Canine and feline histoplasmosis: A review of a widespread fungus
Infection with the pathogenic fungus Histoplasma capsulatum can result in systemic disease in several species of animals, including dogs and cats.
Infection with the pathogenic fungus Histoplasma capsulatum can result in systemic disease in several species of animals, including dogs and cats. While the exact prevalence of this infection is unknown for these animals, large areas of endemicity exist throughout the world. In the United States, the largest number of cases occurs in the Ohio, Missouri, and Mississippi river valleys. One study reported histoplasmosis as the second most common fungal infection in cats.1 Infected dogs and cats may present with a myriad of clinical signs, commonly including pyrexia, anorexia, and lethargy. Histoplasmosis is an important differential diagnosis to consider in animals from endemic areas.
DISCOVERY
Histoplasmosis was first described at the Panama Canal in 1905 by the American physician Samuel Darling.2 During an autopsy of a patient suspected of having miliary tuberculosis, microscopic examination revealed intracellular organisms in many tissues, including the lungs. Because of the organisms' encapsulated appearance, resemblance to plasmodia, and location within histiocytes, Darling named the agent Histoplasma capsulatum. Thinking that he had identified a new form of visceral leishmaniasis, Darling incorrectly identified the organism as protozoal. In 1912, the Brazilian physician and pathologist Henrique da Rocha-Lima reviewed Darling's slides and suspected the organism was a yeast.2
In 1934, pathologist William DeMonbreun successfully cultured and identified the organism H. capsulatum from the blood of an infected person. DeMonbreun subsequently reported naturally occurring histoplasmosis in a dog in 1939.3 In 1948, the organism was isolated in soil contaminated with chicken excrement.4,5 The first reported case of feline histoplasmosis was in 1949.6

The biological basics of Histoplasma species
CLINICAL OUTCOME
Histoplasmosis may have an acute or chronic clinical course.7-9 Depending on the fungal inoculum size and host immunocompetence, H. capsulatum infections may result in subclinical infection, dormant infection with subsequent reactivation and dissemination, or pulmonary or disseminated histoplasmosis.10-13
CLINICAL FINDINGS
Although histoplasmosis has been reported in dogs from 5 months to 11 years old,8,9 it is most commonly seen in dogs < 4.11 No consistent sex predilection has been documented. Male dogs have been reported to be 1.2 times more frequently affected than females,11,14 while in other reports, females are more frequently affected than males.8,9 One study reported that pointers, Weimaraners, and Brittany spaniels had an increased risk of histoplasmosis.11,14
Once thought to be rarely affected, cats are now considered as likely as dogs to develop clinical histoplasmosis.10,11,15 In a retrospective study of 571 cats with deep mycotic infections, histoplasmosis was the second most commonly reported fungal infection (16.7% of cases) after cryptococcosis (46.1% of cases). The reported age of cats with histoplasmosis ranged from < 2 months to > 15 years, with most cases occurring in cats < 2 years old. Males and females were affected in about equal numbers, which1 contrasts with a previous study of 18 cats with pulmonary histoplasmosis in which females outnumbered males 2 to 1.16 Thus, as in dogs, conclusions regarding sex predilection in feline histoplasmosis cannot be drawn.
In a review of 96 cats with histoplasmosis, Persians and Siamese were found to be overrepresented and underrepresented, respectively; this has not been reported elsewhere in the literature.1 Of these 96 cats, 15% had positive test results for feline leukemia virus (FeLV) infection.1 In contrast, a previous retrospective study of 12 cats with disseminated histoplasmosis revealed no association between FeLV infection and histoplasmosis.15
CLINICAL SIGNS
The clinical signs seen in dogs and cats with histoplasmosis vary depending on which form of infection has taken root.
Pulmonary histoplasmosis
Acute pulmonary histoplasmosis in dogs and cats is thought to be uncommon. In dogs, this form is characterized by a rapid onset of dyspnea and cyanosis. Dogs with chronic pulmonary histoplasmosis are presented for evaluation of a mild, chronic cough and a history of weight loss and inappetance.7 Coughing may be due to partial airway obstruction secondary to hilar lymphadenopathy.17 Most affected cats have disseminated disease, and, even with evidence of pulmonary involvement, they seldom cough.10,11,18 Other clinical signs of respiratory tract involvement include dyspnea and tachypnea.11
Canine disseminated histoplasmosis
Acute disseminated histoplasmosis affects multiple organs, with a history of illness of only a few days' duration in experimental animals.19 Gastrointestinal involvement was reported in 28 of 36 (78%) dogs with chronic disseminated histoplasmosis.8,9 Large bowel diarrhea, characterized by hematochezia, mucus, and tenesmus, is common.11 With disease progression into the small intestine, diarrhea may become watery and voluminous, and protein-losing enteropathy may occur.8-11
In addition to gastrointestinal signs, common nonspecific clinical signs of chronic disseminated histoplasmosis in dogs include weight loss, inappetence, and fever of unknown origin that is nonresponsive to antibiotic therapy.7-11,20
Abnormal lung sounds, with or without accompanying cough or dyspnea, are noted in fewer than 50% of dogs with disseminated histoplasmosis.11 Infiltration of the organism into other organs, including the liver, spleen, and bone marrow, may result in hepatomegaly, splenomegaly, or pallor associated with anemia.8,9 Less commonly reported clinical findings of canine disseminated histoplasmosis include
- Vomiting21-23
- Peripheral lymphadenopathy10,11,24,25
- Polyarthropathy or fungal osteomyelitis10,11,26,27
- Ulcerated dermal nodules, sores on footpads, or draining abscesses10,21,28-32
- Neurologic signs, including seizures and vertical nystagmus33
- Oral lesions, including gingival nodules and lingual erosions21,31
- Conjunctivitis, chorioretinitis, retinal detachment, or optic neuritis26,34
- Icterus9
- Pleural and peritoneal effusion7,23,35
Feline disseminated histoplasmosis
Clinical signs of feline disseminated histoplasmosis are often chronic and nonspecific. Weight loss, pale mucous membranes, lethargy, pyrexia, anorexia, and dehydration were the predominant findings in 12 cats with disseminated histoplasmosis. Five of the 12 cats were tachypneic with abnormal lung sounds.15 A review of 96 cases reported weakness, lethargy, emaciation, dehydration, and pyrexia as the most common signs.1 Respiratory signs such as dyspnea, tachypnea, and occasional coughing were noted in 39% of the cats.1
While sometimes reported to be uncommon, ocular involvement may occur in disseminated histoplasmosis more often than in other systemic mycoses in cats.1,36 In a review of 96 cats with histoplasmosis, 24% of the cats had ocular involvement including chorioretinitis, anterior uveitis, or retinal detachments.1 Granulomatous chorioretinitis occurs, possibly because of H. capsulatum in the choroid and retina.34,37 Additional ocular involvement may include retinal hemorrhage, optic neuritis, and fungal granulomas.15,38,39
About one-third of affected cats may have lymphadenopathy, splenomegaly, or hepatomegaly, occasionally accompanied by icterus.11 In contrast to dogs, primary intestinal histoplasmosis is unusual in cats; in one cat, this form of histoplasmosis caused vomiting and watery diarrhea with hematochezia.40
Cutaneous lesions, infrequently reported, are nodular or ulcerated and may exude serosanguineous fluid.11,32,38,41-44 Neurologic signs also occur.45 Rare clinical findings include nasal polyps and oral and lingual ulceration.10,11
CLINICAL PATHOLOGY AND DIAGNOSTIC IMAGING FINDINGS
The results of routine diagnostic tests such as a complete blood count, a serum chemistry profile, a urinalysis, and radiographic or ultrasonographic examinations may raise your suspicion of histoplasmosis.
Complete blood count
The most common hematologic abnormality in dogs and cats with disseminated histoplasmosis is a normocytic, normochromic nonregenerative anemia.10,11,46 Anemia in dogs is usually mild to moderate; the packed cell volume (PCV) ranges from 20% to 37% (reference range = 35% to 57%47).8 In a report of 12 cats, anemia ranged from moderate (PCV = 20% to 25%) to severe (PCV < 20%) (reference range = 30% to 45%47).15 Causes of anemia may include intestinal blood loss, chronic inflammation, or bone marrow infiltration.8,11,30
Other hematologic abnormalities reported in dogs include monocytosis, neutrophilia, eosinopenia, and, less commonly, neutropenia, eosinophilia, basophilia, or a degenerative left shift.8-11,35,48,49 While infrequently observed, histoplasmosis is reported as a risk factor for neutropenia.48 Mild to severe thrombocytopenia may occur in as many as half of affected dogs.11 In a report of three dogs with histoplasmosis, platelet counts ranged from 5,000 to 81,000/mm3 (reference range = 211,000 to 621,000/mm3). Thrombocytopenia may be caused by increased platelet consumption or, possibly, sequestration in association with splenomegaly and hepatomegaly.46
A wide range of other hematologic abnormalities also occur in cats. Both neutropenia and neutrophilia have been reported,1,18,38,50 and pancytopenia was documented in one cat with toxic changes to the neutrophils.18 Thrombocytopenia may be observed in as many as one-third of affected cats.11 Chronically infected cats may not show any hematologic abnormalities.38
Serum chemistry profile
Hypoalbuminemia was reported in five of five cats and nine of 11 dogs with disseminated histoplasmosis.8,15 The hypoalbuminemia may result from intestinal blood loss, decreased synthesis associated with inflammation, liver dysfunction, or protein-losing enteropathy.8-11,15 Hyperglobulinemia secondary to inflammation is reported in dogs and cats.8,10,15,33,38 Hepatic involvement can result in increased serum alanine aminotransferase (ALT) activity, alkaline phosphatase activity, and total bilirubin concentration.8,9,11,38 Hypercalcemia has been reported in cats with histoplasmosis.38
Urinalysis
While proteinuria has been reported,8,38 urinalysis results in dogs and cats with histoplasmosis are usually within reference ranges.10,50
Thoracic radiography
Dogs. Common thoracic radiographic abnormalities in canine pulmonary histoplasmosis include hilar lymphadenopathy and a bronchial-interstitial or interstitial pattern (Figures 1A & 1B).10,51 Mineralization of lymph nodes and pulmonary infiltrates is occasionally observed and may indicate inactive disease.7,10,11,17,20 Pleural effusion and sternal lymph node enlargement are infrequently observed.17,23,35 Additional unusual findings include a focal alveolar opacity affecting one lung lobe and a fungal granuloma in the thoracic cavity cranial to the heart.35,52

1A & 1B. Lateral and ventrodorsal thoracic radiographs of a 7-year-old American cocker spaniel with pulmonary histoplasmosis. A heavy unstructured interstitial-to-coalescing nodular interstitial pattern is seen throughout all lung fields in both views, partially obscuring the pulmonary vessels.
Cats. Unspecified thoracic radiographic abnormalities were present in 27 of 31 (87.1%) cats with disseminated histoplasmosis.1 An interstitial miliary pattern was the most common radiographic abnormality in a study of 12 cats.15 Radiographic patterns in cats with pulmonary histoplasmosis include a fine, diffuse or linear interstitial infiltrate; nodular interstitial infiltrate; or, rarely, alveolar pattern.16,53,54 Enlarged or mineralized tracheobronchial lymph nodes were not a feature of feline pulmonary histoplasmosis.16 Areas of pulmonary consolidation were reported in one cat.54
Abdominal radiography and ultrasonography
Abdominal radiographs in dogs and cats may show hepatomegaly or splenomegaly; ascites was reported in one dog.9,10,15,35,55 On abdominal ultrasonographic examination, the affected liver may have a hyperechoic appearance, as well as nodular lesions.10,36,55 Lymphadenomegaly may also be observed.9
Skeletal radiography
Dogs. Bony lesions of histoplasmosis are rarely reported in dogs; affected sites include the tibia and tarsal, carpal, and metacarpal bones.26,27,56,57 Radiographic abnormalities include soft tissue swelling and joint effusion with osteolysis and proliferative sclerosis.26,56
Cats. In a review of 96 cases of feline histoplasmosis, all seven cats with lameness had changes consistent with osteomyelitis on long bone radiographs.1 Multiple long bones, as well as carpal and tarsal bones, may be affected.38,43,44,58 A predilection for sites distal to the elbow and stifle joints exists.43 Lesions are predominantly osteolytic, with periosteal and endosteal proliferation seen in some cases.43 Bone weakening can result in pathologic fractures that heal after treating the disease.43,44 Additional radiographic changes reported in one cat included soft tissue swelling and subchondral bone collapse.58
DEFINITIVE DIAGNOSIS
Histoplasmosis is commonly diagnosed by identifying the H. capsulatum organism.7,11,51,59
Cytology and histology
Histoplasma capsulatum organisms can be identified by using Wright's-Giemsa stain or a modified Wright's stain.11,50,53 Histoplasma capsulatum are oval or round 2- to 4-µm-diameter organisms that are found within macrophages.10,11,35 The yeast cells have a basophilic center surrounded by a clear area caused by shrinkage of the cell away from the cell wall during fixation (Figure 2).11,24,31,34 During the preparation process, H. capsulatum organisms may be released from cells and appear free on the slide.11,24
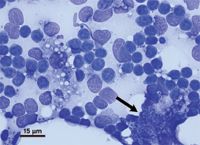
2. A lymph node aspirate from a cat. A single large macrophage is densely packed with yeast (arrow), and numerous yeast organisms are free in the background. Note the clear area surrounding the yeast, caused by shrinkage that occurs during fixation. Numerous small lymphocytes and a few bare nuclei are also present (Diff-Quik, 100X).
When a peripheral blood smear is examined, identifying H. capsulatum is enhanced by examining the buffy coat.7,10,18,38,53 Histoplasma capsulatum has been documented in the neutrophils (Figure 3), monocytes, and, rarely, eosinophils of affected dogs.10,30,35,46,49 A review of cats with histoplasmosis reported the organism within phagocytic cells in peripheral blood smears in 11 of 56 (19.6%) cases.1 In a separate study, examination of peripheral blood smears revealed the organism in four of 12 (33%) feline cases.15

3. A canine peripheral blood smear demonstrating two segmented neutrophils that contain several budding yeast (modified Wright's stain, 100X).
Histoplasma capsulatum organisms are also identified on cytologic evaluation of fine-needle aspirates or impression smears of tissue (Table 1; Figures 2, 4-5).8,15,38,58 Bone marrow aspirates can be diagnostic in feline disseminated histoplasmosis. In retrospective studies, diagnoses were obtained through bone marrow aspirates in 14 of 16 (87.5%) and 11 of 12 (91.7%) cats.1,15 Rectal scrapings (Figure 6) may be diagnostic in dogs with disseminated histoplasmosis; a diagnosis was made in seven of 24 (29%) dogs based on cytologic evaluation of rectal mucosa.8,9 Similarly, H. capsulatum was identified on cytologic or histologic examination of rectal or intestinal mucosa in seven of 12 (58%) dogs with disseminated histoplasmosis.8

4. A liver aspirate from a cat. Three dark-purple hepatocytes are seen among multiple macrophages, some of which contain yeast (arrows). Several yeast are noted free in the background (arrowheads) of erythrocytes and a small amount of finely granular protein (Diff-Quik, 60X).
When indicated, cytologic analysis of pleural or peritoneal effusions, synovial or cerebrospinal fluid, or tracheal or bronchoalveolar fluid can be helpful.11,23,25,33,38,41,58,60 During bronchoscopy of affected dogs, mild to severe compression of the mainstem bronchus may be seen secondary to hilar lymphadenopathy, affecting both the left and right principal bronchi.17

5. A lung aspirate from a cat. Multiple foamy activated macrophages are noted, including a single giant cell on the far left. One macrophage contains several yeast (arrow). Several yeast are noted in the background (arrowheads) of erythrocytes and a small amount of finely granular protein. Also note the morphologically normal respiratory epithelial cells with their tufts of apical cilia to the right of the micrometer (Diff-Quik, 60X).
Histologic evaluation of affected tissues often shows granulomatous or pyogranulomatous inflammation with intracellular organisms. Histoplasma species organisms are not well-visualized with routine hematoxylin-eosin stain. Periodic acid-Schiff, Gridley's fungal, or Gomori methenamine silver stains should be used to enhance detection.10,11 Histoplasma capsulatum has been identified antemortem by histologic examination of several tissues (Table 1).
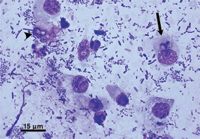
6. A rectal scraping from a dog. A mixture of individualized epithelial cells and macrophages are seen in a moderately heavy background of mixed bacteria. Yeast are seen within macrophages (arrow) and are free in the background (arrowhead) (Diff-Quik, 100X).
Fungal culture
A definitive diagnosis may be made through fungal culture of tissue, body fluid, or fine-needle aspirates of affected organs.10,11 However, culturing H. capsulatum outside of professional diagnostic laboratories is not recommended, as incubation at room temperature can result in the growth of the mycelial phase within seven to 10 days, posing a risk for personnel.10 In addition, fungal cultures may be falsely negative,10,61-63 and growth of H. capsulatum may require up to four weeks.
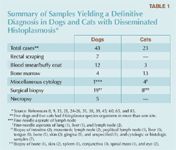
Table 1. Summary of Samples Yielding a Definitive Diagnosis in Dogs and Cats with Disseminated Histoplasmosis
Polymerase chain reaction testing
To date, polymerase chain reaction (PCR) testing has been used primarily in research settings to confirm a diagnosis of histoplasmosis. A nested PCR technique has been applied in situ to DNA extracted from pus and paraffin-embedded tissue samples of dogs with histoplasmosis.64,65 PCR testing is not commercially available for diagnostic testing for histoplasmosis in cats and dogs.
Serology
In people, standard serologic tests include complement fixation and immunodiffusion, which use yeast and mycelial antigens to detect antibodies against H. capsulatum.61 Complement fixation is more sensitive.62 However, when complement fixation was performed in nine cases of canine histoplasmosis, only one titer of 1:8 was obtained.9 Similarly, serologic testing performed in nine cats with histoplasmosis had positive results in only four of the cats (44%).1 Because of a myriad of false negative and false positive results, serology for antibody detection is not considered a reliable method of diagnosis in cats and dogs.10,11
Antigen detection tests are used to detect histoplasmosis in human serum, urine, bronchoalveolar lavage fluid, and cerebrospinal fluid.63 Cross reactivity occurs with other agents of disseminated mycoses, such as Blastomyces species.66 Research on the use of antigen detection tests to diagnose canine and feline histoplasmosis is limited. Full validation of these tests for dogs and cats is pending.
TREATMENT
Although canine pulmonary histoplasmosis may be self-limiting and resolve without treatment,7 antifungal therapy is recommended because of the risk of dissemination (Table 2).10,36 In people, itraconazole is the first-line treatment for mild to moderate pulmonary or disseminated histoplasmosis, and amphotericin B is the first-line treatment for severe pulmonary or disseminated histoplasmosis.67 Itraconazole or amphotericin B is considered the first-line treatment for histoplasmosis in dogs and cats.10
Table 2. Common Antifungal Treatments for Histoplasmosis in Dogs and Cats
Itraconazole
Even though itraconazole is reportedly the treatment of choice for histoplasmosis in dogs and cats,10,38 few reports of specific studies of its efficacy in these species exist. One report indicated good efficacy in eight cats treated with itraconazole (5 mg/kg orally b.i.d.) for 60 to 130 days, with two cats relapsing and requiring additional therapy to achieve complete remission.38 Because of marked variability in the oral absorption of itraconazole, some cats may require twice-daily dosing at 10 mg/kg.68 Different formulations of itraconazole exist (Table 2); of these, the oral suspension has the greatest bioavailability.22,68,69 Use of the intravenous formulation of itraconazole may be considered in animals that cannot be treated with an oral formulation. However, little data exist on the use of intravenous itraconazole in dogs and cats.22,69
Fluconazole
No studies evaluating fluconazole therapy in dogs and cats with disseminated histoplasmosis exist. But since fluconazole has increased penetration into the eye and central nervous system, it may theoretically be a better azole agent for patients that have neurologic or ocular involvement refractory to itraconazole.10 Results of an in vitro study showed that fluconazole had a higher minimal inhibitory concentration than itraconazole for Histoplasma species.70 However, in people, fluconazole is considered a second-line treatment for histoplasmosis,67 and in mice with experimentally induced Histoplasma species meningitis, fluconazole monotherapy was less efficacious than itraconazole or amphotericin B monotherapy.71

Case example: Histoplasmosis in a Himalayan Cat
Ketoconazole
Successful treatment of feline histoplasmosis with varying dosages of ketoconazole has been reported.18,44,50 However, because of its reduced spectrum of activity against Histoplasma species and increased relative toxicity, ketoconazole is not a first-choice treatment.10
Voriconazole and posaconazole
Voriconazole, a triazole structurally related to fluconazole,72 and posaconazole, a triazole structurally related to itraconazole, also have activity against H. capsulatum. There are not sufficient data regarding the safety and efficacy of these newer agents in dogs and cats to warrant recommending their use. They may be considered as rescue therapy for patients in which other treatments have failed. Pharmacokinetic data for these agents in dogs are available.73,74
Amphotericin B
In dogs and cats with severe disseminated or pulmonary histoplasmosis, amphotericin B or combination therapy with amphotericin B and itraconazole may provide more effective control.10 Itraconazole treatment is started at the same time as amphotericin B and is continued for the normally recommended duration of treatment (Table 2) after amphotericin B treatment is terminated. Although typically administered intravenously, subcutaneous amphotericin B has been used to treat cryptococcosis.75
Nephrotoxicosis is an important adverse effect of amphotericin B therapy, particularly when the deoxycholate form is used. Since urine changes may precede serum elevations in urea nitrogen and creatinine, serial evaluation of urine specific gravity and monitoring for evidence of casts, protein, or hematuria should be performed.22 Because of their comparatively reduced nephrotoxicity, the lipid and liposomal forms of amphotericin B are preferred, and should be considered when amphotericin B treatment is indicated.76,77
While the lipid and liposomal forms of amphotericin B are more expensive, this increased expense must be considered in light of increased safety. The financial and health costs of toxicosis related to using the deoxycholate form may be as much or more of a burden than the additional cost of the lipid forms.78
Supportive therapies
Because of the risk of immunosuppression and subsequent dissemination of infection, glucocorticoids are generally not recommended in treating histoplasmosis. However, airway obstruction from enlarged hilar lymph nodes and inflammation associated with proliferation of the organism in the lungs can be life-threatening.10 In a study of dogs with enlarged hilar lymph nodes secondary to chronic pulmonary histoplasmosis, corticosteroid administration (prednisone 2 mg/kg orally every 12 to 24 hours) resulted in the resolution of the clinical signs of airway obstruction in less than one week, compared with 8.8 weeks in dogs treated with antifungal therapy.17 Only consider using corticosteroids if there is marked respiratory compromise and if no organisms are found on cytologic or histologic evaluation. Additional supportive therapy for pulmonary histoplasmosis may include oxygen supplementation and antibiotics, if clinically indicated.11
TREATMENT DURATION AND MONITORING
While the duration of therapy is variable, most patients treated with antifungal drugs will receive these medications for a minimum of four to six months or two months after resolution of all clinical signs.10 Patients should be rechecked at monthly intervals. In addition to physical and ocular examinations, a serum chemistry profile is recommended to monitor hepatic enzyme activity while an animal is receiving azole antifungal therapy.11 In a study of 112 dogs treated with itraconazole, anorexia was the most common adverse effect and was usually associated with an increase in ALT activity. The anorexia resolved within three or four days after the medication was stopped, and therapy was reinstituted one week after discontinuation.79 In dogs, if the serum ALT activity is > 250 IU/L, consider discontinuing itraconazole therapy.80 In dogs and cats with anorexia and increased ALT activity, treatment can be resumed at half the original dose once the anorexia resolves or the hepatic enzyme activity returns to reference values.22,81 Similar recommendations apply for animals exhibiting signs of cutaneous vasculitis.81
Response to therapy should be evaluated through the resolution of clinical signs, hematologic and biochemical abnormalities, and radiographic lesions.10 Treatment is continued for a minimum of one month past resolution of clinical signs, and animals should be reevaluated for evidence of relapse three and six months after therapy is discontinued.11
PROGNOSIS
The prognosis depends primarily on the extent and severity of infection. Pulmonary histoplasmosis may resolve without specific antifungal therapy,82 and dogs and cats with pulmonary histoplasmosis can have a good prognosis. The prognosis for disseminated histoplasmosis depends on the degree of dissemination and severity of clinical signs.10,11 While central nervous system involvement often carries an unfavorable outcome,33,34 recovery of neurologic function is possible.45
With ocular involvement, the prognosis for return of vision is guarded to poor.37 One recent report of feline ocular histoplasmosis documented return of vision with complete resolution of retinal hemorrhages six months after the initiation of systemic itraconazole therapy in a cat.39
PREVENTION
Vaccination against histoplasmosis is not available in cats and dogs, so the recommended method of protection is preventing exposure to potentially Histoplasma species-laden areas, such as chicken coops, bird and bat roosts, and construction and excavation sites.4,10
SUMMARY
Histoplasma capsulatum is a saprophytic, dimorphic fungus that affects people and animals. The primary route of transmission is by inhaling conidia from the soil. It is thought that most infections are self-limiting, but pulmonary or disseminated disease may occur. Clinical signs in cats are often chronic and nonspecific, while dogs often display gastrointestinal signs. Definitive diagnosis is based on cytologic or histologic identification of H. capsulatum. The treatment of choice in cats and dogs is the azole antifungal agent itraconazole. The prognosis depends on the extent of disease and can range from guarded to excellent. The best method of prevention is to avoid exposure to contaminated areas. Horizontal or zoonotic transmission has not been documented, but common-source infection has been observed.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Craig Thompson, DACVP, for obtaining and providing the digital photomicrographs and Dr. Jacob Rohleder, DACVR, for interpreting the radiographic images used in this manuscript.
Kelly Gingerich, DVM
Lynn Guptill, DVM, PhD, DACVIM
Department of Veterinary Clinical Sciences
School of Veterinary Medicine
Purdue University
West Lafayette, IN 47907
REFERENCES
1. Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996;32(5):380-391.
2. Norton SA. Deep fungal skin diseases. In: James WD, ed. Military dermatology. Textbook of military medicine—Part 3, disease and the environment. Washington D.C.: Department of the Army, 1994;1-40.
3. DeMonbreun WA. The dog as a natural host for Histoplasma capsulatum. Am J Trop Med Hyg 1939;19:565-587.
4. Cano MV, Hajjeh RA. The epidemiology of histoplasmosis: a review. Semin Respir Infect 2001;16:109-118.
5. Emmons CW: Isolation of Histoplasma capsulatum from soil. Public Health Rep 1949;64(28):892-896.
6. Emmons C. Histoplasmosis in animals. Trans N Y Acad Sci (Ser II) 1949;2:248-250.
7. Ford RB. Canine histoplasmosis. Compend Contin Educ Pract Vet 1980;2:637-642.
8. Clinkenbeard KD, Cowell RL, Tyler RD. Disseminated histoplasmosis in dogs: 12 cases (1981-1986). J Am Vet Med Assoc 1988;193(11):1443-1447.
9. Mitchell M, Stark DR. Disseminated canine histoplasmosis: a clinical survey of 24 cases in Texas. Can Vet J 1980;21:95-100.
10. Greene CE. Histoplasmosis. In: Greene CE, ed. Infectious diseases of the dog and cat. 3rd ed. St. Louis, Mo: Saunders Elsevier, 2006;577-584.
11. Taboada J, Grooters AM. Systemic mycoses. In: Ettinger S, ed. Textbook of veterinary internal medicine. 6th ed. St. Louis, Mo: Elsevier Saunders, 2005;680-682.
12. Deepe GS Jr. Histoplasma capsulatum: darling of the river valleys. ASM News 1997;63:599-604.
13. Turner C, Smith CD, Furcolow ML. Frequency of isolation of Histoplasma capsulatum and Blastomyces dermatitidis from dogs in Kentucky. Am J Vet Res 1972;33(1):137-141.
14. Selby LA, Becker SV, Hayes HW Jr. Epidemiologic risk factors associated with canine systemic mycoses. Am J Epidemiol 1981;113(2):133-139.
15. Clinkenbeard KD, Cowell RL, Tyler RD. Disseminated histoplasmosis in cats: 12 cases (1981-1986). J Am Vet Med Assoc 1987;190(11):1445-1448.
16. Wolf AM, Greene RW. The radiographic appearance of pulmonary histoplasmosis in the cat. Vet Radiol 1987;28:34-37.
17. Schulman RL, McKiernan BC, Schaeffer DJ. Use of corticosteroids for treating dogs with airway obstruction secondary to hilar lymphadenopathy caused by chronic histoplasmosis: 16 cases (1979-1997). J Am Vet Med Assoc 1999;214(9):1345-1348.
18. Gabbert NH, Campbell TW, Beiermann RL. Pancytopenia associated with disseminated histoplasmosis in a cat. J Am Anim Hosp Assoc 1984;20:119-122.
19. Farrell RL, Cole CR. Experimental canine histoplasmosis with acute fatal and chronic recovered courses. Am J Pathol 1968;53(3):425-445.
20. Krohne SG. Canine systemic fungal infections. Vet Clin North Am Small Anim Pract 2000;30(5):1063-1090.
21. Olson GA, Wowk BJ. Oral lesions of histoplasmosis in a dog. Vet Med Small Anim Clin 1981;76(10):1449-1451.
22. Greene CE, Hartmann K, Calpin J. Antimicrobial drug formulary. In: Greene CE, ed. Infectious diseases of the dog and cat. 3rd ed. St. Louis, Mo: Saunders Elsevier, 2006;1200-1203,1272-1277.
23. Kowalewich N, Hawkins EC, Skowronek AJ, et al. Identification of Histoplasma capsulatum organisms in the pleural and peritoneal effusions of a dog. J Am Vet Med Assoc 1993;202(3):423-426.
24. Sanford SE, Straube U. Ontario. Disseminated histoplasmosis in a young dog. Can Vet J 1991;32:692.
25. Tyre E, Eisenhart D, Foley P, et al. Histoplasmosis in a dog from New Brunswick. Can Vet J 2007;48(7):734-736
26. Huss BT, Collier LL, Collins BK, et al. Polyarthropathy and chorioretinitis with retinal detachment in a dog with systemic histoplasmosis. J Am Anim Hosp Assoc 1994;30:217-224.
27. Shelton GD, Stockham SL, Carrig CB, et al. Disseminated histoplasmosis with bone lesions in a dog. J Am Anim Hosp Assoc 1982;18:143-146.
28. Mackie JT, Kaufman L, Ellis D. Confirmed histoplasmosis in an Australian dog. Aust Vet J 1997;75(5):362-363.
29. Nishifuji K, Ueda Y, Sano A, et al. Interdigital involvement in a case of primary cutaneous canine histoplasmosis in Japan. J Vet Med A Physiol Pathol Clin Med 2005;52(9):478-480.
30. Clinkenbeard KD, Wolf AM, Cowell RL, et al. Canine disseminated histoplasmosis. Compend Contin Educ Pract Vet 1989;11:1347-1360.
31. Kagawa Y, Aoki S, Iwatomi T, et al. Histoplasmosis in the skin and gingiva in a dog. J Vet Med Sci 1998;60(7):863-865.
32. Rosychuk RAW, White SD. Systemic infectious diseases and infestations that cause cutaneous lesions. Vet Med 1991;86(2):164-181.
33. Meadows RL, MacWilliams PS, Dzata G, et al. Diagnosis of histoplasmosis in a dog by cytologic examination of CSF. Vet Clin Pathol 1992;21(4):122-125.
