Using high-frequency radio wave technology in veterinary surgery
Like a scalpel, radiosurgery provides a sense of tactile sensation. And as with a laser, with radiosurgery there is an absence of tissue resistance.
Practitioners have several options for incising tissue when performing surgery. The modality they choose depends on their experience, the type of surgery they are performing, the type of tissue being cut, and even the patient's species. The cost of the instrumentation may also play an important role in the decision-making process. This article discusses the physics of radiosurgery and briefly compares radiosurgery with other surgical devices.

Figure 1. A small-diameter wire electrode is used to concentrate the radio wave, producing a precise incision with minimal distribution of heat laterally into the tissue.
TECHNOLOGICAL DEVELOPMENTS
Historically, hemorrhaging tissue was cauterized with metal that had been heated in an open flame. A modern innovation of this firing iron concept was electrocautery, which used an electric current passed through a wire loop to generate heat. In the 1920s, Bovie developed the first practical electrosurgical device. Electrosurgery uses an electrode to channel electric current through a patient to an indifferent electrode attached to the patient. The indifferent electrode then channels the electric current back to the electrosurgery device. Radio frequency machines convert alternating current to direct current, which then passes through a coil or rectifier to generate a radio wave. The radio waves then pass through a high-frequency waveform adapter to modify the radio wave's shape and amplitude. The radio waves are transferred from the electrode tip to the patient.
HOW RADIOSURGERY WORKS
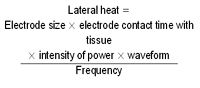
Radiosurgery uses a 4-MHz radio wave that passes from an active electrode (hand-held instrument) to a passive electrode (ground plate beneath the patient). The 4-MHz frequency is similar to that of marine band radios because it is above the AM spectrum but below the FM spectrum.1,2 Tissue resistance to the radio wave transmission volatilizes cells at the tip of the active electrode. Damage to tissue adjacent to the incision is limited provided a good technique is used. Similar to a scalpel blade incision, a radiosurgical incision should be made by using a smooth continuous motion. Unlike a scalpel blade, a radiosurgical electrode cuts without pressure. The character of the cut made with radiosurgery is determined by the type of electrode, contact time with the tissue, intensity of power, nature of the radio wave (waveform mode), and radio wave frequency. The above formula demonstrates how these parameters interact:
Electrode size and configuration
The active electrode transmits radio waves when energized. Numerous electrode configurations are available. The proper electrode to use depends on the type of tissue to be incised and the surgeon's preference.

Figure 2. A large-diameter wire electrode is used once the skin incision is made to incise subcutaneous layers. The larger-diameter needles dissipate more heat laterally into the tissue, sealing small blood vessels to minimize hemorrhage.
Small-diameter electrodes require lower power settings and produce less lateral heating of tissue adjacent to the incision. Thinner-wire electrodes (wire diameter 0.009 to 0.004 in) are generally used to incise skin (Figure 1). The depth of the incision is determined by the length of wire exposed from the insulated housing of the electrode.
Large-diameter electrodes require higher power settings and produce more lateral heat. Large-diameter electrodes are ideal for subcutaneous dissection because lateral heat is useful for hemostasis (Figure 2).
Many specially designed electrodes can be used in oral, dermatologic, reproductive, and ophthalmic surgery. For example, loop electrodes are especially useful for removing small skin masses. If some of the lesion remains, the tissue can be shaved with the electrode until all abnormal tissue is removed (Figure 3). 3 Distichia and ectopic cilia of the eyelids can be eliminated by inserting a 0.004-in-diameter wire electrode along the hair shaft and applying a small amount of power (Figure 4). 4,5

Figure 3. A loop electrode is used to remove a small skin mass. The loop is placed over the lesion, and the mass is grasped with forceps. The electrode is activated and brought through the tissue. A shaving technique can then be used if the base of the lesion remains and requires removal.
Although not part of the formula, the passive electrode is important as well. The passive electrode is the antenna that receives radio waves emitted from the active electrode and returns the energy to the machine. Unlike an electrocautery unit, the passive electrode is not a grounding terminal, so it does not have to be in direct contact with the skin and does not require conductive gels. Placing the passive electrode close to the surgical area decreases the power required to cut tissue, reducing the possibility of lateral thermal damage. The interaction between the passive and active electrodes is similar to that of your car radio in that the radio (passive electrode) has a clearer signal when you are closer to the transmitter (active electrode).
