Acute pancreatitis in dogs: a diagnostic and therapeutic update (Proceedings)
The first step in the approach to the acutely vomiting dog is to determine that vomiting and not regurgitation is present.
Acute vomiting – Diagnostic approach
The first step in the approach to the acutely vomiting dog is to determine that vomiting and not regurgitation is present. Vomiting is associated with signs of nausea (depression, salivation, and frequent swallowing,) that is followed by abdominal contractions prior to the expulsion of material. Regurgitation is associated with esophageal disorders and occurs passively, usually associated with increased intrathoracic pressure that may be caused by excitement, activity, or changes in body position.
Once you have determined the dog is vomiting rather than regurgitating,, the next step is to determine if a self-limiting or life threatening problem is present. This assessment is crucial and must be based on a thorough history, careful physical examination, clinical experience and judgment, and a sound understanding of the differential diagnosis of acute vomiting. Dogs with acute pancreatitis can present with both types of vomiting. Animals should be considered to have a potential life-threatening problem if some of the following are present: Moderate or severe abdominal pain, lethargy, dehydration or pyrexia, enlarged distended bowel, frequent and severe diarrhea, hematemesis, frequent vomiting or increasing frequency of vomiting, signs of systemic disease, or puppies with an incomplete vaccination history. If a clear distinction cannot be reached, it is better to error on the cautious side and consider a potential life-threatening problem.
Dogs with a self-limiting problem require minimal diagnostic testing and symptomatic treatment, and often cease vomiting within 12-24 hours of initial presentation. A minimum data base for animals with self-limiting vomiting should include determination of packed cell volume and total solids, zinc sulfate fecal flotation, and digital rectal examination. Some common causes include acute gastritis or enteritis, dietary indiscretion, drug administration, toxin ingestion, foreign body ingestion, parasites, and coronavirus. Reclassification to life-threatening status may be indicated if an animal initially assessed as having self-limiting acute vomiting continues to vomit despite appropriate symptomatic therapy.
Life-threatening cases of acute vomiting require an in-depth diagnostic evaluation, vigorous symptomatic management, and often specific therapy directed at the underlying cause. The initial minimum data base for life-threatening acute vomiting includes a complete blood count, biochemical profile with amylase and lipase, urinalysis, zinc sulfate fecal flotation, and survey abdominal radiographs. After the initial evaluation, additional diagnostic studies may be indicated in some instances, such as upper GI endoscopy, upper GI barium series, abdominal ultrasonography, ACTH response testing, or surgical exploration of the abdomen. Some common causes include acute gastritis, dietary indiscretion, hookworms, foreign body obstruction, intussusception, parvovirus, distemper, HGE, acute renal failure, acute liver failure, hypoadrenalcorticism, diabetes mellitus, and pyometra.
Acute pancreatitis
Acute pancreatitis commonly occurs in the middle-aged, obese female dog. Clinical signs include vomiting, diarrhea, abdominal pain, and fever. Historical association may be made with ingestion of a fatty meal or corticosteroid administration. Acute pancreatitis rapidly leads to severe dehydration (dry mucous membranes, loss of skin turgor, prolonged capillary refill time, or enophthalmos) and may progress to hypovolemic shock (tachycardia and weak peripheral pulses). In a recent necropsy study, 64% had pancreatic inflammation, many with chronic changes. Most of these dogs had another primary necropsy diagnosis, suggesting that chronic subclinical inflammation with lymphocytes may be an age related change. These findings question the utility of pancreatic biopsy as a gold standard for diagnosis.
The pathogenesis of AP is complex. It is a self-perpetuating auto-digestive process. As auto-digestion of the pancreas occurs, potent digestive enzymes are released into the parenchyma of the pancreas, blood vessels, and to the adjacent abdominal cavity. This causes severe hemodynamic alterations, localized inflammation, and can trigger disseminated intravascular coagulation. Depletion of circulating and tissue anti-proteases occurs. Vascular collapse develops due to a combination of the following: fluid loss from vomiting and diarrhea, release of vasoactive substances, release of cardiodepressant substances, or fluid sequestration within the abdominal cavity. Progression of the disorder may depend on preservation of pancreatic microcirculation, which can be maintained by fluid therapy.
