principles and application. Lake Worth, Fla: Wingers Publishing, 1994;382-416.
7. Jenkins JR. Avian critical care and emergency medicine. In: Altman RB, Clubb SL, Dorrestein GM, et al, eds. Avian medicine and surgery. Philadelphia, Pa: WB Saunders Co, 1997;839-863.
8. Gildersleeve RP, Galvin MJ, Thaxton LP, et al. Hematological response of Japanese quail to acute hemorrhagic stress. Comp Biochem Physiol A 1985;81:403-409.
9. Natt MP, Herrick CA. The effects of cecal coccidiosis on blood cells of the domestic fowl. Poult Sci 1955;34:1100-1105.
10. Murray MJ. Management of the avian trauma case. Semin Avian Exot Pet Med 1994;3:200-209.
11. Kovach AGB, Szasz E, Pilmayer N: Mortality of various avian and mammalian species following blood loss. Acta Physiol Acad Sci Hung 1969;35:109-116.
12. Bos JH, Todd B, Tell LA, et al. Treatment of anemic birds with iron dextran therapy: homologous and heterologous blood transfusions, in Proceedings. Assoc Avian Vet 1990;221-225.
13. Sandmeier P, Stauber EM, Wardrop KJ, et al. Survival of pigeon red blood cells after transfusion into selected raptors. J Am Vet Med Assoc 1994;204:427-429.
14. Lichtenberger M. Transfusion medicine in exotic pets. Clin Tech Small Anim Pract 2004;19:88-95.
15. Bennett RA, Yaeger MJ, Trapp A, et al. Histologic evaluation of the tissue reaction to five suture materials on the body wall of rock doves (Columba liva). J Avian Med Surg 1997;11:175-182.
16. McCluggage DM. Surgery of the integument, selected topics. Semin Avian Exot Pet Med 1993;2:76-82.
17. Carpenter J, ed. Exotic animal formulary. Philadelphia, Pa: WB Saunders Co, 2004.
18. Degernes LA. Trauma medicine. In: Ritchie BW, Harrison GJ, Harrison LR, eds. Avian medicine: principles and application. Lake Worth, Fla: Wingers Publishing, 1994;418-433.
19. Bennett RA. Orthopedic surgery. In: Altman RB, Clubb SL, Dorrestein GM, et al, eds. Avian medicine and surgery. Philadelphia, Pa: WB Saunders Co, 1997;733-766.