ClinQuiz: Interpreting low-dose dexamethasone suppression test results 2016 update
Test your knowledge of what these LDDS test results mean.
2016 update:
Editor's note: This ClinQuiz originally appeared in the February, 2009, issue of Veterinary Medicine. Dr. Bruyette has provided an update for 2016 below.
ACVIM consensus statement
In 2012, the American College of Veterinary Internal Medicine issued a consensus statement addressing the diagnosis of spontaneous canine hyperadrenocorticism, which provides a thorough review of the diagnostic approach to patients with hyperadrenocorticism and addresses many common clinical concerns.

David Bruyette, DVM, DACVIM
This statement can be found here.
Diagnosing hyperadrenocorticism
Low dose dexamethasone suppression (LDDS) test
The LDDS test demonstrates decreased pituitary sensitivity to negative feedback from glucocorticoids.
Indications. Most consider LDDS the screening test of choice for hyperadrenocorticism unless the patient history suggests iatrogenic hyperadrenocorticism, in which case ACTH stimulation is preferred.
Sensitivity/specificity. In veterinary medicine, the reported sensitivity and specificity of the LDDS test range from 85% to 100% and from 44% to 73%, respectively.
Test procedure. The LDDS test is typically performed in dogs that have fasted for eight hours (check whether your laboratory requires fasted samples). To perform this test, obtain a baseline (0 hour) blood sample, administer dexamethasone sodium phosphate (0.015 mg/kg) or aqueous dexamethasone (0.01 mg/kg) intravenously, and obtain two additional blood samples four and eight hours later. Contact your laboratory before testing to determine its specific LDDS test protocol. The serum cortisol concentrations are measured in the three blood samples.
Test interpretation. When interpreting LDDS test results, first evaluate the eight-hour post-dexamethasone administration cortisol concentration. If it is above the reference range, the dog probably has hyperadrenocorticism (false positive results may occur in dogs with nonadrenal illness). If it is within the reference range, either the dog does not have hyperadrenocorticism or there is a 5% to 10% chance that the dog has PDH. (The dog may have early pituitary disease and the pituitary gland is still responding to a pharmacologic dose of dexamethasone by decreasing ACTH production, thereby reducing serum cortisol concentrations.) In those cases, an ACTH stimulation test is warranted.
If the eight-hour post-dexamethasone administration cortisol concentration is above the reference range, then evaluate the baseline and four-hour postdexamethasone administration cortisol concentrations to see whether cortisol suppression occurred during the eight hours. If at least 50% cortisol concentration suppression is present at the four- or eight-hour time points, the definitive diagnosis is PDH and additional adrenal function tests are not needed.
Principles behind dexamethasone suppression testing in differentiating pituitary-dependent hyperadrenocorticism (PDH) from functional adrenal tumors:
Patients with a functional adrenal tumor:
A) Dexamethasone at any dose does not suppress cortisol secretion.
Patients with PDH:
A) Dexamethasone does not appropriately suppress ACTH secretion (therefore does not suppress cortisol) when a low dose (0.01 mg/kg) is administered.
B) In 75% of dogs with PDH, ACTH and cortisol concentrations decrease when a high dose (0.1 mg/kg) is administered.
C) In 25% of dogs with PDH, suppression of ACTH and cortisol does not occur even after administration of higher dosages; in these patients, a large pituitary tumor or tumor developing from the pars intermedia is more likely.
Studies
The largest study evaluating both suppression tests-LDDS and high dose dexamethasone suppression (HDDS)-included dogs with PDH (n = 181) and adrenal tumors (n = 35).1 With LDDS, criteria for identifying dogs with PDH included:
A) Four-hour post LDDS cortisol concentrations below laboratory cutoff or < 50% of basal cortisol concentration.
B) Eight-hour post LDDS cortisol concentrations < 50% of the basal cortisol concentration and greater than the laboratory cutoff.
With HDDS, criteria for cortisol suppression were a four- and/or eight-hour cortisol concentration below the laboratory cutoff or < 50% of the basal cortisol concentration.
Approximately 75% of dogs with PDH met at least one criterion for suppression on either LDDS or HDDS. Of those with PDH, 88% demonstrated suppression with the LDDS and 12% demonstrated suppression with HDDS.
Dexamethasone resistance (i.e. no criteria were met) occurred in all dogs with functional adrenal tumors and the remainder (25%) of the dogs with PDH. In another study of 41 dogs with functional adrenal tumors, 28 LDDS and 30 HDDS tests were performed, with no suppression seen on any test.2
In dogs demonstrating lack of suppression with LDDS, use of endogenous ACTH rather than HDDS is recommended to differentiate PDH from adrenal-dependent hyperadrenocorticism (ADH), since suppression in response to dexamethasone supports a diagnosis of PDH, while a dog with dexamethasone resistance can have either functional adrenal tumors or PDH.
Continue through the case information and quiz on page 2 to test your knowledge of LDDS testing and see page 3 for references and suggested reading.
The four case examples in this quiz help illustrate some of the common pitfalls in LDDS test result interpretation and questions practitioners have after receiving the test results. For the purposes of this quiz, the reference range for the eight-hour post-dexamethasone administration cortisol concentration is ≤ 2 µg/dl; however, this cutoff value varies by laboratory.
Case 1:
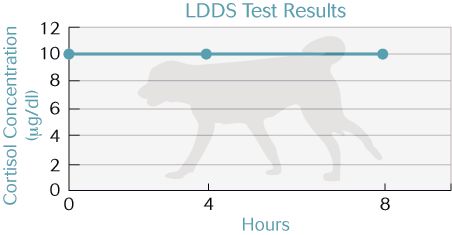
A. The dog has hyperadrenocorticism.
B. The dog has hyperadrenocorticism secondary to an adrenal tumor (ADH).
D. PDH and ADH cannot be differentiated based on these results.
Case 2:
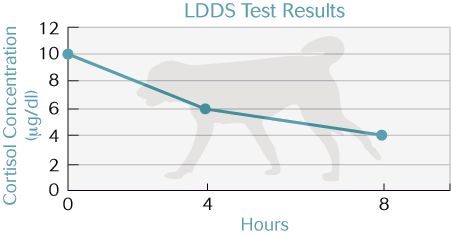
A. The dog has hyperadrenocorticism.
B. The dog has hyperadrenocorticism secondary to an adrenal tumor (ADH).
D. PDH and ADH cannot be differentiated based on these results.
Case 3:
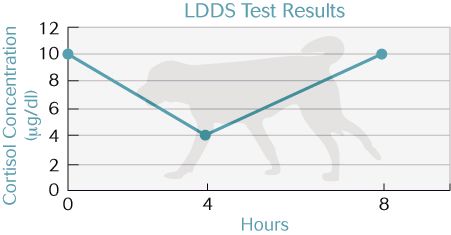
A. The dog has hyperadrenocorticism.
B. The dog has hyperadrenocorticism secondary to an adrenal tumor (ADH).
D. PDH and ADH cannot be differentiated based on these results.
Case 4:
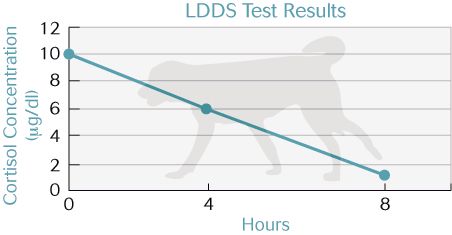
A. The dog has hyperadrenocorticism.
B. The dog has hyperadrenocorticism secondary to an adrenal tumor (ADH).
D. PDH and ADH cannot be differentiated based on these results.
References
1. Feldman EC, Feldman MS, Nelson RW. Use of low and high-dose dexamethasone tests for distinguishing pituitary dependent from adrenal tumor hyperadrenocorticism in dogs. JAVMA 1996; 9:772-775.
2. Meijer JC, Lubberink AAME, Rijnberk A, Croughs JM. Adrenocortical function tests in dogs with hyperfunctioning adrenocortical tumors. J Endocrinol 1979; 80:315-319.
Suggested reading
1. Behrend EN, Kooistra HS, Nelson R, et al. Diagnosis of spontaneous canine hyperadrenocorticism: 2012 ACVIM consensus statement (small animal). J Vet Intern Med 2013; 27:1292-1304.
2. Feldman EC. Comparison of ACTH response and dexamethasone suppression as screening tests in canine hyperadrenocorticism. JAVMA 1981; 182:506-510.
3. Meijer JC, de Bruijne JJ, Rijnberk A, Croughs RJM. Biochemical characterization of pituitary-dependent hyperadrenocorticism in the dog. J Endocrinol 1978; 77:111-118.
4. Mack RE, Feldman EC. Comparison of two low-dose dexamethasone suppression protocols as screening and discrimination tests in dogs with hyperadrenocorticism. JAVMA 1990; 197:1603-1606.
5. May ER, Frank LA, Hnilica KA, Lane IF. Effects of a mock ultrasonographic procedure on cortisol concentrations during low-dose dexamethasone suppression testing in clinically normal adult dogs. Am J Vet Res 2004; 65:267-270.
6. Rijnberk A, van Wees A, Mol JA. Assessment of two tests for the diagnosis of canine hyperadrenocorticism. Vet Rec 1988; 122:178-180.
7. van Liew CH, Greco DS, Salman MD. Comparison of results of adrenocorticotropic hormone stimulation and low-dose dexamethasone suppression test with necropsy findings in dogs: 81 cases (1985-1995). JAVMA 1997; 211:322-325.
8. Foster SF, Church DB, Watson ADJ. Effect of phenobarbitone on the low-dose dexamethasone suppression test and the urinary corticoid:creatinine ratio in dogs. Aust Vet J 2000; 78:19-23.
9. Reusch CE, Feldman EC. Canine hyperadrenocorticism due to adrenocortical neoplasia. Pretreatment evaluation of 41 dogs. J Vet Int Med 1995; 5:3-10.
This quiz was provided by David S. Bruyette, DVM, DACVIM, VCA West Los Angeles Animal Hospital, 1818 S. Sepulveda Blvd, West Los Angeles, CA 90025.