Blood gas analysis made easy (Proceedings)
Blood gas analysis provides information about respiratory function and acid/base status.
Blood gas analysis provides information about respiratory function and acid/base status. This information is vital in determining and monitoring treatment of patients with primary or secondary respiratory disease and/or metabolic disturbances. Blood gas (BG) can be assessed on arterial (ABG) or venous (VBG) samples, although oxygenation assessment is made on arterial blood only. Specifically, ABG assessment describes the degree of hypoxemia and hyper or hypocapnea associated with respiratory disease. These assessments may be used to determine the need for oxygen supplementation or mechanical ventilation. Evaluation of arterial or venous blood gases also determines whether the patient suffers from any of the acid/bas disturbances. Hydrogen ion concentration determines acid/base status and is described by blood pH. The body's major regulation of pH is performed by the lungs which regulate carbon dioxide (CO2) and the kidneys which regulate bicarbonate (HCO3). Disturbances in lung function may result in respiratory acidosis or alkalosis. Disturbances in kidney function may result in metabolic acidosis or alkalosis. Since both organ systems work in concert to regulate blood pH, it is common to see respiratory abnormalities to compensate for metabolic disturbances and visa versa.
Respiratory Acidosis is caused by an increase in carbon dioxide (CO2). Hypercapnea may be due to CNS disease, anesthesia, respiratory muscle weakness, etc.
- Respiratory Alkalosis is caused by decreased CO2. Hypocapnea may be due to excessive panting, heat stroke, compensation for metabolic acidosis, etc.
- Metabolic Acidosis is caused my excessive loss of bicarbonate (HCO3). This may be due to renal failure, diabetic ketoacidosis, various toxic agents, etc.
- Metabolic Alkalosis is caused by excessive HCO3 retention or resorption. This may be due to GI disease
Simple 5 step blood gas analysis
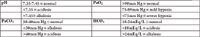
It is easy to perform a quick ABG interpretation by following 5 steps. The normal ranges for each of the basic elements are:
5 steps of basic abg interpretation
1. Evaluate the PaO2 and determine if the patient is hypoxemic (needs oxygen).
2. Evaluate the pH and determine if the patient is normal, acidotic or alkalotic.
3. Evaluate the PaCO2 and determine if it supports the pH findings. (if YES then the condition is primarily respiratory, if NO the condition is not primarily respiratory).
4. Evaluate the HCO3 and determine if it supports the pH findings. (if YES then the condition is primarily metabolic, if NO the condition is not primarily metabolic).
5. Evaluate the parameter NOT responsible for abnormal condition to assess for compensation
A pH in the normal range does not necessarily indicate the absence of acidosis or alkalosis, as an abnormal PCO2 or HCO3- may be due to compensatory mechanisms or multiple simultaneous pathologies which "balance" each other. The clinician must therefore be vigilant in reading the entire blood gas. Lastly, many blood gas analyzers have the capability to measure electrolytes and lactate. These values are also imperative in evaluating and understanding the acid-base abnormality or severity of hypoperfusion (lactate). Please see proceedings specific for lactate analysis for further information.
Causes for metabolic acidosis (with a normal anion gap)
- GI loss of bicarb
o Diarrhea
o Vomiting
- Renal loss of bicarb
- Renal hydrogen retention
- IV nutrition
- Dilutional acidosis
Causes for metabolic alkalosis
- Lasix administration
- Pyloric outflow obstruction
- Hypochloremia
- Hypokalemia
- Hypermineralocorticism
- Penicillin derivatives
- Contraction alkalosis
- Excessive alkalinization therapy
Causes for respiratory acidosis
- Hypoventilation
o Neuromuscular
o Medullary dysfunction
o General anesthesia
o Intracranial disease
o Cervical disease
- Airway obstruction
o Large airway obstruction
o Laryngeal paralysis
o Tracheal collapse
o Small airway obstruction
o Chronic airway disease
o Bronchoconstriction
- Thoracic wall problems
o Open pneumothorax
o Flail chest
o Diaphragm compression
o Pleural space filling disorder
o Pleural fibrosis
- Pulmonary parenchymal disease (late)
- Inappropriate vent settings
- Dead space re-breathing
- Bicarb therapy
- Compensation for metabolic acidosis
- Malignant hyperthermia
- Brain tumor
Causes for respiratory alkalosis
- Hypotension
- Fever
- Sepsis
- Excitement
- Pain
- Brain tumor
- PTE
- Early pulmonary parenchymal disease
- Cytokine release in SIRS
- Inappropriate ventilator settings
- Compensation for metabolic acidosis
References available upon request
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen