Dentistry case study: an unusual gingival lesion
This is the first article in a series of case presentations designed to address a variety of oral conditions and discuss the pathophysiology involved.
This is the first article in a series of case presentations designed to address a variety of oral conditions and discuss the pathophysiology involved. I will ask you to stop and think about the options to explore diagnostically and therapeutically, as we explore them step-by-step.
Presentation: A 7-year-old Staffordshire Bull Terrier presented with a fistula adjacent to the maxillary left canine (Figure 1). The fistula was present at the mucogingival line, which demarcates the attached gingiva and the unattached gingiva (alveolar mucosa).

Figure 1: A fistula is present at the mucogingival line between the left maxillary canine and first premolar.
What are the origins of the fistula? Knowing no other history, several possibilities should come to mind. Direct trauma is plausible if duration is unknown. A penetrating foreign body might be another possibility. Periodontal disease is a consideration if the fistula is in the attached gingiva.
This particular defect is bisected by the mucogingival junction, so it is difficult to tell where its origin resides. On the other hand, fistulas on the alveolar mucosa are likely a result of endodontic disease. In the case of this patient, the location of the fistula might implicate either the canine or the first premolar. Take note of the appearance of the canine cusp. There is blunting of the normal round appearance of the tip of this tooth, suggesting wear and/or fracture.
So, what is the most likely tentative diagnosis? What would you do to confirm the diagnosis?
Diagnostic challenge
In this case, the tooth in question was worn by abrasion, which is defined as wear secondary to contact with anything other than another tooth. Tooth-on-tooth contact is termed attrition.
The cause of the wear was a mystery to the owners. Wear to the point of dentin exposure can be problematic in several ways. Exposed dentin can be sensitive to touch, temperature changes and air movement.
Dentin is not as impervious as it appears. Although very solid in appearance, dentin is comprised of a network of tubules containing live cells that extend from the odontoblast that lies adjacent to the pulp all the way to the dentin-enamel interface.
Exposure to oral bacteria may allow destruction of the cell process and the odontoblast. Bacteria may gain access to the pulp, causing inflammation of the pulp (pulpitis) and eventually results in pulp death and necrosis. To confirm this suspicion, dental radiography is the next step. What are we looking for as signs of pulp necrosis?
Radiographically this tooth has an increase in bone lucency surrounding the root tip or apex (Figure 2). This decrease in bone density represents bone destruction secondary to bacteria residing within the pulp cavity, serving as a persistent source of infection.
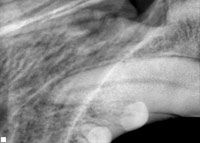
Figure 2: The radiographic appearance of the left maxillary 4th premolar demonstrates a lucency in the bone adjacent to the apex.
Dentin is continually produced throughout the life of the tooth. Consequently the diameter of the pulp cavity decreases as the patient ages. If a tooth dies, the dentin production ceases. This can result in a discrepancy in pulp-cavity diameter whereby the dead tooth may have a pulp cavity larger than its equal in the opposite arcade (Figure 3).
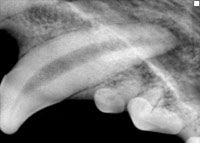
Figure 3: The right maxillary canine tooth has a pulp cavity that is noticeably smaller in diameter indicating that the left canine is non-vital.
This is not always the case however. Chronic pulpitis may result in overstimulation of dentin production, eventually resulting in a tooth with a smaller pulp chamber. Although uncommon, it should be taken into consideration.
What are the treatment options for a worn tooth with necrotic pulp?
Elimination of the necrotic pulp will eliminate further inflammation and destruction of periapical bone. Root-canal therapy allows for elimination of the pulp, cleaning the pulp canal, filling the canal and sealing it to allow the patient to retain the tooth while the periapical tissue heals.
The other option for this patient is extraction of the canine tooth. Pet guardians should be given an option for referral for root-canal therapy or extraction in all cases of teeth that are non-viable. "Wait and see" is not an option for these patients because veterinary patients are very adept at hiding oral pain. Practitioners with extraction skills involving use of mucoperiosteal flaps may be comfortable performing this procedure.
This case manifests endodontic disease not seen by most clinicians. Most patients with pulp death do not present with fistulas. Many show no soft-tissue signs grossly. Furthermore, fractured teeth with pulp exposure and teeth that are intrinsically stained are dead or dying teeth and should be treated in a similar manner.
A tooth fracture that does not reach the pulp chamber often involves dentin exposure and may be dead or dying. Radiographs might not always be diagnostic in cases where recent fracture has not provided evidence of chronicity described in this case.
When dentin exposure is confirmed but the radiographic evidence of tooth death is not yet evident, radiographs should be repeated in four to six months to determine if pathology is present. In the meantime, treating the dentin with dentinal bonding and/or composite restoration will seal the open dentinal tubules and eliminate any further exposure to oral bacteria.
In our case, the endodontic disease must be either treated with extraction or root-canal therapy. The next article in this series will describe the treatment approach to this case.
Dr. Beckman is acting president of the American Veterinary Dental Society and owns and operates a companion-animal and referral dentistry and oral surgery practice in Punta Gorda, Fla. He sees referrals at Affiliated Veterinary Specialists in Orlando and at Georgia Veterinary Specialists in Atlanta, lectures internationally and operates the Veterinary Dental Education Center in Punta Gorda.