Contact time with tissue
Active electrode contact time with the tissue is directly proportional to the lateral heat transferred to tissue. A well-planned surgical approach and experience with radiosurgery improve efficiency, reducing tissue contact time. If you perform reconstructive or blepharoplasty procedures, marking the area to be incised with a skin marking pen is helpful.
Power intensity
Proper power intensity varies with the tissue being cut. Correct power application allows for enough generated heat to volatilize cells at the tip of the electrode. With proper power intensity, the electrode passes smoothly through the tissue with no sparking or resistance. Insufficient power causes lateral accumulation of heat because of drag. Drag from an improperly powered electrode tends to increase hemorrhage because tissue is torn rather than cut. Likewise, excessive power results in excessive lateral heat because of sparking.
Waveform
Four waveforms are used in radiosurgery. The fully filtered, or continuous, waveform is a continuous high-frequency wave that produces a smooth cutting action. The continuous waveform generates the least amount of lateral heat. When the continuous waveform is delivered by a fine-wire electrode, the incision is comparable to that made by a scalpel.1

Figure 4. Focal distichia may be removed from the eyelid margin by using a very low power setting and a small-diameter wire electrode. The electrode is slid down beside the hair and activated, destroying the hair follicle. No resistance is felt when the hair is removed if the follicle is properly destroyed.
The fully rectified modulated waveform differs from the continuous waveform by inducing a minute pulsation of the wave; this slightly reduces the efficiency of the cut. The fully rectified modulated waveform generates some lateral heat that is useful in hemostasis. When combined with a large-diameter needle electrode, the fully rectified modulated waveform is excellent for subcutaneous dissection.
For more vascular tissues in which hemostasis is critical, you may select the partially rectified modulated waveform. This waveform is an intermittent transmission of high-frequency waves that increases lateral heat transmission, resulting in excellent hemostasis. Blood vessels up to 1/16 of an inch may be sealed with the electrode in the partially rectified modulated waveform mode. Alternatively, hemostasis may be achieved by an indirect method while in this mode by touching the electrode to a hemostat while it grasps the vessel. The indirect method is familiar to any surgeon who has used electrocautery for coagulation in a similar manner.
Finally, there is the fulguration, or spark-gap, waveform. This waveform delivers a mutated electric current that rapidly dehydrates tissue in contact with the active electrode. Much of the tissue destruction produced in this mode is limited by the insulating effect of carbonized tissue, the air space the spark must jump to contact the tissue, and the movement of the electrode by the surgeon. The spark-gap waveform mode is not used when cutting skin or any tissue in which scar formation would be detrimental. This mode has been used in combination with a ball electrode to treat anal fistulas in people.6
Frequency
The final factor in the equation is the denominator, frequency. Radiosurgical instruments operate at frequencies of 3.8 to 4 MHz. Electrocautery devices operate at much lower frequencies, in the 300- to 500-kHz range. Higher frequencies result in less lateral distribution of heat from the incision and more accurate application of energy.2 Interestingly, 4 MHz appears to be the ideal frequency, in that frequencies higher than 4 MHz can create channeling, thus damaging tissue distant to the incision, and higher frequencies increase the risk of sparking, resulting in excessive lateral heat transfer.7
PROS AND CONS OF VARIOUS CUTTING INSTRUMENTS
Tissue cuts are produced when tissue fibers are divided by a concentrated application of energy. To understand the advantages and disadvantages of instruments used to divide tissue, you must understand how cuts are made and how different tissues respond to cuts. Three principal factors are involved in the cutting process: the properties of the tissue to be incised, the shape of the instrument, and its guidance by the surgeon.8
Tissue properties
A key property of tissue is sectility. Tissue sectility is determined by the degree fibers are cut compared with how much they shift as energy is applied. Tissues of high sectility are more easily cut, while those of low sectility are apt to remain intact. Sectility may be enhanced by increasing tension directly in front of the cutting instrument and by increasing the speed of the cutting device's travel. Placing tension on low-sectility tissue while making an incision requires extensive mechanical support and may create a final incision that looks quite different from that initially intended by the surgeon. The eyelids are good examples of low-sectility tissue. They are difficult to incise in their normal state, but cutting is enhanced through mechanical support (e.g. chalazion forceps).
Instrument shape
The action of a scalpel is determined by the sharpness and shape of the blade. The sharper the cutting edge, the less the tissue resistance, which results in more efficient cuts. The length of the cutting surface is also important. A longer blade edge has greater lateral resistance, resulting in the blade's following the path of least resistance when guided parallel to the blade's cutting surface.8 Shorter blades have less lateral resistance, allowing a surgeon to manipulate the blades around surfaces. So blade length is directly proportional to the ease with which a surgeon makes a straight incision but inversely proportional to the ease tissue is incised along contours. Scalpel blades are ideal for cutting tissues of high sectility, especially in cases in which long straight cuts are desired. Lasers and radiosurgical electrodes offer the advantage of being point cutting devices (devices with very short blade length, or, in the case of these modalities, no blade length) in which there is no lateral resistance, allowing the cut to be completely controlled by a surgeon.
Since tissue resistance is not a factor with lasers or radiosurgical devices, tissue sectility is not a factor. This allows a surgeon to make precise cuts with minimal tissue support. The cutting ability of the laser is determined by the source of atoms being excited to emit energy as photons. Examples of lasers used in veterinary medicine include carbon dioxide, neodymium:yttrium-aluminum-garnet (Nd:YAG), and diode lasers. Carbon dioxide lasers are commonly used in veterinary medicine to incise skin and other superficial tissues. Carbon dioxide lasers produce an infrared light (10,600 nm) that is invisible to people. The slower a surgeon passes the laser beam across the tissue, the deeper the cut; however, similar to radiosurgical electrodes, the slower the passage, the greater the lateral heat distribution. The wavelength of light emitted by a laser also determines its effectiveness in ablating tissue. For example, carbon dioxide laser light is preferentially absorbed by water, and cells with high water content are vaporized as they absorb carbon dioxide laser energy; thus, high-moisture tissues will be more effectively removed. Diode lasers emit a light preferentially absorbed by melanin, so pigmented tissue is more effectively removed.
As previously discussed, many factors are involved in determining the incision made with radiosurgery, including the shape and size of the active electrode. Fine-wire electrodes concentrate the radio wave into tissue with immediate contact. The radio wave vaporizes cells contacting the electrode. Once the cells are vaporized, the resulting air gap between the electrode and adjacent tissue serves as insulation to prevent lateral heat transmission. The length of the exposed wire will determine the depth of the incision. Larger-diameter electrodes transfer the radio wave less efficiently and, while vaporizing cells in contact with the electrode, allow the transfer of some heat laterally to enhance hemostasis.
Surgical guidance
The final principal factor in incising tissue is guidance by the surgeon. Most veterinarians are experienced with scalpels. Scalpels provide excellent tactile sensation through which you may increase or decrease pressure to change the depth of cut. Within the limits of lateral resistance, you can move blades over, through, and around structures to make incisions. Lasers provide no tactile sensation since their path is visually guided. Like a scalpel, radiosurgery provides a sense of tactile sensation. And as with a laser, with radiosurgery there is an absence of tissue resistance. For this reason, some surgeons consider the learning curve quicker and easier with radiosurgery than with lasers.1
Other factors to consider
To avoid postoperative complications, it is important to avoid damaging tissue that surrounds the incision. Steel scalpel blades produce no lateral heat as they pass through tissue. The absence of lateral heat is an advantage in that no surrounding tissue is altered, but it is also a disadvantage in that no hemostasis occurs. Lasers and radiosurgery generate lateral heat to seal small vessels, nerve endings, and lymphatics as incisions are made. Radiosurgery electrodes of varying shapes and different waveforms may be used to enhance hemostasis.
Several studies have been performed to examine the damage done to surrounding tissue by lateral heat transfer by radiosurgery and carbon dioxide lasers.9-11 The tissue damage produced by radiosurgery when in the fully rectified modulated waveform mode is similar to that of a steel scalpel, allowing comparable biopsy samples to be obtained that lack thermal or mechanical artifact.9 A study in people in which oviducts were incised with lasers (carbon dioxide, Nd:YAG, and KTP-532), electrocautery, and radio frequency showed that radio frequency produced the least damage to surrounding tissue and carbon dioxide lasers produced the second lowest amount of damage when compared with scalpel incisions.10 In another study, carbon dioxide lasers were compared with scalpels for resecting the soft palates of brachycephalic dogs. Clinical outcomes were similar in dogs in which lasers or conventional scalpels were used, but surgical times were significantly shorter when lasers were used.12 One surgeon has anecdotally noted that skin incisions made with radiosurgery heal as quickly as those made with a steel scalpel.1
Another factor is equipment cost. The cost of steel scalpel blades varies depending on their intended use, but for the most part the scalpels are a negligible cost of surgery. Radio frequency surgery units are one-third to one-half the cost of lasers.3,13 Additionally, handpieces and electrodes for radio frequency surgery can be steam-autoclaved. One factor that is often not considered is the space a unit occupies when not in use. While none of the mechanical methods of surgical incision compares with the small size of a box of scalpel blades, radiosurgical units occupy a much smaller space when compared with lasers, resulting in less clutter in the operating room. A disadvantage of both radio frequency surgery and lasers is smoke generated during the procedure. A smoke evacuation system should be considered when using either radio frequency surgery or lasers to incise tissue. Be careful to avoid using alcohol or other flammable substances when preparing skin for surgery if radiosurgery will be used.
