Acute renal failure (Proceedings)
A guide to diagnosing and treating renal failure.
Renal disease overview
1. Renal insufficiency: 75-85% loss of renal function
2. Renal failure: 85+% loss of renal function
a. Acute
b. Chronic
c. Acute on chronic
Clinical signs of renal failure
1. Anorexia
2. Lethargy
3. Dehydration
4. Vomiting +/- Much less than dogs.
5. Diarrhea +/- Uncommon
Laboratory findings of renal failure
1. Elevated BUN and creatinine
2. Elevated serum phosphorus
3. Normal to decreased serum potassium
4. Decreased TCO2 and HCO3
5. Decreased urine specific gravity
Acute vs. chronic
1. Best single test to differentiate: PCV
a. Acute renal failure: PCV is normal
b. Chronic renal failure: PCV < 20%
2. Acute: disease onset is usually subacute to acute – days of illness instead of weeks of gradual decline.
3. Once Acute is established, you need to aggressively attempt to find the cause
Primary workup
1. To establish a diagnosis of acute renal failure
2. History of acute onset
3. Chem Profile: BUN, creatinine, phosphorus, potassium, TCO2-HCO3
4. CBC: PCV, WBC
5. Urinalysis: SG, bacteria, crystals
Secondary workup
1. Know what diseases are likely to cause acute renal failure
2. Divide them into Horses and Zebras
3. Concentrate on the Horses first
4. But, don't forget about the Zebras
5. Differential list: 4 Horses
a. Ethylene glycol (antifreeze)
b. Lily toxicosis
c. Pyelonephritis
d. Hydronephrosis secondary to ureteral obstruction
6. Differential list: 14 Zebras
a. NSAIDs
b. ACE inhibitors
c. Cholecalciferol rodenticide (Vitamin D toxicosis)
d. Antihypertensive drug
e. Renal lymphoma
f. Prolonged anesthesia
g. Aminoglycosides
h. Amphotericin-B
i. Radiographic contrast agents
j. Insect or snake venom
k. Acute pancreatitis
l. Heat stroke
m. Transfusion reaction
n. Melamine in tainted food (should not see again)
7. Ethylene glycol (antifreeze)
a. Exposure within the last 6 hours
b. Hypocalcemia
c. Calcium oxalate crystalluria
d. U/S: hyperechoic cortex and medulla (due to CalOx crystals) and medullary rim sign (MRS)
e. Positive ethylene glycol test
f. Recap: history, chemistry panel, urinalysis, renal ultrasound, EG test
8. Lily toxicosis
a. Within the last 4 days
b. Recap: history
9. Pyelonephritis
a. Painful kidneys/abdomen – usually
b. Radiographs – enlarge kidney(s). Normal sized kidneys when acute phase.
c. Excretory urogram – dilated renal pelvis
d. Ultrasound – enlarged kidney(s) with dilated, irregular renal pelvis (unless too acute)
e. Urinalysis – bacteria in sediment
f. Urine culture – positive growth
g. Recap: exam, radiographs, (excretory urogram), ultrasound, UA, U culture
10. Hydronephrosis due to ureteral obstruction
a. Painful kidneys/abdomen – usually
b. Radiographs – enlarged kidney(s); urolith(s) in ureter
c. Excretory urogram – no flow
d. Ultrasound – enlarged kidney(s) with dilated renal pelvis – may be extremely dilated
e. Recap: exam, radiographs, ultrasound
Summary: Secondary workup
1. Directed history taking
2. Physical examination – abdominal palpation
3. Abdominal radiographs
4. Excretory urogram – if no ultrasound
5. Renal ultrasound
6. Urinalysis
7. Urine culture
8. (Ethylene glycol test) if available and there is likely exposure
9. What if you do not have ultrasound?
10. Excretory urogram
a. Filtration of kidneys (cortex and medulla)
b. Flow ability (pelvis and ureters)
c. Dilated renal pelvis
d. If creatinine is > 15, it will probably fail due to lack of filtration
Treatment of acute renal failure
1. Expect hospitalization for 3-6 days.
2. Be frank about the cost for doing so.
3. Be frank about not achieving a cure – long-term treatment must follow.
4. IV fluids with KCl and NaHCO3 (if not hyperkalemic)
5. AlOH in food given by orogastric tube
6. Famotidine
7. Oral potassium (if not hyperkalemic)
8. Antibiotic pending culture
9. Success: converting this cat to Renal Insufficiency
a. This creates the need for long-term treatment at home.
Prognosis
1. Good if 1) the underlying problem is diagnosed and treated successfully, 2) the cat is not anuric or oliguric, 3) the owner has the financial resources, 4) you have the ability to offer aggressive therapy.
Renal insufficiency in cats
I much prefer creatinine over BUN
1. The BUN is influenced by many non-renal factors
a. High protein diet: increase BUN
b. GI bleeding: increase BUN
c. Increased protein catabolism: increase BUN
d. Corticosteroids, burns, fever, tetracycline
e. Dehydration: increase BUN
f. Prerenal renal failure: increase BUN
g. Polyuria: decrease BUN
h. Severe liver disease: decrease BUN
2. Creatinine is lowered when there is extreme weight loss to the point of emaciation.
Stages of renal disease
1. Renal insults
a. Bacterial infections, toxins, trauma, aminoglycosides, urethral obstruction, etc.
b. Generally, these result in loss of some renal function but it is less than 75% so the creatinine and USG remain normal.
c. There may be a few days of lethargy and anorexia but often PU/PD does not occur.
2. Renal insufficiency
a. Loss of 75-85% of renal function
b. Creatinine typically = 2.5-5.5 (when the normal range is up to 2.4)
c. No or mild clinical signs (which may be missed by the owners)
(1) PU/PD, reduced appetite, slight weight loss.
3. Renal failure
a. Loss of >85% of renal function
b. Lab findings
• Creatinine = 5.5 – 20
• Hyperphosphatemia
• Acidosis (+/-)
• Anemia of chronic disease
c. Clinical findings
• Anorexia, dehydration, very sick cat
• The clinical signs increase in severity as the creatinine rises.
Further diagnostics
1. All of these cats should have a urine culture
a. 22% positive: J Fel Med Surg April 07, p.124.
2. Ultrasound and possibly biopsy should be performed if:
a. The cat is less than 10 years of age.
b. One or both kidneys are enlarged.
c. One or both kidneys are painful.
3. Sizing kidneys
a. Palpation
b. Radiographs: Normal is 2.0-2.5 X the length of the body of L2.
c. Ultrasound: 38-42 mm in a young cat.
4. Urine culture – by cystocentesis.
5. Ultrasound
6. Biopsy
a. Indicated when the cat is < 10 years of age or the kidneys are enlarged.
b. Technique
• Confine the biopsy to the renal cortex.
• Direct the needle in a longitudinal plane.
• Consider a fine needle biopsy using a 22 gauge disposable needle.
Home maintenance
1. Indications
a. Cats presented for PU/PD and treated as above for renal insufficiency.
b. Cats treated for renal failure in the hospital and converted to renal insufficiency.
c. Cats diagnosed with renal insufficiency on geriatric profiles.
2. Expectations: to add 1-3 years of life to the cat.
3. Steps of Treatment
a. Renal diet
• Reduced protein (controversial)
• Reduced phosphorus
• Non acidifying
• Low sodium
• Good choices (because cats are so picky about what they eat)
o Purina: NF canned and dry
o Iams: Multistage Renal canned and dry
o Hill's: k/d canned (regular and minced) and dry
• Avoid diets that acidify the urine
o Aggravate acidosis
o Predispose the cat to calcium oxalate stones which are much more common in older cats than struvite stones.
b. Potassium orally: 2-4 mEq/d or 500-1000 mg/d
• Indication: Cats with renal insufficiency with serum K levels in the low half of the normal range or lower.
• The cycle:
o Renal failure causes polyuria.
o Potassium is lost in increasing amounts resulting in hypokalemia.
o Hypokalemia is harmful to the kidneys of the cat.
o Acidosis causes a shift of potassium from within the cells (where it works) to the blood.
o This results in muscle weakness in spite of improving potassium blood levels.

DiBartola in JAVMA, 3/1/93
"Chronic renal disease initiates a self-perpetuating cycle of declining renal function and increasing potassium depletion."
DiBartola in Sherding, 1994 ed.
"Potassium depletion leads to functional and morphologic abnormalities in the kidneys characterized by decreased GFR and defective renal concentrating ability." DiBartola in JAVMA, 3/1/93
"Dietary potassium supplementation may stabilize or improve renal function and should be a part of chronic renal disease management."
• Potassium tastes badly so administration can be a problem.
• You must find a method that is hassle-free or it will not be done long-term.
• Options
o Tumil-K: powder (good in canned food); tablets; gel
o Generic potassium gluconate (RenaCare)
o Compounded chewables
o Renal K powder; excellent palatability
o Pill Pockets: very well accepted by cats.
c. Subcutaneous fluids: by the owner or your technician
• 150 ml 2X per week; increase based on creatinine level and creatinine trend
• Use 18 gauge needles
• Potassium can be added to SQ fluids
o KCl up to 35 mEq per liter (more causes SQ inflammation)
o I recommend it if fluids are given 3X per week or more due to increased loss of potassium due to the amount of fluid being given.
o I consider it a replacement of this lost potassium and not a replacement for oral potassium.
d. Famotidine (Pepcid): PRN
• For appetite stimulation by resolving nausea that accompanies low gastric pH
• 2.5 mg q12h
e. Phosphate binder: PRN (usually not needed)
• Phosphate control
o Feed a renal diet for one month then check serum phosphorus level
- If < 5.0, no Pi binder is needed
- If 5.0+, use a Pi binder
- If the cat will not eat a renal diet or the owner will not feed a renal diet:
- If < 5.0, no Pi binder is needed.
- If 5.0+, use a Pi binder
o Phosphate binders
- If total calcium (or ionized Ca) is normal, any type is acceptable.
- If iCa is elevated, do not use a calcium-containing binder
- Ca acetate: PhosLo
- Ca carbonate: Epakitin
- Instead, use aluminum hydroxide
- Amphojel @ 100 mg/kg divided BID; available as 600 mg tablet; average dose: 1/2 tablet BID with food
- Spectrum Chemical (www.spectrumchemical.com); "AL226-500GM DRIED ALUMINUM HYDROXIDE GEL, POWDER, USP"; 500 gm for $81.30 + shipping (as of April 2009); Must be in each meal to bind the phosphates in that meal. Mix in canned food or "shake in a baggy" with dry food. Dose: 1/4 teaspoon per cat BID in food. Dose can be increased 2-4X if needed to reduce phosphorus to < 5.0. Tasteless but there will be a limit as to how much you can add to food without it reducing palatability of food. Can be placed in water or other liquid and syringed orally.
f. Drugs to increase food intake
• Famotidine (see above)
• Cyproheptadine
• Mirtazapine: 15 mg tablet: ¼ to 1/8 tablet q3d (benzodiazepine derivative)
• FortiFlora (Purina): sold for diarrhea control but some cats eat much better with it in their food.
• Benazepril (main "side effect" is appetite stimulation and weight gain).
g. Hypotensive agents
• About 20% of cats with renal insufficiency are hypertensive
• Amlodipine (Norvasc) is clearly the drug of choice.
• ACE-inhibitors will lower blood pressure but not very much
h. Benazepril
• AJVR, 3/01: Shown to slow progressive deterioration of the kidneys in cats.
• Actions (per Novartis)
o Inhibits the Renin-Angiotensin-Aldosterone System
o Vasodilation of the glomerular efferent arteriole
o Reduces glomerular pressure (relieves glomerular hypertension)
o Decreases protein loss
o Increases glomerular filtration leading to increased clearance of creatinine and urea.
• Dose: Up to 5 kg: 2.5 mg/q24h; Over 5 kg: 5 mg/q24h
• Watch for development of hyperkalemia (very unlikely)
i. Summary
• Level One
o Creatinine ~ 2.5-4.0
o Renal diet + potassium + benazepril
o Note: Do not begin potassium and benazepril at the same time or there is a good chance of anorexia. Make the transition to the new diet first, then add benazepril (or potassium). After it has been taken for one week, add potassium (or benazepril).
• Level Two
o Creatinine ~ 4.0-6.0 or increasing creatinine values over time
o Add SQ fluids to above
• Others: On a PRN basis.
4. Rechecks
a. Most vital tests: creatinine, phosphorus, calcium, potassium, PCV, blood pressure.
b. First should be 2 weeks after all recommendations are being performed
• May take 4-6 weeks.
• Primarily to check compliance as there should be no change in the creatinine level.
• Also, to check for hyperkalemia and hypercalcemia.
• Check blood pressure – first and with owner present.
c. Every 3 months thereafter.
d. I perform my rechecks in-house
• Takes less than 15 minutes of run time to get results.
• I go to another exam while it is running.
• This approach allows changes in the treatment protocol without having the client return.
• No phone call is needed the next day when you have forgotten the details of the case or when you have to
• leave a message.
5. Compliance
a. Differentiate insufficiency from failure
b. Have a plan and make it understandable
c. Make do-able recommendations
d. Plan rechecks (to check cat and owner compliance)
e. Give the client a reasonable goal
6. Microalbuminuria in cats
a. Elevated in the following (3 or more positives obtained 2 or more weeks apart)
• Primary renal disease
• Renal injury secondary to other systemic disease.
• Inflammatory disease, chronic infections, metabolic disease
• Hypertension, Cushing's Syndrome, Diabetes Mellitus, Hyperthyroidism
• Neoplasia
• False positives due to pyuria and gross hematuria.
ACEi for renal disease
The use of ACEi for renal disease is controversial because we do not have convincing data that they are either protective or detrimental to the kidneys. The following references are my basis for deciding to use benazepril in all my feline patients with renal insufficiency and renal failure. I have done so aggressively in hundreds of cats since the publication of Scott Brown's paper in 2001. Based on my experience I am absolutely convinced that benazepril is not harmful to the kidneys. Whether or not it is beneficial is yet to be determined. Only further research will ultimately resolve this controversy.
Use in humans
1.) Journal of the American Society of Nephrology, April 1999, Vol. 10, Supplement 12, pp. S283-S286.
Mackenzie HS, Zial F, Omer SA, Nadim MK, Taal MW. Angiotensin Receptor Blockers in Chronic Renal Disease: The Promise of a Bright Clinical Future.
"Pharmacologic interruption of the renin-angiotensin system (RAS) with angiotensin-converting enzyme inhibitors (ACEi) is considered a standard therapeutic intervention for patients with chronic renal disease, regardless of whether systemic hypertension is present."
Use in canines
1. )Journal of the American Veterinary Medical Association, April 15, 2009, Vol. 234, pp. 1031-1037.
Tenhundfeld J, Wefstaedt P, Nolte JA. A randomized controlled clinical trial of the use of benazepril and heparin for the treatment of chronic kidney disease in dogs.
Results
Health status score at the end of the study (ie, day 180) was significantly higher for dogs in the 2 treatment groups than for dogs in the placebo group. In addition, glomerular filtration rate was significantly increased and the urine protein-to-creatinine ratio was significantly decreased, compared with baseline rates, at the end of the study for dogs in both treatment groups but not for dogs in the placebo group. Systolic and diastolic blood pressures were significantly decreased on day 6 for dogs in both treatment groups."
Conclusions and clinical relevance
Results suggested that administration of benazepril had beneficial effects in dogs with chronic kidney disease but that short-term administration of heparin in conjunction with benazepril did not appear to provide additional benefit."
"In the benazepril group, the significant increase in glomerular filtration rate from day 30 on was associated with transient significant decreases in plasma urea nitrogen and creatinine concentrations on day 90. For dogs in both treatment groups, glomerular filtration rate was significantly increased, compared with baseline rates, on days 30, 90, and 180, but no change in glomerular filtration rate was detected for dogs in the placebo group. This suggested that benazepril administration had a positive effect on glomerular filtration rate and is in accordance with results of previous studies in which ACEIs were found to reduce glomerular capillary hypertension and decrease the release of extracellular matrix and collagen from mesangial and tubular cells, potentially decreasing glomerular interstitial fibrosis."
"Our findings are similar to findings of a previous study in cats in which cats with CKD treated with benazepril for 12 to 24 weeks had had significant decreases in serum and creatinine and urea nitrogen concentrations."
2.) Journal of Veterinary Internal Medicine, July 2008, Vol. 22, pp. 905-914.
Pouchelon JL, Jamet N, Gouni V, Tissier R, Serres F, Sampedrano CC, Castaignet M, Lefebvre HP, Chetboul V.
Effect of Benazepril on Survival and Cardiac Events in Dogs with Asymptomatic Mitral Valve Disease: A Retrospective Study of 141 Cases.
"Interestingly, the present study shows that, similar to enalapril, BNZ had a significant effect on all-cause death in both the whole and OB populations (whereas the effect on cardiac death was observed only in the OB population.) Several possible mechanisms may explain these noncardiac beneficial effects. First, renal dysfunction was recently identified in dogs with MVD, and ACEIs have been shown to exert a renoprotective action owing to decreases in systemic arterial pressure, glomerular capillary pressure, and glomerular volume together with an increase in glomerular filtration rate."
Use in felines
1.) American Journal of Veterinary Research, March 2001, Vol. 62, pp. 375-383.
Brown SA, Brown CA. Jacobs G, Stiles J, Hendi RS, Wilson S. Effects of the angiotensin converting enzyme inhibitor benazepril in cats with induced renal insufficiency.
Results
Compared with cats that received placebo, mean systolic arterial blood pressure was significantly less and GFR significantly greater in cats that received benazepril. Glomerular capillary pressure and the ratio of efferent to afferent arteriolar vascular resistance were also significantly less in treated cats. However, histologic differences in renal specimens were not detected." (Benazepril was given for approximately 6.5 months.)
Conclusions and clinical relevance
Treatment with benazepril sustained single nephron GFR in remnant nephrons of cats with induced renal insufficiency. Administration of benazepril was also associated with a small but significant reduction in degree of systemic hypertension and an increase in whole kidney GFR. Benazepril may be an effective treatment to slow the rate of progression of renal failure in cats with renal disease."
2.) Journal of Veterinary Internal Medicine, July 2008. Vol. 22, pp. 1103-1110.
Lapointe C, Belanger MC, Dunn M, Moreau M, Bedard C.
N-Acetyl- -D-Glucosaminidase Index as an Early Biomarker for Chronic Kidney Disease in Cats with Hyperthyroidism.
"Renal hemodynamic changes, such as those observed in hyperthyroidism, can result in damage to the nephrons by various mechanisms. The 1st process by which damage is thought to be induced is increased angiotensin II (AII) concentrations in the hyperthyroid state. Increased AII activity leads to increased transforming growth factor 1 and platelet derived growth factor in rats. These changes could result in interstitial fibrosis and matrix protein accumulation and eventually lead to tubulointerstitial nephritis. The 2nd possible harmful process is increased proteinuria, which has been observed in humans with hyperthyroidism as well as in some cats in our study. Proteins that penetrate into the glomerular lumen are primarily reabsorbed by the proximal tubular epithelial cells. Proteinuria can induce proximal tubular damage by direct cytotoxic effects on tubular epithelial cells with proteins in the tubular lumen are reabsorbed."
3.) Proceedings, State of the Art in Renal Disease in Cats and Dogs, Nice 2007, pp. 24-29.
Grauer GF.
Note that primary renal disease can lead to systemic hypertension and activation of the RAAS both of which can lead to intra-glomerular hypertension that can lead to progressive loss of nephrons without proteinuria.
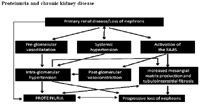
Proteinuria and chronic kidney disease
Final question
Is proteinuria simply a marker of CKD that is more likely to be rapidly progressive or does proteinuria mediate progressive renal injury? If the latter is true, treatments that attenuate proteinuria are likely to be renoprotective and improve survival. Another possibility is the intraglomerular hypertension is a major mediator of progressive renal damage in CKD and that proteinuria is simply a consequence of this intraglomerular hypertension."
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen