Endodontic disease: Remove the source of infection
Concussive force from blunt trauma can result in pulpal inflammation and death of the pulp tissue.
Endodontic disease is a pathologic process dealing with the pulp cavity. To get a deeper understanding, one first must have knowledge of the anatomy of the tooth, especially the pulp.
The tooth is divided into three areas. The first area is the crown, the visible portion of the tooth coronal to the gingiva. The second area is the root, the portion of the tooth below the gingiva and encased in the alveolar bone. The third area is the neck, which is the junction of the root and the crown.
Typically, the neck is inside the gingival sulcus. The bulk of the tooth is made of dentin, which becomes thicker as the tooth ages. In the area of the crown, the dentin is covered by enamel. In the area of the root, the dentin is covered by cementum.
The cementum and the enamel meet at the neck of the tooth. Within the dentin is the pulp cavity. Above the gum, it is referred to as the pulp chamber, whereas below it is referred to as the root canal. The pulp is comprised of nerves, blood vessels, collagen fibers, elastic fibers and cells, including odontoblasts. The odontoblasts line the periphery of the pulp and produce dentin. The tip of the root is termed the apex and contains the apical delta. The apical delta is an area of many small canals extending from the root canal through the dentinal walls to the periapical space. It is through this delta that the blood and nerve supply enter the pulp cavity. It is important to remember that the tooth is a vital structure, so it is sensitive and responsive to a variety of stimuli.
•Endodontic pathology
Inflammation of the pulp tissue is termed pulpitis, which can be either reversible or irreversible. If the pulpitis is reversible, the pulp returns to a healthy state when the cause of the inflammation is removed. An example of this would be a carious lesion. Restoration of the caries removes the irritation and allows the pulp to return to normal.
With an irreversible pulpitis, the inflammation of the pulp tissue within the unyielding dentinal walls results in a cessation of the circulation to the pulp tissue. As a result, the necessary nutrient supply and gas exchange is halted, resulting in pulpal necrosis.
There are multiple causes of pulpitis, including trauma, bacterial penetration from resorptive or carious lesions, extension of periodontal disease into the pulp cavity via lateral canals or through the apical delta and anachoresis (blood-borne bacteria). Trauma resulting in crown fracture and pulp exposure creates an avenue for bacterial invasion and subsequent pulpal death. Concussive force from blunt trauma can result in pulpal inflammation and death of the pulp tissue without the bacterial influx seen with pulp exposure. Bacteria then can invade the necrotic pulp tissue through the apical delta via anachoresis.
When irreversible pulpitis occurs, periapical inflammation and apical periodontitis follow. The classic presentation of endodontic pathology is the periapical lucency seen on radiographs with chronic disease (Figure 1).

Figure 1: Note the presence of periapical lucency, a presentation of endodontic pathology.
•Diagnosis of endodontic disease
Signs of endodontic disease include discolored teeth, fractured teeth with pulpal exposure, pain with chewing or chewing on one side of the mouth, reluctance to hold objects in the mouth, excessive salivation, sensitive teeth, sinus tract formation (apical to the mucogingival junction).
- Discolored teeth: This is a result of concussive trauma without pulp exposure. Blood and its breakdown products enter the dentinal tubules resulting in a pink to purple discoloration of the crown. If the pulpitis is irreversible, the color typically changes to a purple-gray or brown (Figure 2).

Figure 2: Concussive trauma can cause a pink to purple discoloration of the crown.
- Fractured teeth with pulpal exposure: If it is fresh, bleeding from the pulp will be present. The fracture site is probed with an explorer. If the tip of the explorer can enter the pulp chamber, endodontic involvement is certain (Figure 3). If the pulp is not exposed, the tooth still can be non-vital due to bacterial invasion through the dentinal tubules.

Figure 3: If the fracture is fresh, bleeding from the pulp will be present.
- Oral pain: During the acute phase, or later on with the development of a periapical abscess, the patient might exhibit oral pain. In some cases, the patient can show an excessive buildup of calculus on the effected side compared to the contralateral side.
- Sinus tract formation: After the periapical infection develops, a draining tract can develop apical to the mucogingival junction (Figure 4). The maxillary carnassial teeth, third premolars and first molars can develop the classic draining tract on the ventral aspect of the associated orbit.

