Wound management: simple skin flaps (Proceedings)
Wound closure following extensive tumor resection or trauma may require reconstruction surgery. Skin can be borrowed from another location to accomplish closure without tension.
Wound closure following extensive tumor resection or trauma may require reconstruction surgery. Skin can be borrowed from another location to accomplish closure without tension. Free skin grafts have been used with good success, but this procedure requires healthy granulation tissue, is technically demanding and requires intensive postoperative care. Skin flaps can be transplanted without the presence granulation tissue and a large amount of skin can be moved if a direct cutaneous artery and vein are included in the flap.
Classification of skin flap
Flaps are categorized according to 1) circulation, 2) various forms of compound, 3) location in relation to the recipient bed. A compound flap incorporates skin, and other structures such as muscle, fat or bone.
Circulation
According to the circulation classification we have subdermaal plexus or axial pattern flap. Dogs skin is fed through direct cutaneous artery running in the panniculus muscle. (Figure 1) Branches of the direct cutaneous artery supply the subdermal and the dermal plexus.

Figure 1
Survival of flaps used in dogs and cats elevated without including a direct cutaneous artery and vein depends on the deep or subdermal plexus: subdermal plexus flap. A pedicle graft incorporating a direct cutaneous artery is an axial pattern flap. They have an excellent blood supply and survived better than subdermal plexus flap.
Location
Flaps that are developed adjacent to the recipient bed are called local flap whereas flaps transferred from a distant region are termed distant flaps. Local flaps are commonly used for closure of defect that cannot be approximate by simple undermining and suturing. They depend on forming a flap in the neighboring area where loose elastic skin prevails. The secondary defect can be closed primarily. Distant flaps are used for major skin defects on the extremities. Local flaps are based on subdermal plexus blood supply while the distant flap are based on direct cutaneous artery.
Local flaps
Local flaps are subdivided in:
• rotation flap
• transposition flap
• interpolation flap.
Rotational flap
Rotation flap is a semicircle sharing a common border with a triangular defect. A curved incision is usually created in a stepwise fashion and the flap undermined until the defect can be closed without tension. (Figure 2)

Figure 2
Transpositional flap
A transposition flap is a rectangular pedicle graft usually created within 90° of the long axis of the defect. An edge of the defect is common to a portion of the flap border.(Figure 3) The distant from the pivot point to the tip of the flap must equal the distance between the pivot point and the most distant point of the defect. (Figure 3 A & B
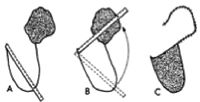
Figure 3
Interpolating flap
An interpolating flap is a rotating rectangular flap without any common border with the defect.(Figure 4) A portion of the flap covers the skin between the donor bed and the recipient bed. The flap is suture to the recipient bed on the 3 edges only. After the flap healed with the donor bed, a second surgery is necessary to eliminate the part of flap covering the skin between the defect and the donor bed. This part of the flap can be tubed. An alternative technique is to make a bridge incision between the defect and the donor bed, and to suture the flap to the edges. No second surgery will be necessary to resect the excess amount of flap.
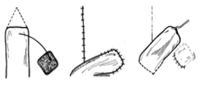
Figure 4
Axial pattern flaps
Axial pattern flaps are based on a major direct direct cutaneous artery. With those flaps a large amount of skin can be moved over a long distance with its own blood supply. Therefore they allow coverage of major wounds in area where not much skin is present (Table 1). Since they are based on their own blood supply they do not require a healthy granulation tissue to survive, and they can resist to infection. Each flaps have specific landmarks. If those landmarks are well followed more than 90% of the skin flap will survive. The flaps require minimal post-operative cares.

Table 1: Major axial pattern flaps in dogs and cats
Several major direct cutaneous arteries are used for axial pattern flaps in dogs and cats: omocervical artery, the thoracodorsal artery, deep circumflex iliac artery, and the caudal superficial epigastric artery (Figure 5).
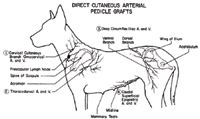
Figure 5
The superficial brachial artery, the genicular artery axial pattern flap, and the reverse saphenous conduit flap have also been described in dogs. The thoracodorsal and the caudal superficial epigastric flap are the most versatile flaps in dogs and cats.
Caudal superficial epigastric axial pattern flap
This flap can be used to closed defect on the hind leg proximal to the distal tibia in dogs and to the tarsus in cats. The last 3 mammary glands can be harvested in dogs and cats.
After surgical preparation of the recipient and donor beds, a sterile pen is used to delineate the border of the flap according to the size of the defect.(Figure 6) The medial border is abdominal midline and the lateral border is determined based on the amount of loose skin available for closure of the donor site. The cranial border is between the 2nd and 3rd mammary glands in the dog and 1st and 2nd mammary glands in the cat. The flap should be extended caudally passed the 5th mammary gland. A combination of sharp and blunt dissection is used to elevate the flap. Caudal to the last mammary gland, particular care is taken not todisrupt the caudal superficial epigastric artery and vein. In male, care is taken to avoid transection of the caudal superficial epigastric artery and vein by including the base of the prepuce. Minimal cauterization should be done during the dissection of the flap. At this stage, the skin flap can be islanded by completing the incision 3600 around the base of the flap. Island flaps have a better freedom of motion. The flap is transferred to the recipient bed either by making a bridging incision between the donor and the recipient beds or by creating a tube. The skin flap is then laid over the defect and sutured without tension. A subcutaneous suture followed by skin sutures (continuous pattern, 4-0 nylon) are used. The recipient bed is closed in a routine fashion. A drain (Penrose or closed continuous suction drain) can be placed under the flap for a few days. In the postoperative period, the limb is kept bandaged until sutures are removed.
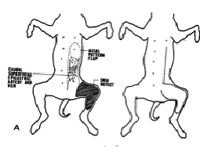
Figure 6