10 axioms to aid your diagnostic skills
Not all diagnoses are equal in terms of their prognostic and therapeutic implications.
Treating a patient without a diagnosis is analogous to shooting without aiming.
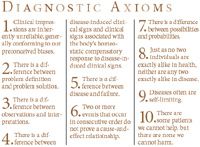
Diagnostic Axioms
Body systems and organs manifest the effects of a variety of different causes of disease in a limited number of ways (pruritis, alopecia, vomiting, diarrhea, polyuria, polydipsia, seizures, coma, azotemia, anemia, etc.). All of these clinical signs may have different causes that are not always easy to distinguish by routine clinical procedures. The ability to reliably and consistently establish the different causes of various types of illness requires specialized knowledge, and the wisdom to wisely apply that knowledge in such fashion that it will benefit patients.
The noun "diagnosis" is derived from a Greek word meaning to distinguish or discern. The word "discern" conveys the concept of an ability to recognize and understand the difference between two or more things. In this context, it is one thing to make a diagnosis, and another to be able to substantiate it.
Though we name the things we know, we do not necessarily know them because we name them. If we begin the diagnostic process with a preconceived notion (or bias) about the cause of a patient's illness, we have a tendency to ask questions and perform diagnostic procedures to support our preconceptions. We tend to ignore clinical findings that do not fit our stereotype.
If we are not careful in how we collect information, we may derive erroneous diagnoses. In fact, an erroneous diagnosis is one of the most common diseases.
Would you agree that a correct diagnosis is a key prerequisite to providing safe and effective treatment for various illnesses? Would you also agree that diagnoses often are a matter of opinion rather than matter of fact? Isn't it true that most diagnoses often require us to make decisions in the absence of certainty?
Medical diagnoses are based on probability. Therefore we must use caution not to fall into the trap of making them on the basis of faulty logic or insufficient information.
Shortcuts in diagnostic reasoning tend to become increasingly prevalent when veterinarians are subjected to the pressures of a high caseload in a busy hospital. In this context, shortcuts often are defended on the basis of practicality. Although practicality is a virtue, we must use caution not to use the concept of practicality as an excuse for ignorance. Why? Because, a misdiagnosis may be more detrimental to the patient than the illness. A wise sage once penned this thought: "Heaven defend me from a busy doctor."
How do we know when our diagnoses are in error? If we do not have a system designed to periodically audit our diagnoses for accuracy, we are less likely to recognize and correct our errors. If the accuracy of our diagnoses is never questioned, we may become over-confident in our judgments with a tendency to rely less and less on clinical data and more and more on our intuition. What is the inevitable result? Experience has revealed that diagnosis by intuition is often a rapid method of reaching the wrong conclusion.
Based on the premise that almost right is still wrong, the primary objective of this diagnote is to review some clinical axioms that foster the diagnostic process.
Diagnostic axioms
After 45 years of serving as a clinician in a university hospital, I have learned that periodically reviewing diagnostic axioms is helpful as a self-teaching aid. An "axiom" is a statement universally accepted as true. In the box (p. 10S), I have listed 10 key axioms associated with the diagnostic process. Review the items and test yourself as to whether you can explain (or define) them. Then review the explanations.
AXIOM 1: Clinical impressions are inherently unreliable, generally conforming to our preconceived biases.
Strong preconceptions are not a substitute for objective evidence. For example, on the basis of logic, urologists have for decades instructed human patients with calcium oxalate uroliths to reduce their dietary calcium intake to minimize stone recurrence. However, several contemporary epidemiological studies have revealed that reducing dietary calcium actually increased the frequency of calcium oxalate urolith recurrence. What is the point? Belief or skepticism does not alter the truth. Rather than forcing preconceived conclusions on the facts, we must be alert to allow reproducible observations (facts) to lead us to reasonable conclusions.
AXIOM 2: There is a difference between problem definition and problem solution.
We use the term diagnosis in context of defining the cause(s) of clinical signs. The ability to define a patient's medical problems without overstating them is a crucial first step in the diagnostic process, since one must be able to accurately define problems before they can be solved. No veterinarian has or ever will be trained to single-handedly solve all types of medical problems. No one can recall enough knowledge and be proficient with enough techniques to guarantee that (s)he alone can provide the best care of very patient. Veterinarians can be trained to accurately identify problems, however. They can and should be master "problem definers." Accurate definition of a patient's clinical problems will permit us in our role as diagnosticians to more efficiently utilize available resources, such as journals, books, the internet, consultations, and referrals, to help resolve diagnostic problems. A problem well defined is half solved!
AXIOM 3: There is a conceptual difference between observations and interpretations. Discernment of the difference between observations and interpretations of them (inferences) is critical to making a diagnosis.
Clients frequently confuse these two types of information when describing the illness of their animals to us. A classic example is to misinterpret the observation of tenesmus as constipation in a male cat with urethral obstruction. Although either observations or interpretations may be erroneous, in my experience misinterpretation of a correct observation is the most common pattern of error. A misinterpreted problem is the worst of all problems. Why? Because if erroneous interpretations are accepted as facts, erroneous diagnosis followed by erroneous prognosis and formulation of ineffective or contraindicated therapy may result. This is indeed ironic, in that the patient may acquire a worse condition as a result of having visited the doctor (e.g., the concept of iatrogenesis).
AXIOM 4: There is a difference between disease-induced clinical signs and clinical signs associated with the body's homeostastic compensatory response to disease-induced clinical signs.
Clinical manifestations of disease can be subdivided into the following two classes:
1) signs directly induced by the disease (such as impaired urine concentrating capacity and obligatory polyuria associated with damage to the countercurrent system in patients with bilateral bacterial pyleonephritis), and
2) the body's compensatory response to these signs (such as compensatory polydipsia to maintain fluid balance despite obligatory persistent polyuria).
Other examples of this relationship include compensatory inflammation in response to damaged tissue, fever in response to systemic infectious agents, polychromasia and reticulocytosis in response to anemia and hyperparathomonemia in response to hypocalcemia. Logically then, making a diagnosis of urinary-tract infection solely on the basis of pyuria would be an over-diagnosis because pyuria may be a compensatory response to infectious or noninfectious diseases of the urinary tract.
AXIOM 5: There is a conceptual difference between disease and failure.
Discernment of the conceptual difference between organ disease and organ failure also is fundamental to proper diagnostic refinement. Organ function that is "adequate " to sustain homeostasis is usually not synonymous with "total " organ function. For example, patients with only one functional kidney (an organ donor) have adequate renal function to live a "normal " life without manifestations of renal dysfunction. Even when slowly progressive irreversible renal lesions occur, signs of organ dysfunction do not develop as long as adequate quantities of functional parenchyma (i.e., nephrons) remain to maintain homeostasis. This concept is the basis for distinguishing organ disease (such as cardiac valvular insufficiency associated with normal pulse rate and rhythm) from organ failure (such as abnormal circulation associated with abnormal cardiac rate and rhythm which ultimately occur as a result of irreversible progressive cardiac valvular insufficiency). The approach to management of a patient with cardiac valvular insufficiency and adequate cardiac function is very different from management designed for a patient with cardiac valvular insufficiency and congestive heart failure.
AXIOM 6: Just because two or more events occur in consecutive order do not prove a cause-and-effect relationship.
Unrelated and unforeseen coincidences commonly occur in the lives of all living beings. Therefore, extreme caution must be used in the interpretation of uncontrolled observations. The ability to recognize true cause-and-effect relationships is not an innate characteristic, it must be learned.
The key point is that just because two or more events occur in consecutive order does not prove a cause-and-effect relationship. Consider this example:
In the late 1970s and early 1980s, vesicourachal diverticula were cited as playing an etiologic role in some cats with lower urinary-tract disease (LUTD). Treatment by surgical extirpation was recommended in most veterinary textbooks at that time. The observation that clinical signs subsided coincidentally with diverticulectomy, and lack of studies of the biologic behavior of macrosopic diverticula without surgery, reinforced the interpretation that this anatomic abnormality was a cause of LUTD.
However, subsequent studies of the biological behavior of vesicourachal diverticula revealed that they were a sequela, rather than a cause of LUTDs. Most of them spontaneously resolved with appropriate medical therapy of the underlying problem. Surgery was unnecessary. This example highlights the fact that favorable outcomes associated with our treatments do not prove that our diagnoses were correct, or that our treatments were beneficial.
AXIOM 7: There is a conceptual difference between possibilities and probabilities.
The need to discern that difference is another key medical axiom. In general, numerous diagnostic possibilities are reduced to a few or one diagnostic probability on the basis of proper collection and interpretation of clinical data. However, even after collection of a large quantity of relevant data, many diagnostic probabilities still represent a matter of educated opinion rather than a matter of fact. Absence of clinical evidence of suspected diseases is not always synonymous with evidence of absence of these diseases. It follows that we as veterinarians should convey to our clients that our diagnoses, prognoses and treatment recommendations are not infallible. The practice of veterinary medicine often requires judgment in the absence of certainty.
AXIOM 8: Just as no two individuals are exactly alike in health, so neither are any two in disease.
The concept of a key pathogno- monic finding that will unlock the door to a specific diagnosis is misleading. Rarely will a single historical event, physical exam finding, laboratory test result or radiograph/ultrasound finding provide information of sufficient specificity to warrant a specific diagnosis.
Likewise, memorization of textbook descriptions of characteristic clinical findings of specific diseases is not consistently effective. Why? The same disease typically induces a variety of manifestations of different degrees of severity in different patients. Most textbook descriptions are abstracts of prototypical disease features, all of which often do not coexist in the same patient. Just as no two individuals are exactly alike in health, so neither are any two in disease.
AXIOM 9: Diseases often are self-limiting.
The severity of many diseases subsides in a day or two. In this situation, any treatment may appear to be bene- ficial as long as it is not harmful.
AXIOM 10: There are some patients we cannot help, but there are none we cannot harm.
Especially when we are overconfident, and when saving face is more important than saving lives. We all can extinguish life. However, who among us can create life?
Not all diagnoses created equal
Are their conceptually different levels of diagnoses? Not all diagnoses are equal in terms of their prognostic and therapeutic implications.
Based on results obtained from a variety of sources, including: 1) the patient's history, 2) the physical examination, 3) various laboratory tests, 4) radiography and other methods of diagnostic imaging, 5) endoscopy, 6) biopsy, and/or 7) exploratory surgery, we recommend that clinical problems be classified into one of four progressive levels of refinement. Listed from the lowest to the highest level of refinement, problems may be diagnosed as:
1. An unquantified (subjective) symptom or clinical finding (e.g., depression, polydipsia, polyuria, or vomiting). If the problem(s) is mild and transient, treatment my not be warranted. However, if clinical signs are severe, persistent or progressive, further information is often warranted to identify its source/cause, and to formulate a prognosis and treatment plan.
2. A reproducible (objective) diagnostic finding (e.g., mild proteinuria; urine/protein creatinine ratio of 4:7; palpable splenic mass; a hematocrit of 15 associated with marked polychromasia; serum potassium concentration of 2.4 mEq/l). If the problem is mild and transient, treatment may not be warranted. However, if it is severe, persistent or progressive, further information usually is warranted to identify its source/cause, and to formulate a prognosis and treatment plan. In addition, it may be useful to repeat appropriate diagnostic procedures to determine if the abnormality is getting better, worse or remaining the same, and to determine the rate of change of the abnormality.
3. A pathophysiologic syndrome (e.g., renal failure, congestive heart failure, hepatic encephalopathy, nephrotic syndrome, or malabsorption syndrome). Problem refinement of this degree requires integration of signs induced by the disease (e.g., polyuria) and the body's compensatory responses to the effects of disease (e.g., polydipsia). Pathophysiologic syndromes are frequently recognized without knowledge of their underlying cause(s). Patients with various pathphysiologic syndromes of unknown cause often benefit from supportive and symptomatic therapy (e.g., in patients with renal failure, correction of deficits and excesses in fluid, electrolyte, nutrient, acid-base, and endocrine balance).
4. A specific diagnostic entity (e.g., immune complex protein-losing glomerulonephropathy and nephrotic syndrome caused by Borrelia bergdorferi; splenic hemangiosarcoma with metastases to the peritoneum, omentum, lungs and heart; congenital intahepatic portovascular shunt with hyperammonemic encephalopathy and ammonium urate urocystoliths). The goal of determining the specific cause(s) of disease is of more than academic interest. Knowledge of the specific cause of an illness is most likely to permit: 1) a more accurate prognosis of the biological behavior of the illness; 2) assessment of the ability of the body to functionally compensate for irreversible damage to various biologic functions; 3) assessment of the availability of specific therapy (in contrast to supportive and symptomatic therapy) to eliminate, halt, or control progression of the underlying cause(s) of the disease (s); and 4) assessment of the need for supportive and/or symptomatic therapy of associated dysfunctions.
Although a specific diagnosis represents the highest level of refinement of the patient's status, it is not always necessary or even desirable to expend the resources or expose the patient to unnecessary risks associated with invasive diagnostic techniques to determine the specific cause of all illnesses.
Examples include self-limiting non-communicable infectious diseases, transient gastrointestinal signs associated with dietary indiscretion, and end-stage organ (hepatic, renal, etc.) failure that has advanced beyond recovery even if the underlying cause is eliminated.
Diagnoses should not be overstated by guessing their underlying causes based on insufficient or faulty evidence. They should be stated at the level of refinement that can be reasonably justified on the basis of current knowledge about the patient. Why? Because if the diagnosis is overstated, misdiagnosis, misprognosis and formulation of ineffective or contraindicated therapy may result. No patient should be worse for having seen the doctor.
What is the meaning of the word iatrogenic? The term iatrogenic contains Greek root word "iatros," which is translated as physician, and the Greek root word "gennan." which means " to create or produce." Dorland's medical dictionary defines iatrogenic as any adverse condition or complication in a patient occurring as a result of treatment by a physician. Because there is no comparable English word for adverse events in patients resulting from treatment by veterinarians, the word iatrogenic has been adopted by our profession. The fact that iatrogenic is considered as a pathophysiologic mechanism of disease emphasizes that there are some patients we cannot help, but there are none we cannot harm.
As is the situation with the research scientist, consistent success of practicing veterinarians in defining and solving patients' problems is dependent on reproducibly collecting, recording, organizing and interpreting clinical data. The problem oriented medical system provides a "blueprint" which all of us in veterinary practice can follow in our efforts to provide proper, timely, and cost-efficient care for our patients.
The problem-oriented veterinary medical record is the focal point of the problem-oriented veterinary medical system, in that relevant information is linked visibly to specific problems (i.e., it is problem-oriented).
It is the antithesis of the chaotic veterinary medical record. The problem-oriented system is a practical clinical method that can be relied upon to guide us toward the correct diagnosis.
by Carl A. Osborne DVM, PhD, Dipl. ACVIM
Dr. Osborne, a diplomate of the American College of Veterinary Internal Medicine, is professor of medicine in the Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Minnesota.