Choosing the best tests to diagnose feline hyperthyroidism
In this article, I describe the most common clinical signs and physical examination findings in hyperthyroid cats. I also review the available diagnostic methods, including their advantages and disadvantages.
In this article, I describe the most common clinical signs and physical examination findings in hyperthyroid cats. I also review the available diagnostic methods, including their advantages and disadvantages.
CLINICAL SIGNS AND PHYSICAL EXAMINATION FINDINGS
In a study of 202 cats with hyperthyroidism at the Animal Medical Center in New York City, the clinical sign most commonly reported by owners was weight loss.1 Polyphagia, vomiting, polyuria and polydipsia, increased activity, a decreased appetite or anorexia, diarrhea, weakness, dyspnea, panting, and a large fecal volume were also common owner complaints. Hyperthyroidism has been reported in cats ranging in age from 4 to 22 years, but 95% of cases occur in cats older than 10 years.1
On physical examination, a palpable enlargement of one or both thyroid glands is likely. Enlargement of the glands may precede a rise in T4 concentrations, emphasizing the importance of a thorough physical examination.2 A cat with advanced hyperthyroidism often has a low body condition score with muscle atrophy. A host of other physical examination findings may also be present, such as an unkempt coat, a heart murmur, tachycardia, a gallop rhythm, restlessness, or aggression. Some cats with pronounced cardiac effects may be in congestive heart failure.
The clinical signs associated with hyperthyroidism have been declining in severity over the years.1 In one review, the authors compared the electrocardiographic and radiographic changes seen in two populations of cats confirmed to have hyperthyroidism—one from 1979 to 1982 and one from 1992 to 1993.3 Sinus tachycardia, which is the most commonly recognized cardiac manifestation of feline thyrotoxicosis, was not as prevalent in the 1993 group as it was in the 1982 group. That was also true of an increased R-wave amplitude on lead II electrocardiography. Both groups had similar low incidences of atrial and ventricular dysrhythmias, but the 1993 group had a significantly higher occurrence of right bundle branch block. Thoracic radiographs were deemed necessary in a larger proportion of the 1982 group than in the 1993 group. Although no significant differences in cardiac size were noted on radiographs between the two groups, a larger number of cats in the 1982 group had evidence of congestive heart failure. These findings suggest that feline hyperthyroidism is being diagnosed earlier today and that newly diagnosed cats have less severe cardiovascular clinical signs than a decade ago.
DIAGNOSTIC TESTS
Hyperthyroidism can be definitively diagnosed by measuring increased serum thyroid hormone concentrations or by performing scintigraphy. Both tests have advantages and disadvantages.
Serum tests
The advantages of using serum tests to diagnose hyperthyroidism include their low cost, ease (no need for anesthesia), and availability (standard laboratory tests). The main disadvantage of serum testing is that the results may not be easy to interpret if a cat has other illnesses or if you are trying to diagnose hyperthyroidism in its early stages. Other tests (e.g. T3 suppression, thyroid-stimulating hormone and thyrotropin-releasing hormone stimulation testing, scintigraphy) are available if the suspicion is high for hyperthyroidism in cats with appropriate clinical signs but normal thyroid hormone concentrations.
Total T4 and free T4
In the initial diagnostic approach to a cat with hyperthyroidism, the best test is still total T4 measurement. This test is simple and inexpensive and provides the correct diagnosis in most cases. However, we now are often faced with diagnosing or confirming hyperthyroidism in cats that are asymptomatic, that have only mild clinical signs, or that have concurrent illness that may skew laboratory assessment of thyroid function. These cases can be challenging, but recent research indicates that measuring free T4 by equilibrium dialysis is the next logical diagnostic step. This approach is likely to eliminate the need for additional expensive or problematic tests such as thyrotropin-releasing hormone stimulation and T3 suppression.