Cases of AP can have inconsistent laboratory parameters. Diagnosis should not be based on any single test. Common changes include: leukocytosis with a left shift, elevated hematocrit, total protein, and prerenal azotemia (dehydration), elevated ALT and ALP, hypercholesterolemia, hyperglycemia, hypocalcemia, and lipemia. Classically, serum amylase, lipase, and trypsin-like immunoreactivity (TLI) should be elevated. However, elevations are not definitive for pancreatitis as amylase is contained in many tissues and lipase has recently been identified in the stomach. Amylase, lipase, and TLI depend on the kidney for elimination, thus prerenal azotemia due to dehydration from any cause of vomiting results in mild elevations. Some cases of AP have normal or only slightly elevated serum amylase, lipase, and TLI. In experimental AP, serum trypsin-like immunoreactivity (TLI) increases prior to amylase and lipase. Based on preliminary results, a new serum test is showing promise in diagnosing pancreatitis in dogs. The test, serum canine pancreatic lipase immunoreactivity (cpli), was developed by Texas A&M researchers and immunologically measures lipase from the pancreas. The test showed a sensitivity of 82% in the diagnosis of acute pancreatitis; these results are from a low number of cases (11), but are promising. A modification of this test using a monoclonal antibody and a recombinant antigen for calibration has been marketed by IDEXX as the Spec cPL. This test compares favorably with the cPLI and because of plate stability can be run daily with results rapidly reported. In a recent study of necropsied dogs with macroscopic evidence of pancreatitis the cPLI and SPEC cPL correlated and their overall sensitivity was 64%. IDEXX has also developed a in-house screening test (SNAP cPL) that has been shown to correlate with the Spec cPL. More data are needed, but these tests may be the most accurate serum tests for diagnosing acute pancreatitis in dogs.
Radiographic signs of AP are nonspecific and don't often contribute to diagnosis except by eliminating the presence of intestinal obstruction. Ultrasonographic evaluation of the abdomen can be very helpful and may identify a pancreatic mass or an enlarged hypoechoic pancreas that may surrounded by a hyperechoic rim. Pancreatic abscesses and cysts can also be identified.
Treatment
The therapeutic plan should prevent pancreatic secretion and manage hypovolemia while supporting pancreatic circulation. In severe cases, the dog should be maintained NPO and vigorous fluid therapy administered. Lactated ringers is an appropriate fluid to use at a volume necessary to correct dehydration, provide maintenance (44-66 ml/kg/day), and to replace losses due to vomiting and diarrhea. Potassium supplementation, 20 mEq/l KCl, is necessary to replace losses in diarrhea, vomitus, and urine and supplement the lack of food intake. Potassium supplementation should be based on measurement of serum potassium levels. Plasma transfusion (6-12 ml/kg) has been recommended to provide a fresh source of protease inhibitors. Mildly affected dogs may be held NPO and given fluids subcutaneously until the vomiting ceases for 12 hours.
Treatment should continue until parameters used to make a diagnosis return to normal, often 3-5 days in moderately affected dogs. Gradual oral alimentation can be initiated. Initially, ice cubes or small amounts of water are frequently offered. If vomiting does not occur, small amounts of a bland diet can be frequently offered. This diet should be soft and low in fiber, highly digestible, high in carbohydrates, low in fat, and low in protein. Boiled rice, rice with chicken, low fat cottage cheese, or prescription diets such as i/d® (Hills Pet Products), EN® (Ralston Purina), or Low Residue (Iams) are effective. The size of the meals should be slowly increased and the frequency of feeding decreased if vomiting does not recur. If the dog does not vomit for 3 days, the normal diet can be slowly added. Low fat diets have been recommended to prevent relapse.
If vomiting is severe, antiemetics can be used. A phenothiazine, chlorpromazine 0.5 mg/kg q 4-6h, or metoclopramide, 0.2-0.4 mg/kg q 8h can be used. Because phenothiazines cause vasodilation they cannot be started until the dog has been rehydrated. Metoclopramide is contraindicated in cases with GI obstruction so obstruction should be eliminated prior to its use. If prolonged fluid therapy is necessary (7-10 days) total parenteral nutrition should be considered.
The prognosis for cases of AP is variable. Self-limiting cases respond to minimal therapy. Life-threatening cases warrant a guarded prognosis. Response to therapy in 3-5 days is a favorable prognostic sign. Dogs requiring intensive therapy for longer than 7 days carry a guarded prognosis. Because the etiology is unclear, recurrent bouts can occur.
