Common mistakes in your veterinary dermatology workups
In a busy veterinary clinic, it's easy to make your best educated guess and move on when presented with what seem to be simple dermatologic diagnoses. But not so fast-many conditions can have similar presentations.
We have all been mystified by some clinical presentations of various dermatologic diseases. There isn't one of us who hasn't opened a dermatology book and looked to see if a picture of what we're seeing matches. The problem is, in dermatology a patient can have several manifestations of the same disease, and the same disease can look different among various breeds.
After almost 25 years as a boarded veterinary dermatologist I'd like to think I've learned a thing or two that I can pass on to help you sort out what you're seeing. The following are a few tips about differential diagnoses for diagnosing similar-looking diseases and some pearls of wisdom that I have found helpful.
Don't forget demodicosis of the feet
Let's start with feet. One of the most forgotten and undiagnosed foot problems is Demodex species infection of the feet, or demodectic pododermatitis. Demodicosis is one of the most common reasons for recurrent yeast or bacterial pododermatitis, yet it's frequently missed. Instead, if yeast or bacteria are found on skin smears, a skin scraping is often neglected (Figures 1A and 1B). Don't stop at just performing cytology of the feet and nail beds-be sure to do deep skin scrapings of the affected areas.

Figure 1A. Demodex species mites affecting the feet of a dog with secondary bacterial and yeast pododermatitis. (All photos courtesy of Dr. Alice M. Jeromin.)

Figure 1B. Demodicosis in an English bulldog being treated as a bacterial pododermatitis. Don't forget to scrape the feet!Sometimes the initial presentation is with just one foot affected. I have had patients that have always favored one foot since very young and were never checked for demodicosis-it was assumed they were allergic since they licked the foot. Years later, this can grow into generalized demodicosis if corticosteroids continue to be prescribed because it is thought that the patient is allergic. Be sure to rule out demodicosis before starting any corticosteroids as they will reduce the inflammation but incite the demodicosis even more. Remember, not all dogs that lick their feet are allergic.
Is it juvenile cellulitis or demodicosis?

Figure 2. The chin of a young English bulldog with Demodex species mites and deep pyoderma. This can be mistaken for juvenile cellulitis (puppy strangles).As mentioned above about missing the diagnosis of demodicosis of the feet, in young dogs with suspected juvenile cellulitis, be sure and scrape for Demodex species mites first before starting the traditional corticosteroid and antibiotic therapy used for suspected juvenile cellulitis. Both diseases may result in lymphadenopathy, deep pyoderma and swelling of the periocular area and muzzle (Figure 2). A mistake would be to not check for Demodex species mites and start treatment because of the above clinical signs in a young dog. Scrapings take only a few seconds and can make the difference between diagnosing the correct disease or, in the case of demodicosis, perpetuating a potentially fatal disease.
And don't forget demodicosis of the ears
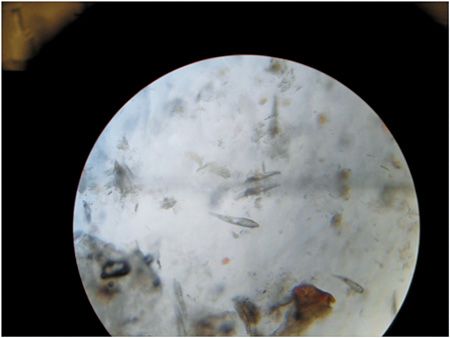
Figure 3. Adult Demodex species mites seen on an ear smear in oil under the microscope.When diagnosing otitis, remember when performing ear smears for yeast or bacteria to also perform ear smears in oil in dogs and cats. Otitis caused by Otodectes species and especially Demodex species may be missed if smears are not checked in oil (Figure 3). As with demodicosis of the feet, if you find yeast on smears or cytology, then make sure to dig deeper by doing smears in oil to look for demodectic otitis.
Quick tip for the ears
All ear drops should be administered at room temperature. One study showed that in any species-people included-cold ear drops should not be instilled in the ear since vertigo, nausea or vomiting may result. So if certain ear preparations need to be refrigerated, bring them to room temperature before administration.
Ear smears in oil need to be performed on all patients with otitis, especially those with generalized demodicosis that you think may have resolved their skin lesions. Sometimes demodectic otitis tends to linger despite resolution in other parts of the body, and practitioners may forget to monitor ear smears.
Rule out dermatophytosis before treating for pemphigus foliaceus
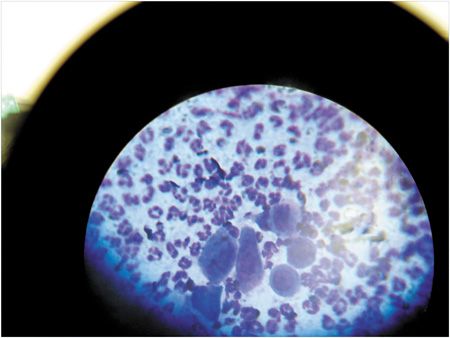
Figure 4. Acantholytic cells on cytologic examination of a pustule from a patient with pemphigus foliaceus (modified Wright's stain; oil immersion).Clinically and histologically, pemphigus foliaceus and dermatophytosis have many similarities. Acantholytic cells are one of the histologic characteristics of pemphigus foliaceus in a skin biopsy (Figure 4), but dermatophytosis can also produce acantholytic cells. Since these two diseases are treated totally differently-one with immunosuppressives, the other with antifungals-it is important to rule out dermatophytosis before starting corticosteroids or other immunosuppressives for pemphigus foliaceus.

Figure 5. A poodle with lesions consistent with pemphigus foliaceus.
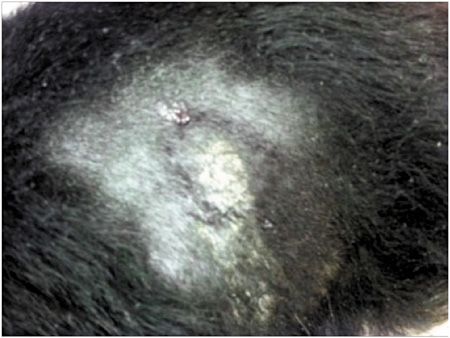
Figure 6. A dermatophytosis lesion on the trunk of a dog infected with Microsporum canis.Special stains used on the skin biopsy samples can help rule out dermatophytes, but a fungal culture is important to include in your workup when you are diagnosing pemphigus foliaceus (Figures 5 and 6). It would be deleterious to use immunosuppressives in a patient with dermatophytosis as its immunity is already compromised. Also consider the public health ramifications of missing a diagnosis of dermatophytosis. If you are not an expert at reading your own fungal cultures, submit them to the laboratory. This is what we do at my office as I want to be confident we have ruled out dermatophytes and are not dealing with a fungal contaminant.
Treat pyodermas like pyodermas
When you have a first-time bacterial pyoderma in a young dog (Figure 7), treat it as a pyoderma-don't assume that the dog is allergic and add corticosteroids. Some dogs with pyoderma are pruritic, while others are not. Allergy should be considered once the pyoderma has been properly treated and if pruritus remains. Properly treated means antibiotics were administered until total clearing of the lesions, plus an additional week, as well as weekly antibacterial bathing.
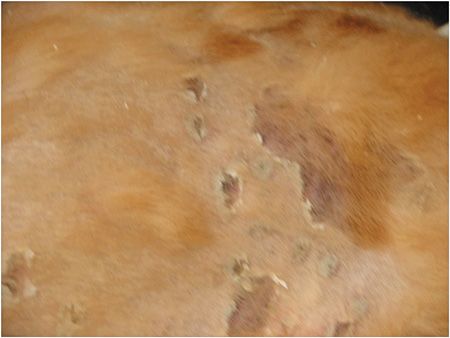
Figure 7. Bacterial pyoderma lesions on the trunk of a dog.Some dogs are so corticosteroid-sensitive that even a tiny dose will negate the effect of the antibiotic. If you need to prescribe something for the pruritus, either use an antihistamine, topical water-based corticosteroid conditioner (nothing stronger than a 1% preparation-and some owners overuse even this) or more frequent bathing. Also, when using cefpodoxime or amoxicillin-clavulanic acid for pyoderma, both medications tend to work best at the high end of the dosage range (10 mg/kg once a day for cefpodoxime; 13.75 mg/kg t.i.d. for amoxicillin-clavulanic acid). When using cephalexin, remember that it can take 21 days for optimal doses to get into the circulation feeding the skin and to treat the patient until the lesions are gone, plus an additional week past clearing. This should be explained to owners.
Don't mistake epitheliotropic lymphoma for pyoderma
Epitheliotropic lymphoma can present with three different manifestations: erythema and scaling, nodular or tumor stage. The first two manifestations are often mistaken for a bacterial pyoderma. These patients will frequently have a history of different antibiotics being prescribed without success (and sometimes a corticosteroid dose that will alleviate any associated inflammation). In an older dog, particularly a golden retriever or boxer, if antibiotics (whether dosed empirically or based on culture and sensitivity results) are not improving your patient's lesions, perform skin biopsies to rule out skin lymphoma.

Figure 8. A golden retriever with epitheliotropic lymphoma. Note the raspberry-colored erythema.When cytologic examination of the lesions is performed in-house, it usually provides a clue, showing numerous lymphocytes that are not normally seen in cytology of a bacterial pyoderma. A skin biopsy is then indicated to confirm the diagnosis. Also in the erythemic presentation of epitheliotropic lymphoma, the generalized erythema is more of a raspberry color than the traditional pink or red that sometimes accompanies a pyoderma (Figure 8).
Final thoughts
I sincerely hope the above suggestions and tips will help in your daily practice. Basically, it is a good idea to perform skin scrapings, combings, ear smears and ear smears in oil in every dermatology patient and to perform a cytologic examination of any skin masses that may be present. All of these procedures take very little time to perform, yet they can yield important diagnostic and therapeutic information.
Suggested reading
1. Hillier A, Lloyd DH, Weese JS, et al. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society of Companion Animal Infectious Diseases). Vet Dermatol 2014;25:163-175.
2. Gross TL, Ihrke PJ, Walder EJ, et al. Skin diseases of the dog and cat: clinical and histopathologic diagnosis. 2nd ed. Ames, Iowa: Blackwell Publishing, 2005;15-16, 414.
3. Tater KC, Patterson AP. Canine and feline demodicosis. Vet Med 2008;103(8):444-461.
Dr. Jeromin is a pharmacist and veterinary dermatologist in private practice in Cleveland, Ohio. She is a 1989 graduate of the Ohio State University College of Veterinary Medicine and an adjunct professor at Case Western Reserve University's College of Medicine.