34. Gwin RM, Makley TA Jr, Wyman M, et al. Multifocal ocular histoplasmosis in a dog and cat. J Am Vet Med Assoc 1980;176(7):638-642.
35. VanSteenhouse JL, DeNovo RC Jr. Atypical Histoplasma capsulatum infection in a dog. J Am Vet Med Assoc 1986;188(5):527-528.
36. Kerl ME. Update on canine and feline fungal diseases. Vet Clin North Am Small Anim Pract 2003;33(4):721-747.
37. Martin C, Stiles J. Ocular manifestations of systemic disease. Part 1: The dog; Part 2: The cat. In: Gelatt K, ed. Veterinary ophthalmology. Baltimore, Md: Lippincott Williams & Wilkins, 1999;1401-1473.
38. Hodges RD, Legendre AM, Adams LG, et al. Itraconazole for the treatment of histoplasmosis in cats. J Vet Intern Med 1994;8(6):409-413.
39. Pearce J, Giuliano EA, Galle LE, et al. Management of bilateral uveitis in a Toxoplasma gondii-seropositive cat with histopathologic evidence of fungal panuveitis. Vet Ophthalmol 2007;10(4):216-221.
40. Stark DR. Primary gastrointestinal histoplasmosis in a cat. J Am Anim Hosp Assoc 1982;18:154-156.
41. Johnson LR, Fry MM, Anez KL, et al. Histoplasmosis infection in two cats from California. J Am Anim Hosp Assoc 2004;40(2):165-169.
42. Burton G. The cat with non-healing wounds. In: Rand J, ed. Problem-based feline medicine. China: Elsevier Saunders, 2006;1081-1106.
43. Wolf AM. Histoplasma capsulatum osteomyelitis in the cat. J Vet Intern Med 1987;1(4):158-162.
44. Wolf AM. Successful treatment of disseminated histoplasmosis with osseous involvement in two cats. J Am Anim Hosp Assoc 1988;24:511-516.
45. Vinayak A, Kerwin SC, Pool RR. Treatment of thoracolumbar spinal cord compression associated with Histoplasma capsulatum infection in a cat. J Am Vet Med Assoc 2007;230(7):1018-1023.
46. Clinkenbeard KD, Tyler RD. Thrombocytopenia associated with disseminated histoplasmosis in dogs. Compend Contin Educ Pract Vet 1989;11:301-306.
47. Duncan JR, Prasse KW, Mahaffey EA. Veterinary laboratory medicine. 3rd ed. Ames: Iowa State University Press, 1994.
48. Brown MR, Rogers KS. Neutropenia in dogs and cats: a retrospective study of 261 cases. J Am Anim Hosp Assoc 2001;37(2):131-139.
49. Clinkenbeard KD, Cowell RL, Tyler RD. Identification of Histoplasma organisms in circulating eosinophils of a dog. J Am Vet Med Assoc 1988;192(2):217-218.
50. Noxon JO, Digilio K, Schmidt DA. Disseminated histoplasmosis in a cat: successful treatment with ketoconazole. J Am Vet Med Assoc 1982;181(8):817-820.
51. Brömel C, Sykes JE. Histoplasmosis in dogs and cats. Clin Tech Small Anim Pract 2005;20(4):227-232.
52. Gardner CE. Pulmonary histoplasmosis in a dog. Mod Vet Pract 1981;62(10):785-786.
53. Blass CE. Histoplasmosis in a cat. J Am Anim Hosp Assoc 1982;18:468-470.
54. Lenarduzzi RF, Jones L. Diagnosing pulmonary histoplasmosis despite nonspecific clinical signs. Vet Med 1986;81(5):412-418.
55. Chapman BL, Hendrick MJ, Washabau RJ. Granulomatous hepatitis in dogs: nine cases (1987-1990). J Am Vet Med Assoc 1993;203(5):680-684.
56. Burk RL, Jones BD. Disseminated histoplasmosis with osseous involvement in a dog. J Am Vet Med Assoc 1978;172(12):1416-1417.
57. Lau RE, Kim SN, Pirozok RP. Histoplasma capsulatum infection in a metatarsal of a dog. J Am Vet Med Assoc 1978;172(12):1414-1416.
58. Rochat MC, Crystal MA. Challenging cases in internal medicine: what's your diagnosis? Vet Med 1999:94(6):520-527.
59. Kabli S, Koschmann JR, Robertstad GW, et al. Endemic canine and feline histoplasmosis in El Paso, Texas. J Med Vet Mycol 1986;24(1):41-50.
60. Hawkins EC, DeNicola DB. Cytologic analysis of tracheal wash specimens and bronchoalveolar lavage fluid in the diagnosis of mycotic infections in dogs. J Am Vet Med Assoc 1990;197(1):79-83.
61. Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am 2003;17(1):1-19, vii.
62. Wheat LJ. Current diagnosis of histoplasmosis. Trends Microbiol 2003;11(10):488-494.
63. Wheat LJ, Garringer T, Brizendine E, et al. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn Microbiol Infect Dis 2002;43(1):29-37.
64. Ueda Y, Sano A, Tamura M, et al. Diagnosis of histoplasmosis by detection of the internal transcribed spacer region of fungal rRNA gene from a paraffin-embedded skin sample from a dog in Japan. Vet Microbiol 2003;94(3):219-224.
65. Murata Y, Sano A, Ueda Y, et al. Moldecular epidemiology of canine histoplasmosis in Japan. Med Mycol 2007;45(3):233-247.
66. Wheat J, Wheat H, Connolly P, et al. Cross-reactivity in Histoplasma capsulatum variety capsulatum antigen assays of urine samples from patients with endemic mycoses. Clin Infect Dis 1997;24(6):1169-1171.
67. Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev 2007;20(1):115-132.
68. Boothe DM, Herring I, Calvin J, et al. Itraconazole disposition after single oral and intravenous and multiple oral dosing in healthy cats. Am J Vet Res 1997;58(8):872-877.
69. Vandewoude K, Vogelaers D, Decruyenaere J, et al. Concentrations in plasma and safety of 7 days of intravenous itraconazole followed by 2 weeks of oral itraconazole solution in patients in intensive care units. Antimicrob Agents Chemother 1997;41(12):2714-2718.
70. McGinnis MR, Pasarell L, Sutton DA, et al. In vitro evaluation of voriconazole against some clinically important fungi. Antimicrob Agents Chemother 1997;41(8):1832-1834.
71. LeMonte AM, Washum KE, Smedema ML, et al. Amphotericin B combined with itraconazole or fluconazole for treatment of histoplasmosis. J Infect Dis 2000;182(2):545-550.
72. Hector RF. An overview of antifungal drugs and their use for treatment of deep and superficial mycoses in animals. Clin Tech Small Anim Pract 2005;20(4):240-249.
73. Nomeir AA, Kumari P, Hilbert MJ, et al. Pharmacokinetics of SCH 56592, a new azole broad-spectrum antifungal agent, in mice, rats, rabbits, dogs, and cynomolgus monkeys. Antimicrob Agents Chemother 2000;44(3):727-731.
74. Roffey SJ, Cole S, Comby P, et al. The disposition of voriconazole in mouse, rat, rabbit, guinea pig, dog, and human. Drug Metab Dispos 2003;31(6):731-741.
75. Malik R, Craig AJ, Wigney DI, et al. Combination chemotherapy of canine and feline cryptococcosis using subcutaneously administered amphotericin B. Aust Vet J 1996;73(4):124-128.
76. Bekersky I, Boswell GW, Hiles R, et al. Safety and toxicokinetics of intravenous liposomal amphotericin B (AmBisome) in beagle dogs. Pharm Res 1999;16(11):1694-1701.
77. Dupont B. Overview of the lipid formulations of amphotericin B. J Antimicrob Chemother 2002;49(suppl):31-36.
78. Kleinberg M. What is the current and future status of conventional amphotericin B? Int J Antimicrob Agents 2006;27(suppl 1):12-16.
79. Legendre AM, Rohrbach BW, Toal RL, et al. Treatment of blastomycosis with itraconazole in 112 dogs. J Vet Intern Med 1996;10(6):365-371.
80. Berthelin CF, Legendre AM, Bailey CS. Cryptococcosis of the nervous system in dogs: Part 2. Diagnosis, treatment, monitoring, and prognosis. Prog Vet Neurol 1994;5:136-145.
81. Legendre AM. Antimycotic drug therapy. In: Bonagura JD, ed. Kirk's current veterinary therapy XII small animal practice. Philadelphia, Pa: WB Saunders Co, 1995;329-331.
82. Davies SF, Colbert RL. Concurrent human and canine histoplasmosis from cutting decayed wood. Ann Intern Med 1990;113(3):252-253.
83. Brunker JD, Hoover JP. B-cell lymphoma in a dog with ehrlichiosis (Ehrlichia canis) and systemic histoplasmosis (Histoplasma capsulatum). Can Vet J 2007;48(3):292-295.
84. Krawiec DR, McKiernan BC, Twardock R, et al. Use of an amphotericin B lipid complex for treatment of blastomycosis in dogs. J Am Vet Med Assoc 1996;209(12):2073-2075.
85. Deepe GS Jr. Histoplasma capsulatum. In: Mandell GLB, Bennett JE, Dolin R, eds. Principles and practice of infectious diseases. 5th ed. New York: Churchill Livingstone, 2000;2718-2733.
86. Gustafson TL, Kaufman L, Weeks R, et al. Outbreak of acute pulmonary histoplasmosis in members of a wagon train. Am J Med 1981;71(5):759-765.
87. Muniz MM, Pizzini CV, Peralta JM, et al. Genetic diversity of Histoplasma capsulatum strains isolated from soil, animals, and clinical specimens in Rio de Janeiro State, Brazil, by a PCR-based random amplified polymorphic DNA assay. J Clin Microbiol 2001;39(12):4487-4494.
88. Sano A, Miyaji M. Canine histoplasmosis in Japan [Japanese]. Nippon Ishinkin Gakkai Zasshi 2003;44(4):239-243.
89. Woods JP, Heinecke EL, Luecke JW, et al. Pathogenesis of Histoplasma capsulatum. Semin Respir Infect 2001;16(2):91-101.
90. Eissenberg LG, Goldman WE, Schlesinger PH. Histoplasma capsulatum modulates the acidification of phagolysosomes. J Exp Med 1993;177(6):1605-1611.
91. Newman SL. Cell-mediated immunity to Histoplasma capsulatum. Semin Respir Infect 2001;16(2):102-108.
92. Howard DH, Rafie R, Tiwari A, et al. Hydroxamate siderophores of Histoplasma capsulatum. Infect Immun 2000;68(4):2338-2343.
93. Batanghari JW, Goldman WE. Calcium dependence and binding in cultures of Histoplasma capsulatum. Infect Immun 1997;65(12):5257-5261.