Because the diagnosis of AP is difficult to prove, a thorough evaluation of other causes of acute vomiting, acute diarrhea, and abdominal pain should be performed. Classic findings of AP include: 1) acute vomiting, 2) cranial abdominal pain, 3) pyrexia, 4) leukocytosis with a left shift, 5) elevated serum amylase, lipase, cPLI, and SNAP cPLI and 6) ultrasonographic findings of an enlarged hypoechoic pancreas. Supportive findings include: 1) signalment 2) recent fatty meal, 3)corticosteroid administration, 4) lipemia, 5) hypocalcemia, 6) elevated ALT, ALP, and bilirubin, and 7) hypercholesterolemia.
Acute vomiting: Case 1
Signalment
Toy poodle, FS, 15 months old
History
Vomiting for 1 week, associated with abdominal contractions
RX – Darbazine, amoxicillin, SC fluids
Initial clinical improvement then decompensation
Vomiting all food and water despite NPO status and IV fluids – vomitus contains blood
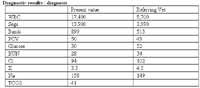
Labs: segs 3900, bands 513, glu 52, BUN 34, CL 102, K 4.5, Na 149, amylase 697, lipase 80
Physical examination
Moderate depression, 7% dehydration, mild pain in cranial abdomen
Acute vomiting
SELF-LIMITING - LIFE-THREATENING (CIRCLE ONE)
Differential diagnosis
Acute gastritis / enteritis
Dietary indiscretion
Gastric / duodenal foreign body
Gastric / duodenal ulcer
Diagnostic plan
CBC, biochemical profile, UA
Abdominal radiograph
Abdominal radiographs normal
Endoscopy – hemorrhagic area within duodenum, no foreign body seen
Exploratory celiotomy – 4-5 cm mass in pancreas
Histopathology – suppurative pancreatitis
Therapy
IV bolus 1g/kg 25% dextrose, NPO
IV 0.9% NaCl+2.5% dextrose+20mEq KCl/L
Cimetidine
Cephalothin
Case follow-up
Vomiting 3-8 times/day – despite acepromazine and metoclopramide SC and CRI
Day 2 endoscopy
Day 3 palpable pancreatic mass and surgery
Day 6 TPN
Day 10 sudden death
Necropsy – static suppurative pancreatitis
Selected References
Steiner JM, Newman SJ, Xenoulis PG, et. al. Sensitivity of serum markers for pancreatitis in dogs with macroscopic evidence of pancreatitis. Vet Therapeutics 9: 263-273, 2008.
Newman SJ, Steiner JM, Woosley, K, et. al. Localization of pancreatic inflammation and necrosis in dogs. J Vet Int Med 18: 488-493, 2004.
Mansfield C, Jones B. Plasma and urinary trypsinogen activation peptide in healthy dogs, dogs with pancreatitis and dogs with other systemic diseases. Aust Vet J 2000; 78: 416-422.
Hess RS, Kass PH, Shofer FS, et al. Evaluation of risk factors for fatal acute pancreatitis in dogs. J Am Vet Med Assoc 1999; 214: 46-51.
Hess RS, Saunders HM, Van Winkle TJ, et al. Clinical, clinicopathologic, radiographic, and ultrasonographic abnormalities in dogs with fatal acute pancreatitis: 70 cases (1986-1995). J Am Vet Med Assoc 1998; 213: 665-670.
Cook AK, Breitschwerdt EB, Levine JF, et al. Risk factors associated with acute pancreatitis in dogs: 101 cases (1985-1990). J Am Vet Med Assoc 1993; 203: 673-679.
7 Mulvany MH, Feinberg CK, Tilson DL. Clinical Characterization of Acute Necrotizing Pancreatitis. Comp Cont Educ Pract Vet 394: 394-407, 1982.
Murtaugh RJ. Acute Pancreatitis: Diagnostic Dilemmas. Sem Vet Med Surg 2: 282-295, 1987.
Hall JA, Macey DW. Acute Canine Pancreatitis. Comp Cont Educ Pract Vet 10: 403-417, 1988.
Simpson K, Batt R, McLean L, et al. Circulating concentrations of trypsin-like immunoreactivity and activities of lipase and amylase after pancreatic duct ligation in dogs. Am J Vet Res 50: 629-632, 1989.
Simpson KW. Current concepts of the pathogenesis and pathophysiology of acute pancreatitis in the dog and cat. Comp Cont Educ Pract Vet 2: 247-254, 1993
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen