Canine stomatitis: an unusual presentation
An unusual presentation results in an unusual diagnosis.
Stomatitis generally is thought of as a feline disease. Although it is seen much more frequently in cats, dogs can present with stomatitis as well.

Brett Beckman
Primary generalized stomatitis (affecting buccal mucosa and many times tongue margins and palatal mucosa adjacent to teeth) where no specific cause is detected is likely associated with a profound host immune response to oral microbes associated with plaque. Generalized stomatitis can be secondary to a variety of other diseases.
A thorough evaluation of the patient is indicated when stomatitis is present. The dental case this month had an unusual presentation that resulted in an unusual diagnosis.

Photo 1: Profound generalized oral mucosal stomatitis and mucopurulent oral discharge in a 5-year-old Maltese.
A 5-year-old Maltese presented with profound generalized oral mucosal ery-thema, stomatitis and mucopurulent oral and nasal discharge with severe halitosis (Photo 1). The entire palatal mucosa was equally affected (Photo 2), but the margins of the tongue were not. Dried crusts of mucous almost obliterated the nasal openings bilaterally. The nasal discharge occurred some weeks following the onset of the oral signs. A previous biopsy from the referring veterinarian revealed inflammation consistent with stomatitis.
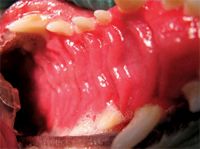
Photo 2: A severely erythematous palatal mucosa is uncharacteristic of stomatitis in the dog. (Photos courtesy of Dr. Brett Beckman)
This patient did not show any reluctance to oral manipulation, which was quite uncharacteristic for this kind of presentation. Most patients with this pathology are in pain, so sedation often is required for a complete evaluation. Palpation of the tissue did, however, repeatedly induce avoidance behavior consistent with oral pain. Upon removal of the dried mucous crusts surrounding the nasal openings, nasal mucosal hyperemia was excessive, approximating the scale of that found in the oral cavity (Photo 3). Based on the initial biopsy at the referring practice suggesting primary stomatitis, what do you tell the owners at this point?

Photo 3:The nasal mucosa displayed significant erythema and discharge.
Building a treatment plan
Stomatitis in dogs is a painful condition generally poorly responsive to conservative management. Frequent professional dental prophylaxis is the initial approach to therapy followed by strict adherence to a home-care regimen. Brushing a minimum of once daily is the basis of conservative therapy. Chlorhexidine daily gel, plaque-retardant sealants, water additives and enzymatic chews may serve as adjunctive therapy. In many cases, strict adherence to home care alleviates signs only for three to six months before professional prophylaxis is required. Immunosuppressive agents may offer short-term benefits; however, long-term therapy generally is unrewarding and has obvious detrimental long-term effects.
In some cases, extraction of teeth adjacent to affected areas is indicated. In generalized cases, this may require full-mouth extractions.
Now that you have thoroughly discussed primary stomatitis, we are ready to make our therapeutic recommendations. Or are we? What clinical signs normally present with cases of stomatitis just don't fit this case?
Profound nasal mucositis and generalized palatal involvement are not commonly seen. Typically the palatal mucosa is affected immediately adjacent to the tooth/palate interface. In this case, the entire mucosa was affected. Nasal discharge might be a secondary factor or a separate entity, but the degree of hyperemia strikes an unusual chord in this case.
Immune-mediated disease, renal insufficiency, liver disease, viral, bacterial and fungal organisms, eosinophilic granuloma complex, foreign-body reactions, chemical and thermal insult should be included in our list of differential diagnoses.
In an attempt to determine a specific etiology, a biopsy was taken of the nasal mucosa, including a portion of the alar fold, the lip margin and oral mucosa, and submitted for histopathology. Consultation with dermatology resulted in a trial of immunosuppressive doses of prednisone and a broad-spectrum antibiotic. Interestingly enough, both samples in this second biopsy were consistent with erythema multiforme, which is a rare ulcerative dermatosis associated with host-specific T lymphocyte cell-mediated hypersensitivity. (See suggested reading, p. 10S.)
Infections, drug therapy and food have been implicated. However, a large percentage of cases are idiopathic. Vesicles and ulcerations are common oral mucosal changes. Ulcers commonly are covered by a gray-white film consistent with those seen in this case. The oral mucosa is a common site for lesion predilection with this condition.
Spontaneous regression has been reported in a matter of weeks to months. Definitive resolution occurs if the cause can be determined and resolved. The use of immunosuppressive drugs is not without controversy and is usually reserved for more severe cases where a cause cannot be determined. Anecdotal evidence suggests that cyclosporine may be of benefit in canine idiopathic erythema multiforme.
Response to therapy
Two weeks later, the dermatology service reported much improvement in the degree of stomatitis. The doctor tapered the dosage of prednisone and discontinued the antibiotic. Two weeks after a recheck with the dentistry service, the doctors noted an appreciably positive response in the palatal mucosa (Photo 4, p. 9S). But the caudal buccal mucosa showed epithelial sloughing and severe stomatitis (Photo 5, p. 9S). No other potential causes co-existed with onset, and the initial biopsy didn't show changes characteristic of erythema multiforme.

Photo 4:The patient showed a dramatic response in the palatal mucosa following immunosuppressive doses of prednisone.
Taking into consideration historical and clinical aspects of this case, it might be logical to speculate that the stomatitis was the primary disease, subsequently resulting in erythema multiforme. It is, however, impossible to make this conclusion definitively. The etiology of individual cases of this disease is difficult to determine.

Photo 5: Severe stomatitis and gray-white plaques (adjacent to the fourth premolar) were seen two weeks following prednisone tapering.
Another diagnostic consideration is chronic ulcerative paradental stomatitis (CUPS) which resembles stomatitis and has similar histopathology. With CUPS, mucosal irritation occurs in regions where the tissue contacts the tooth. Unfortunately, original classification was not possible in that we did not observe this patient until after the erythema multiforme was present.
At this point in the work-up, the owners opted to maintain this patient on immunosuppressive doses of prednisone. If stomatitis is the inciting factor, extractions would likely result in complete resolution. Unfortunately, we may not have the opportunity to find out. Updates regarding any change in owner sentiment resulting in a different long-term plan will be discussed in future issues.
Our next article will address a more classic case of CUPS.
Dr. Beckman is acting president of the American Veterinary Dental Society and owns and operates a companion-animal and referral dentistry and oral surgery practice in Punta Gorda, Fla. He sees referrals at Affiliated Veterinary Specialists in Orlando and at Georgia Veterinary Specialists in Atlanta, lectures internationally and operates the Veterinary Dental Education Center in Punta Gorda.
For a complete list of articles by Dr. Beckman, visit dvm360.com/beckman