CONCLUSION
Practicing veterinarians have many alternatives for making incisions during surgery. The choice of instruments varies depending on the surgeon's preference and experience, tissue to be cut, procedure to be performed, and cost of equipment.
In my practice, I have found that the lack of hemorrhage and the ability to incise tissue without extensive manipulation when using radio frequency surgery greatly reduces surgery time. Additionally, I have observed that animals have less postoperative swelling when I use radiosurgery rather than a scalpel, resulting in less self-trauma and less dehiscence.
The learning curve for radiosurgery is not steep for veterinarians familiar with scalpels. Similar tactile movements are required. The most difficult sensation to learn is that no resistance is felt when incising tissue. In our practice, we are developing techniques to raise conjunctival flaps, replace hyperplastic third eyelid glands, and perform enucleations in addition to correcting eyelid abnormalities. Practitioners should consider radiosurgery as an alternative to steel scalpels when performing surgery on easily deformable and highly vascular tissue.
William W. Miller, DVM, MS, DACVO
Advanced Animal Eye Clinic
3767 Summer Ave.
Memphis, TN 38122
REFERENCES
1. Older, J.J.: The value of radiosurgery in oculoplastics. Ophthalmic Plast. Reconstr. Surg. 18(3):214-218; 2002.
2. Niamtu, J.: 4.0 MHz radio wave applications in cosmetic facial surgery. Cosmetic Derm. 16:33-46; 2003.
3. Saidi, M.H. et al.: Comparison of office loop electrosurgical conization and cold knife conization. J. Am. Assoc. Gynecol. Laparosc. 1(2):135-139; 1994.
4. Pfenninger, J.L.; DeWitt, D.E.: Radiofrequency surgery (modern electrosurgery). Pfenninger and Fowler's Procedures for Primary Care, 2nd Ed. (J.L. Pfenninger; G.C. Fowler, eds.). Mosby, Philadelphia, Pa., 2003; pp 213-224.
5. Bosniak, S.; Cantinsano-Zikha, M.: Radio-surgery: A 25 year history of scarless mole removal. Operative Tech. Oculoplastic Orbital Reconstr. Surg. 4:109-112; 2001.
6. Gupta, P.J.: Radio frequency "sutureless" fistulotomy—A new way of treating fistula in anus. World J. Gastroenterol. 9(5):1082-1085; 2003.
7. Altman, R.B.: Radiosurgery. Seminars in Avian and Exotic Pet Medicine. W.B. Saunders, Philadelphia, Pa., 2000; pp 180-183.
8. Eisner, G.: Eye Surgery: An Introduction to Operative Technique. Springer-Verlag, New York, N.Y., 1980; pp 14-24.
9. Turner, R.J. et al.: Analysis of tissue margins of cone biopsy specimens obtained with "cold knife," CO2 and Nd:YAG lasers and a radiofrequency surgical unit. J. Reprod. Med. 37(7):607-610; 1992.
10. Olivar, A.C. et al.: Transmission electron microscopy: Evaluation of damage in human oviducts caused by different surgical instruments. Ann. Clin. Lab. Sci. 29(4):281-285; 1999.
11. Maness, W.L. et al.: Histologic evaluation of electrosurgery with varying frequency and waveform. J. Prosthet. Dent. 40(3):304-308; 1978.
12. Davidson, E.B. et al.: Evaluation of carbon dioxide laser and conventional incisional techniques for resection of soft palates in brachycephalic dogs. JAVMA 219(6):776-781; 2001.
13. Kronemyer, B.: Radiosurgery is safe, versatile and income-producing, surgeon says. Ocular Surg. News 18:22; 2000.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.