Stem-cell therapy shows promise for horse soft-tissue injury, disease
While interest and controversy swirl around stem-cell use for treating human spinal-chord injuries and diseases ranging from diabetes to Parkinson's, veterinary medicine has been investigating stem-cell use for a variety of animal conditions and diseases.
While interest and controversy swirl around stem-cell use for treating human spinal-chord injuries and diseases ranging from diabetes to Parkinson's, veterinary medicine has been investigating stem-cell use for a variety of animal conditions and diseases.
Before and after: A torn inferior check ligament is traced between November 2007 (left) and eight weeks later in January 2008 to show improvement after treatment with adipose-derived stem cells.
One intriguing possibility is stem-cell therapy for soft-tissue (tendon and ligament) injury and joint disease in horses and dogs.
"Stem cells hold tremendous promise for the treatment of tendonitis and joint repair," says Lisa Fortier, DVM, PhD, Dipl. ACVS, associate professor of large-animal surgery at Cornell University's School of Veterinary Medicine.
Others agree, including Jose Garcia-Lopez, VMD, DMS, Dipl. ACVS, who has been using stem-cell therapy to treat soft-tissue injuries for about two and a half years at the Cummings School of Veterinary Medicine at Tufts University in North Grafton, Mass.
Also familiar with the therapy is Wes Sutter, DVM, Dipl. ACVS, at Ocala Equine Hospital in Ocala, Fla.
"For about seven years I've been treating tendon and ligament injuries with platelet-rich plasma (PRP). From a clinical standpoint the results have been encouraging. However, horses with significant scarring or chronic injuries do not appear to respond as well as do the acute anechoic lesions," Sutter says.
"Basically the big change that I've made in the past year and a half is that I'm adding stem cells to the PRP. This provides sort of the healing trinity — a provisional matrix from the fibrin in the PRP, growth-factor release from the activated platelets and progenitor or trophic cells to support quality fibroplasia and hopefully remodeling of the abnormal tissue."
Stem cells are undifferentiated cells capable of self-renewal through replication and differentiation into specific cell lineages. There are two broad categories of stem cells — embryonic and adult-derived.
Embryonic (ES) cells formerly were derived from Day-8, pre-implanted blasto-cysts. Recently, however, scientists have learned how to insert key genes into adult cells, effectively "turning" them into embryonic stem cells. No embryo is generated or destroyed, thereby avoiding the previous ethical controversy over embryonic stem cells. Significant scientific hurdles remain, though, before these cells can be used clinically.
Adult-derived mesenchymal stem cells (MSC) can be obtained from a variety of tissues, including bone marrow, adipose tissue, muscle, cartilage, trabecular bone and tendon. And there are hematopoetic stem cells (HSC) derived from bone marrow, capable of forming all types of blood cells.
The interest in stem cells centers on their potential to differentiate into a variety of cell types, including those of tendons and joints.
The challenge for veterinary medicine is determining which stem-cell types are best suited and most valuable to treat horse injuries and disease.
Cells dervived from fat vs. bone marrow
Three techniques are available for treating tendon and ligament injuries with MSCs, according to Fortier. One involves using mixed cells from adipose tissue, and the others make use of cultured cells from bone marrow or a centrifugation technique to concentrate bone-marrow stem cells.
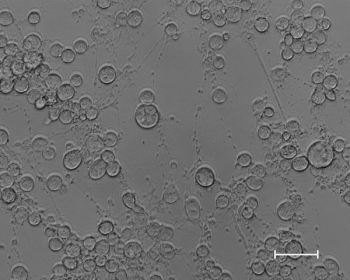
"You tend to get more nucleated cells from adipose tissue, so that might be one advantage, but what those cells are we don't really know," Fortier says.
"Literature suggests that if you compare cells from fat and from bone marrow side by side, only looking at differentiation of the cartilage and bone (for tendon, we don't really know), fat loses every time," Fortier says.
While acknowledging that "there is controversy in the literature," Bob Harman, DVM, MPVM and CEO of Vet-Stem Inc., of Poway, Calif., says "an equal number of papers show that stem cells from adipose and bone marrow are equal in characteristics, including differentiation ability into bone, cartilage, fat and other cell types." Vet-Stem provides a concentrated form of autologous, adipose-derived adult stem and regenerative cells to practitioners, to treat traumatic and degenerative diseases.
"The reason we don't have the same information for tendon is that there are very few ways to mimic tendon development in the laboratory, in contrast to the established ways we have to investigate development of new cartilage and bone," Fortier says. "The superior cell type will come out within the next four to five years, when people have enough cases and clinically evaluate their results."
Adipose-derived stem-cell therapy of the suspensory ligament injury in the horse showed a 76.6 percent return to prior level of performance, according to a study by Harman and colleagues.
"I have not used many marrow-derived stem cells, but do use adipose-derived cells, mostly in conjunction with platelet-rich plasma," says Lane Easter, DVM, Dipl. ACVS, with Performance Equine Associates in Whitesboro, Texas.
Platelet-rich plasma is thought to serve as a matrix for the stem cells to grow, and to add some growth factors. The jury is still out on what growth factors actually do for stem cells and which growth factors are associated with different types of platelet-rich plasma.
"The growth factors we get may not be the exact ones we need to turn that particular stem cell into whatever tissue we're trying to grow," says Easter.
"The most promising type of cells in my view are those from bone marrow, the sternally derived stem cells," says John Peroni, DVM, MS, Dipl. ACVS, at the University of Georgia College of Veterinary Medicine.
"I don't have any proof that they are better than the adipose-derived cells, so more work needs to be done to compare scientifically the pros and cons of these two cell types. Evidence would suggest that the origin of the cells plays a role in their pluripotent properties and it is possible that we will understand that the different cell types have different benefits and applications."
"We use the adipose-derived stem cells," says Garcia-Lopez. "In part, because of the ease of collection of the fat and the ease of turnaround, and there are more potential stem cells in fat than in bone marrow, so we don't have to do the culturing, as the group at Cornell does."
Biology/physiology of stem-cell therapy
"While provocative, studies documenting cellular transdifferentiation, i.e., the ability of adult stem cells from one tissue type to form specialized cell types of other tissues, should be carefully reviewed and regarded with some skepticism. Very few of these studies demonstrate functionality of the terminally differentiated cell type," Fortier cautions.
"There is considerable data regarding cartilage-tissue engineering and some data on tendon regenerative studies. What is lacking is information on characterization of the cells prior to implantation, and data on survival or function of the transplanted/grafted cells," Fortier says.
"The most controversy is over what these (injected) stem cells are doing," Garcia-Lopez says. "One of the things I suspect is happening ... is activation of the neighboring cells. That's a hugely debated part of it. We are not really sure whether these (injected) cells are already differentiated tissue. We think ... you probably have an activation phenomenon. Some of the cells within that tissue, whether bone, tendon or ligament, likely create more of their own cells, with the assistance of the growth factors injected with the stem cells."
"One of the areas we are interested in is trying to understand whether stem cells injected into tissues actually remain in those tissues and can be traced," Peroni says. "So if one can follow them through time and verify that they're not removed and not destroyed by the local environment of the wound, etc., it would make you believe they are actually doing something. It would be disappointing if we were not able to find a trace (of them) once they are injected in a tissue."
To trace what happens to the stem cells, Peroni and his group are doing preliminary work with "markers" — specific protein-expressing genes placed within the cells so that researchers later can observe whether the proteins are expressed in the tissues.
Bone-producing proteins are of particular interest. These are thought to be useful to expedite new bone formation — for fracture healing and joint fusion, for instance.
"I've used them with pretty decent luck on horses that have required joint-fusion procedures, such as cases of advanced osteoarthritis of the small hock joints," Peroni says.
The lower joints of the hock often are affected by arthritis that is unresponsive to traditional treatment. "One of the things they do for those horses is surgically fuse those joints by arthrodesis. In horses we treated recently with the addition of stem cells, we were impressed with the amount of bone turnover," Peroni says.
Researchers also are exploring the use of other markers, such as fluorescent dyes, to follow cell activity.
The University of Georgia researchers are interested in tracing marked cells during laminitis treatment, but there's a problem with that, Peroni says.
"The problem is that there is no practical way to put stem cells in laminar tissue because it is trapped between the hoof capsule and the coffin bone; we don't have direct access to it," he explains.
"They're trying to take advantage of a feature of MSCs called patho-tropism," Peroni says. "These cells apparently can hone in to a site of injury. If so, it would be interesting to be able to administer the cells to the horse essentially rather than to the foot and watch them target the specific area of injury. It's a bit of a long shot but something that we're trying to explore," Peroni says.
Stem-cell therapy for tendon injury
After tendon injury, scar tissue often results in reduced performance and/or the potential for re-injury. In theory, adult stem cells could replace damaged tendon tissue and scar tissue with healthy, viable tissue.
Easter uses stem-cell therapy mainly for flexor tendon injuries and for suspensory ligament injuries. "For flexor tendons, I find it a rewarding means of returning these horses to a performance level closer to their pre-injury level. Injured tendons treated with stem cells sonographically resemble normal tendon much earlier than conventionally treated tendons. Getting a better quality of healed tissue is the goal," Easter says.
He finds the same to be true for suspensory ligament injuries, especially proximal suspensory injuries. "Early on, I had poor luck with suspensory branch lesions, but I think we were losing our stem cells into the fetlock joint space.
"We started using platelet-rich plasma to glue stem cells in those lesions and then began getting a lot better healing response," Easter says.
"As far as what stem cells do for us in tendons and ligaments, I think they make the tears in those structures heal quicker and in the end more closely resemble the original tissue," he says.
"It's interesting to think about whether the tendons are truly back to normal at the 90-day range, when they look sonographically normal. Most of us believe the horses probably are not ready to start back into normal exercise, because they haven't had enough time to gain their tensile strength back, making them subject to re-injury," Easter explains.