Figure 4: Look for a draining tract apical to the mucogingival junction.
It is very important to realize that in many cases, the patient might not display any obvious clinical signs. Careful evaluation of the oral cavity is an important part of the patient's physical examination. It is not uncommon for the diagnosis of endodontic disease to be made during the time of the routine health examination. A lack of obvious pain does not rule out endodontic disease. Another misconception is that if the tooth is solid in the alveolar bone, it is permissible to leave the tooth in place without any treatment. The fallacy with this decision is that tooth mobility is a function of the periodontal structures and has nothing to do with the state of the pulp. With endodontic disease, the periodontal structures are not affected significantly unless the periapical pathology extends coronally up the periodontal ligament space and can result in tooth mobility. This event is seen rarely.
•Treatment of endodontic disease
Endodontic disease can be compared to a bony sequestrum or a foreign body infection. In both of these cases, the body cannot clear up the infection as long as the sequestrum or foreign body is present. With removal of the sequestrum or foreign body, the body then can resolve the infection. With endodontic disease, the necrotic pulp is the foreign body or sequestrum. Without any blood supply to this source of infection, the root-canal contents, the bacteria continue to percolate out through the apical delta perpetuating the infection. Treatment of endodontic disease is based on removing the source of the infection, the necrotic pulp chamber contents.
Root-canal therapy removes the infected pulp tissue and refills the pulp cavity with a material to prevent re-establishment of bacteria in the root canal. Initially, the root canal is shaped by filing and disinfected by irrigation with a bactericidal solution. The filing removes the contaminated surface of the dentinal walls and also shapes the canal for filling. The bactericidal solution, sodium hypochlorite, chlorhexidine or EDTA aids in dissolution of the necrotic contents and provides chemical disinfection.
After the canal has been cleaned and dried, a dentinal sealant is placed in the canal to seal the dentinal tubules. The canal is obturated (filled) with a material that prevents bacterial growth and conforms to the root-canal shape. The most commonly used product is gutta percha. Although the entire pulp cavity should be filled with the obturation material, the most critical part of the root-canal filling is the apical one-third. Communication of the pulp cavity to the periapical space is through the apical delta and through accessory canals, when present. In most cases, these openings are limited to the apical one-third of the root canal cavity.
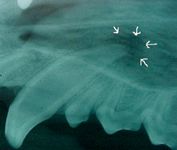
Figure 5: If evidence of periapical infection is present, then antibiotics are indicated.
After filling the root canal, the fracture site (and access hole openings if created) are sealed with restorative compounds. If evidence of active periapical infection is present, post-operative antibiotics are indicated. A follow-up radiograph should be obtained six to 12 months later to determine the success of the root-canal procedure. (See Figures 5, 6.)

Figure 6: Follow-up six to 12 months later with a radiograph to determine the success of the root-canal procedure.
The other option available for treatment of endodontic disease is extraction. (See related story) With extraction, the source of the infection is removed, but so is the tooth. However, as pets are becoming more a part of the family, owners are requesting the best option for their animal family members. Root-canal therapy should always be offered as an option.
•Summary
A complete oral examination should be a part of every visit to the veterinarian. In addition to the examination, a thorough history should be obtained, including oral issues. If a non-vital tooth is discovered, the two options should be discussed with the owner. Root-canal therapy always should be offered as an alternative to extraction. If the owners decline root-canal therapy, then extraction is performed. These are the only two options. Leaving the tooth in the mouth and ignoring the chronic infection is not an option.
Dr. Matson is a diplomate of the American Veterinary Dental College and a fellow of the Academy of Veterinary Dentistry. Dr. Matson operates a referral dentistry practice, Eastside Veterinary Dentistry. The referral practice is part of Hollywood Hill Animal Hospital in Woodinville, Wash., www.hollywoodhillanimalhospital.com. Matson graduated from Washington State University School of Veterinary Medicine in 1985.He can be reached via e-mail at: VettDrAl@aol.com.