Two studies have assessed the value of free T4 measurement by equilibrium dialysis in diagnosing feline hyperthyroidism and have evaluated the effects of nonthyroidal illness on thyroid function.4,5 As is the case in dogs, euthyroid cats with nonthyroidal illness may have a decrease in total T4 concentrations that probably results from protein-binding abnormalities. In a study of 98 cats with nonthyroidal illness and 50 normal control cats, thyroid function was assessed by measuring total T4 and free T4 concentrations.4 Serum total T4 concentrations were measured by radioimmunoassay, and free T4 concentrations were measured by equilibrium dialysis. Serum total T4 concentrations were significantly lower in sick cats (1.33 ± 0.63 µg/dl [17.18 ± 8.14 nmol/L]; reference range = 0.8 to 4 µg/dl) than in healthy cats (2 ± 0.59 µg/dl [26 ± 7.62 nmol/L]). Serum total T4 concentrations were inversely correlated with mortality. No significant difference was noted between the serum free T4 concentrations in sick cats (2.15 ± 1.05 µg/dl [27.7 ± 13.53 pmol/L]; reference range = 0.78 to 3.9 µg/dl [10 to 50 pmol/L]) and in healthy cats (1.93 ± 0.65 µg/dl [24.79 ± 8.33 pmol/L]). Twelve percent of sick euthyroid cats had increased serum free T4 concentrations. This study showed that, as is the case in dogs and people, euthyroidism is maintained in sick cats, despite low serum total T4 concentrations. Also the serum total T4 concentration is a valuable prognostic indicator because it appears to be an excellent predictor of mortality. Lastly, and perhaps more importantly with respect to diagnosing hyperthyroidism, some euthyroid older cats have elevated free T4 concentrations measured by equilibrium dialysis. Thus, initially measuring free T4 by equilibrium dialysis as a screening test for hyperthyroidism in older cats can lead to false positive results.
One of the challenges in diagnosing hyperthyroidism is the effect that nonthyroidal illness has on thyroid function tests in cats with concurrent hyperthyroidism. In a large study, researchers measured total T4, free T4 (by equilibrium dialysis), and total T3 concentrations in 917 cats with hyperthyroidism, 221 cats with nonthyroidal illness, and 172 clinically normal cats.5 They found that measuring free T4 by equilibrium dialysis was significantly more sensitive than measuring total T4 as a diagnostic test for hyperthyroidism. However, of the 221 cats with nonthyroidal illness, 12 cats (5.4%) had a high free T4 concentration measured by equilibrium dialysis (a false positive result). Therefore, the calculated specificity of measuring free T4 by equilibrium dialysis as a diagnostic test for hyperthyroidism was significantly lower than the specificity of measuring total T4. This study suggests that measuring free T4 by equilibrium dialysis is only indicated in those cats with clinical signs and a total T4 concentration in the upper 50% of the normal resting range. In these animals, the free T4 concentration will be elevated. In our practice, we see this most often in cats with nonthyroidal illnesses such as inflammatory bowel disease, gastrointestinal lymphoma, diabetes, and renal disease as well as in cats receiving glucocorticoids. The biggest challenge is deciding how to treat such cats. You must decide what role both diseases are playing with respect to the clinical signs and address each disease separately.
ALP, ALT, Calcium, and PTH
We know that many cats with hyperthyroidism have elevated alkaline phosphatase (ALP) or alanine transaminase (ALT) activities. Results of serum bile acids testing and histopathologic examination of liver biopsy samples in these cats are abnormal, but no clinical signs are present, and the abnormalities resolve after treating the hyperthyroidism in most cats. Hypercalcemia can also be seen in hyperthyroid cats. The calcium abnormalities appear to self-correct after successful treatment, and no other cause for the hypercalcemia has been found. Several recent studies have examined the effects of hyperthyroidism on bone and calcium metabolism in hyperthyroid cats.
Enzymes that arise from the liver, bone, the intestines, and other tissues constitute serum ALP. The source of elevated total serum ALP activity in hyperthyroid cats has been suggested to be from the liver and bone isoenzymes. In one study, ALP isoenzymes were measured by serum electrophoresis in five normal cats and in 34 hyperthyroid cats.6 Electrophoresis was used to identify and quantify ALP isoenzymes in homogenates of the kidneys, the intestines, bone, and the liver. In both groups, the highest concentration of ALP was found in the kidneys, followed by the intestines, the liver, and then bone. The liver isoenzyme of ALP was the only type identified in the serum of normal cats. Serum total ALP activity was elevated in 53% of hyperthyroid cats. Thirty of the 34 hyperthyroid cats had two main electrophoresis bands corresponding to liver and bone isoenzymes of ALP. A significant correlation was noted between the total T4 concentration and total serum ALP activity and the total T4 concentration and liver isoenzyme activity, but not between the T4 concentration and bone isoenzyme activity in hyperthyroid cats. The proportion of bone and liver isoenzymes of ALP in sera of hyperthyroid cats varied considerably, with the liver isoenzyme making up 17% to 100% of the total serum ALP and the bone isoenzyme constituting 0% to 74% of ALP. The researchers concluded that abnormalities in bone and liver isoenzymes account for the elevations in serum ALP found in hyperthyroid cats. This study points out that practitioners should evaluate thyroid function in older cats with increased serum ALP activities. Although bone disease has not been reported to occur in cats with hyperthyroidism, it is likely that the high bone ALP activity is related to increased bone turnover. This theory was reinforced in two studies evaluating bone turnover and calcium metabolism in hyperthyroid cats.7,8
In one study, serum markers for increased bone metabolism and turnover were evaluated in 36 cats that had elevated serum T4 concentrations and elevated serum ALP activities.7 Serum total calcium, ionized calcium, and phosphorus concentrations were measured. ALP isoenzymes were separated by agarose gel electrophoresis, and the concentration of osteocalcin, a marker of increased bone turnover, was measured by radioimmunoassay. The test results in the hyperthyroid cats were compared with those in healthy cats. All 36 hyperthyroid cats had markedly increased ALP bone isoenzyme activity. Forty-four percent of the cats had increased osteocalcin concentrations. No correlation was found among the magnitude of increase in ALP bone isoenzyme activity, osteocalcin, and serum T4 concentrations. Thirty-five percent of the cats had increased serum phosphorus concentrations. All the cats had total calcium concentrations within the reference range, while 50% of the cats had decreased serum ionized calcium concentrations. This study provided evidence that bone turnover is increased in hyperthyroid cats but that it is not clinically important because the increased bone turnover does not result in clinical signs (e.g. pain, arthritis, fracture) as a result of osteoporosis. The finding of low serum ionized calcium concentrations in half of the hyperthyroid cats is interesting, and this topic relates to the study described next.
Parathyroid hormone (PTH) and ionized calcium concentrations in 30 untreated hyperthyroid cats and 38 age-matched normal (control) cats were evaluated.8 The hyperthyroid group had significantly lower blood ionized calcium and plasma creatinine concentrations and significantly higher plasma phosphorus and PTH concentrations. Seventy-seven percent of the hyperthyroid cats had hyperparathyroidism, with PTH concentrations up to 19 times the upper limit of the reference range. The authors stated that the etiology, significance, and reversibility of hyperparathyroidism in hyperthyroid cats have yet to be determined but could play a role in these cats' bone strengths and renal functions. Hyperthyroid cats may have decreased creatinine concentrations from either increased glomerular filtration rates or decreased muscle mass, though that was not evaluated in this study. The effects of thyrotoxicosis on renal function are discussed in the next article.
Fructosamine
The effect of hyperthyroidism on clinical and laboratory findings hasn't been fully elucidated. Because many hyperthyroid cats are geriatric and are likely to have concurrent disease, it remains important to thoroughly investigate these interrelationships. Two recent studies evaluated the effects of hyperthyroidism on laboratory assessment of glycemic control (by measuring serum fructosamine concentrations) in cats with concurrent diabetes mellitus.
In cats, serum fructosamine concentrations reflect the mean blood glucose concentration of the preceding one or two weeks. However, fructosamine concentrations are affected by the concentration and metabolism of serum proteins. Hyperthyroidism can profoundly increase protein metabolism and, therefore, possibly affect serum fructosamine concentrations. In one study, hyperthyroidism was diagnosed in 22 cats, ranging in age from 8 to 20 years, based on clinical signs, detection of a palpable thyroid gland, and a serum total T4 concentration greater than 45 nmol/L.9 Blood glucose, total protein, and albumin concentrations were within reference ranges. The serum fructosamine concentrations of the 22 hyperthyroid cats were compared with those of 42 healthy control cats, 10 newly diagnosed diabetic cats, and nine cats with hypoproteinemia. Serum total T4 concentrations ranged from 46 to 475 nmol/L (median µ 86 nmol/L). Hyperthyroid cats had serum fructosamine concentrations between 154 and 267 µmol/L (median µ 198 µmol/L), significantly less than those in healthy cats. Serum fructosamine concentrations in cats with hypoproteinemia ranged from 124 to 254 µmol/L (median µ 174 µmol/L; reference range = 175 to 400 µmol/L) and were significantly less than those in healthy cats. Serum fructosamine concentrations did not differ between hypoproteinemic and hyperthyroid cats. In hypoproteinemic cats, concentrations of serum total protein and albumin were significantly lower than those in hyperthyroid cats, while blood glucose concentrations did not differ between the two groups of cats. Serum fructosamine concentrations in diabetic cats were significantly increased compared with those in healthy cats, hypoproteinemic cats, and hyperthyroid cats. After two weeks of carbimazole treatment (discussed in the next article) in six of the hyperthyroid cats, serum fructosamine concentrations were not significantly different from the initial concentrations. After six weeks of carbimazole treatment, serum fructosamine concentrations were significantly higher than the initial concentrations. Serum total T4 concentrations were significantly decreased both two and six weeks after initiating treatment. The authors concluded that serum fructosamine concentrations are lower in cats with hyperthyroidism independent of blood glucose concentrations. In the clinical setting, serum fructosamine concentrations should not be used to initially diagnose or assess the adequacy of diabetic control in cats with concurrent hyperthyroidism in which the hyperthyroidism has not been controlled for at least six weeks.
In another study, fructosamine concentrations were evaluated in 30 nondiabetic hyperthyroid cats before and 30 days after radioiodine treatment (discussed in the next article) and compared with normal control cats.10 Fructosamine concentrations were significantly lower in the hyperthyroid cats both before and after treatment with radioiodine. However, treatment was associated with a statistically significant increase in fructosamine concentrations. This study, like the study evaluating cats with diabetes mellitus, shows that fructosamine concentrations in hyperthyroid cats will be lower than those in nonhyperthyroid cats (normal or diabetic) and that this effect is probably from the effects of hyperthyroidism on increasing protein turnover.
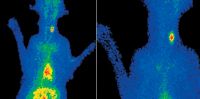
Figure 1. Scintigrams of a 10-year-old domestic shorthaired cat with hyperthyroidism. Unilateral uptake of pertechnetate with pooling of the isotope is evident in the heart along with the trapping of the isotope in the gastric mucosa. The area of interest is highlighted on the right panel.
Thyroid scanning
Scintigraphy has been used since 1985 to diagnose hyperthyroidism. The isotopes most commonly used for imaging are pertechnetate (99mTcO4) and iodine-123 (123I). Hyperplastic thyroid glands have increased uptake of these radioactive isotopes, which is detectable by nuclear imaging. This procedure detects whether one or both glands are enlarged (70% of cats have bilateral enlargement) and detects other sites of thyroid gland activity (e.g. ectopic benign thyroid tissue, metastatic thyroid carcinoma) (Figures 1-3). Disadvantages include the lack of nuclear imaging centers available to practitioners, the need for anesthesia, and the cost. Furthermore, recent data indicate that treating a cat with methimazole before nuclear imaging may increase the radioactive material absorbed by the thyroid gland, creating false interpretations of increased thyroid activity.11
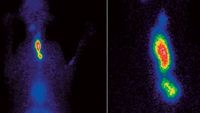
Figure 2. Scintigrams of an 11-year-old domestic shorthaired cat with hyperthyroidism. Bilaterally asymmetric uptake of pertechnetate with mild pooling of the isotope is evident in the heart along with the trapping of the isotope in the gastric mucosa. The area of interest is highlighted on the right panel.
SUMMARY
Hyperthyroidism is a common endocrine disorder in senior cats. Clinical signs in cats with hyperthyroidism appear to be declining in severity, likely because of earlier recognition of the disorder and the use of routine total T4 screening tests in senior cats. Nonthyroidal illness can interfere with the diagnosis of hyperthyroidism, especially in cats with mild increases in total T4. Measuring free T4 by equilibrium dialysis and performing nuclear scintigraphy can enhance our ability to accurately diagnose this disorder in cats, including cats with concurrent nonthyroidal illness.

Figure 3. Scintigrams of an 11-year-old domestic shorthaired cat with hyperthyroidism. Mild, bilaterally asymmetric uptake of pertechnetate with mild pooling of the isotope is evident in the heart along with the trapping of the isotope in the gastric mucosa. The area of interest is highlighted on the right panel.
David S. Bruyette, DVM, DACVIM
VCA West Los Angeles Animal Hospital
1818 S. Sepulveda Blvd.
West Los Angeles, CA 90025
REFERENCES
1. Broussard, J.D. et al.: Changes in clinical and laboratory findings in cats with hyperthyroidism from 1983 to 1993. JAVMA 206 (3):302-305; 1995.
2. Norsworthy, G.D. et al.: Palpable thyroid and parathyroid nodules in asymptomatic cats. J. Feline Med. Surg. 4 (3):145-151; 2002.
3. Fox, P.R. et al.: Electrocardiographic and radiographic changes in cats with hyperthyroidism: Comparison of populations evaluated during 1992-1993 vs. 1979-1982. JAAHA 35 (1):27-31; 1999.
4. Mooney, C.T. et al.: Effect of illness not associated with the thyroid gland on serum total and free thyroxine concentrations in cats. JAVMA 208 (12):2004-2008; 1996.
5. Peterson, M.E. et al.: Measurement of serum concentrations of free thyroxine, total thyroxine, and total triiodothyronine in cats with hyperthyroidism and cats with nonthyroidal disease. JAVMA 218 (4):529-536; 2001.
6. Foster, D.J.; Thoday, K.L.: Tissue sources of serum alkaline phosphatase in 34 hyperthyroid cats: A qualitative and quantitative study. Res. Vet. Sci. 68 (1):89-94; 2000.
7. Archer, F.J.; Taylor, S.M.: Alkaline phosphatase bone isoenzyme and osteocalcin in the serum of hyperthyroid cats. Can. Vet. J. 12:735-739; 1996.
8. Barber, P.J.; Elliott, J.: Study of calcium homeostasis in feline hyperthyroidism. J. Small Anim. Pract. 37 (12):575-582; 1996.
9. Reusch, C.E.; Tomsa, K.: Serum fructosamine concentration in cats with overt hyperthyroidism. JAVMA 215 (9):1297-1300; 1999.
10. Graham, P.A. et al.: Serum fructosamine concentrations in hyperthyroid cats. Res. Vet. Sci. 67 (2):171-175; 1999.
11. Nieckarz, J.A.; Daniel, G.B.: The effect of methimazole on thyroid uptake of pertechnetate and radioiodine in normal cats. Vet. Radiol. Ultrasound 42 (5):448-457; 2001.