"They probably still need at least eight months to get back to the range to where they have enough tensile strength for exercise, so we may not have shortened the overall time interval that much, but I think the tissue that we have in the end more closely resembles that of the original horse than what we used to end up with without stem-cell therapy."
Compared to the results he's seen for years with conventional therapies — anti-inflammatories, stall rest, immobilization, cold therapy, etc. — stem-cell therapy significantly shortens the time for tendon tissue to return to a normal appearance in sonographs, Easter says.
"We used to tell people that if you have a large tear in a digital flexor tendon, the best you could ever hope for was 80 percent of what the (horse's) original tendon was. I think with stem cells we can get the tissues back closer to original," he says.
Garcia-Lopez concurs, saying "What we see clinically, especially with the soft-tissue injuries, is an induction of better regeneration of the tissue that once was occupying (the location) where the lesion is."
"Tendons and ligaments seem to heal in a more normal fashion. Not necessarily a whole lot faster, but ... the fiber pattern (of healed tendons) is as close to normal as possible — not perfectly normal, but on ultrasound pretty darn close. Some of the short studies by the group at Cornell show a better type of composition of the lesion area compared to no (stem-cell) treatment," says Garcia-Lopez.
"With some of those injuries, even with stem cells we have a very hard time getting them to heal on a consistent basis," Garcia-Lopez adds.
With some injuries, the location that is treated with stem cells "plays a huge role on how these horses do. For example, a suspensory ligament in the front limb responds very differently than a hind limb, because of the amount of tension exerted by the hind limb. With a front-limb suspensory injury, there is a chance that the horse will recover without doing anything, as opposed to a hind-limb suspensory injury. Even with stem-cell therapy, it's the same thing. A hind suspensory injury is more troublesome for event horses or racehorses or high-level sport horses than a front suspensory injury," Garcia-Lopez says.
"Even within the suspensory ligament itself, certain areas react very differently (to treatment). For example, with some chronic lesions in jumpers or dressage horses affecting the branches of the suspensory as it attaches to the sesamoid bone, there are a fair amount of setbacks. Colleagues at the university and in private practice also see similar problems in these types of lesions.
"It's not that we put stem cells in and they do great, or that it's a cure-all for everything, but it does help with some of these lesions," Garcia-Lopez says.
Cartilage regeneration
"Embryonic stem cells have shown promise for cartilage regeneration," says Fortier, but there are some difficulties, so her group is doing research with equine mesenchymal-derived cells.
Fortier's Cornell laboratory generated a stem-cell concentrate from sternal bone-marrow aspirate and researchers test it in equine models of articular cartilage loss.
They have treated 10 experimental horses "in which 15-mm full-thickness defects were made on the lateral trochlear ridge of the femur," and 18 clinical cases, Fortier says. No adverse reactions were seen. The animals are convalescing and follow-up data is pending.
Future stem-cell uses
"There are some encouraging aspects to this technology, but definitive proof of efficacy is still lacking," says Fortier. "There are still gaps in our knowledge, although the technology is developing rapidly."
"There is a client-based use for stem cells," Peroni says. "People have learned we have this treatment modality for the horse and request it. One of the good things (about stem-cell therapy) is that there really aren't any down sides.
"Still, people need to stop thinking that stem cells are the 'silver bullet' for any tendon and ligament injury. It is still vitally important that traditional measures be employed, such as rest and rehabilitation, although I think the quality of the healing may be improved after stem-cell injection."
"We're starting to see more people asking for this therapy, because they've become familiar with it through the media," says Garcia-Lopez. "For the joints, I'm still very cautious. It just depends on the condition. For instance, for horses with end-stage arthritis ... obviously I don't think you can just inject stem cells and have a horse recover. You might give it relief for a short period, but it's not as if you are regenerating cartilage. But for some soft-tissue injuries, for some cysts, we are definitely more comfortable using it (stem cells) as a viable alternative. ... As an adjunct to other therapies, I think it is going to be very effective."
"Stem-cell regenerative medicine is on the horizon, so a basic understanding of stem-cell biology is important for surgeons," Fortier says.
"Although there are several exciting studies suggesting the existence of stem cells in adult tissues and the ability of these and ES cells to transdifferentiate across tissue lineages, indisputable in vivo data is lacking. Studies need to be carefully evaluated; biologics advertised as "stem-cell therapies" should be closely scrutinized before clinical application. Still, the potential benefits of stem-cell transplantation ... are limitless," says Fortier.
"There are still so many questions. Maybe two stem cells are enough in some cases and we don't need 200. Do you start turning them into tendon tissue before you put them into the horse? I think we'll answer a lot of these questions. Perhaps in 20 years we can simply call on the resident pool of stem cells and without taking anything out of the body just figure out a way to call them into action."
Kane is a Seattle author, researcher and consultant in animal nutrition, physiology and veterinary medicine, with a background in horses, pets and livestock.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.





