Feline hyperaldosteronism: Recognition and diagnosis
Dr. Joseph Bisignano explains when you should add this disorder to your differential diagnosis list.
Primary hyperaldosteronism, also referred to as Conn's syndrome or aldosteronism, is an adrenal disorder characterized by excessive and independent secretion of aldosterone. Conn first described primary hyperaldosteronism in people in 1955 and discussed three hallmarks—hypertension, hypokalemia, and increased serum aldosterone concentrations.1 Primary hyperaldosteronism was originally thought to be a rare condition, but the prevalence in people was found to be 6% in all patients with arterial hypertension and about 11% in patients with therapy-resistant hypertension.2,3

Joseph Bisignano, DVM
The first case of primary hyperaldosteronism in a cat was described in 1983.4 The disease is not often diagnosed in veterinary practice despite the thought that it is likely one of the most common adrenocortical disorders in cats.5 Many cases of arterial hypertension, hypokalemia, or both are attributable to chronic kidney disease (CKD) as the primary disorder, but primary hyperaldosteronism itself has been shown to be a mediator and associated with the progression of CKD.6
This article reviews the physiology and actions of aldosterone and the pathophysiology of primary hyperaldosteronism, and it describes the typical presentation and clinicopathologic abnormalities. Primary hyperaldosteronism should be included as a differential diagnosis in cats presenting with hypokalemia, hypertension, or both and should no longer be regarded as a rare condition.
ALDOSTERONE PHYSIOLOGY
Aldosterone is a corticosteroid hormone with strong mineralocorticoid activity produced by the cells within the zona glomerulosa of the adrenal cortex. The production of aldosterone is driven and regulated through two main mechanisms: 1) the renin-angiotensin-aldosterone system and 2) direct regulation via potassium ions. The renin-angiotensin-aldosterone system becomes activated in response to a decrease in circulating blood volume and renal blood flow. This leads to a decrease in the delivery of sodium and chloride to the cells comprising the macula densa of the distal tubules and results in renin secretion. Renin cleaves angiotensinogen (produced in the liver) into angiotensin I, which in turn is hydrolyzed into angiotensin II in the lungs by angiotensin-converting enzyme (ACE). Angiotensin II stimulates the secretion of aldosterone from the adrenal gland.

David S. Bruyette, DVM, DACVIM
Potassium ions also regulate aldosterone secretion independent of the renin-angiotensin-aldosterone system by directly depolarizing the membranes of the zona glomerulosa cells in cases of hyperkalemia.7 Adrenocorticotropic hormone (ACTH) also acts as a third stimulant of aldosterone production, and studies have shown significant differences between plasma aldosterone concentrations before and after synthetic ACTH administration.8,9
Circulating aldosterone targets tissues of the kidney, colon, and salivary gland and passes through the plasma membranes of these epithelial cells, binding to cytoplasmic mineralocorticoid receptors. In response to circulating aldosterone, the epithelial cells of the distal convoluted tubules and collecting ducts of the kidney reabsorb sodium, thereby increasing water retention, and excrete potassium. Plasma and extracellular fluid volume are increased along with total peripheral resistance because of vasoconstriction from angiotensin II, thus causing an increase in blood pressure. Potassium is excreted into the urine, decreasing plasma potassium concentrations.
The increase in extracellular fluid volume results in an increased blood flow to the kidney, thereby decreasing renin secretion.5,10 Hyperkalemia resolves through kaliuresis, and repolarization of the zona glomerulosa cells occurs.7 These two mechanisms make up the negative feedback loop for aldosterone secretion.
PATHOPHYSIOLOGY OF HYPERALDOSTERONISM
Excessive aldosterone production can be the result of primary or secondary causes.5,10-13 Primary hyperaldosteronism results from a neoplastic adrenal mass—either an adenoma or an adenocarcinoma that could be unilateral or bilateral—or from hyperplasia of the zona glomerulosa of the adrenal cortex, often termed idiopathic or nontumorous primary hyperaldosteronism.5,11 Congestive heart failure, renal failure, and hepatic failure can each be responsible for secondary hyperaldosteronism because of activation of the renin-angiotensin-aldosterone system. The consequences of excessive aldosterone production are related to increased sodium and water retention, causing systemic arterial hypertension and increased renal potassium excretion, resulting in hypokalemia.5,10,14,15
Histopathologic findings in reported cases of cats with primary hyperaldosteronism include unilateral adrenocortical adenocarcinomas, unilateral and bilateral adenomas (Figure 1), and bilateral nodular hyperplasia of the adrenal glands.5,6,11,12,14,16,17 Since histopathologic examination of adrenal tissue is required to determine the cause of primary hyperaldosteronism, and cats with hyperplasia of the zona glomerulosa are typically treated medically, bilateral nodular hyperplasia likely occurs more frequently than is represented by current data. The etiology of this idiopathic form of hyperaldosteronism in cats is unknown at this time, but a circulating stimulatory factor is thought to be responsible for hyperfunction of the zona glomerulosa.6 This factor has not been identified, but one theory suggests it is a pituitary peptide that may be a fragment of pro-opiomelanocortin.6

1. A unilateral adrenal adenoma from a cat. (The shiny layer is the peritoneum, and the cat's head is to the right.)
With respect to cases of primary hyperaldosteronism, nontumorous or idiopathic bilateral nodular hyperplasia of the zona glomerulosa may lead to incomplete suppression of renin, while unilateral or bilateral neoplasia of the zona glomerulosa typically results in complete renin suppression.4-6,11,12,14,16,17 In disease with incomplete renin suppression, hyperaldosteronism is an important mediator of progressive renal disease in cats because of the presence of two mediators of vascular change and fibroproliferative destruction—aldosterone and angiotensin II.6
CKD has been linked to glomerular and tubulointerstitial injury as well as excessive accumulation of the extracellular matrix of the kidney.6 Extracellular matrix accumulation can be mediated by several growth factors including angiotensin II.6 Its actions may be involved in the upregulation of hyperplasia or hypertrophy of mesangial, glomerular endothelial, tubular epithelial, and renal interstitial fibroblasts.6 Angiotensin II is also a peripheral vasoconstrictor and a regulator of glomerular filtration and is considered a proinflammatory cytokine responsible for the onset of and progressive damage associated with CKD.6
Aldosterone can also contribute to the progression of renal damage by promoting vascular thrombosis and fibrosis.6 Thus both aldosterone and angiotensin II are instrumental in sustaining hypertension and further fibroproliferative destruction of the kidney.6 It is important to be aware of the role these factors play in the progression of renal disease, as systemic hypertension, hypokalemia, or both in geriatric cats are often clinical signs attributed to CKD as the causal disorder, as opposed to the direct effect of primary hyperaldosteronism. This association tends to delay or often preclude further diagnostic tests or screening for this disease in cats.
Many cats with hyperaldosteronism can also have evidence of cardiovascular disease indicated by the presence of a heart murmur, cardiomegaly on thoracic radiographic examination, or ventricular hypertrophy on echocardiographic examination.11,14,16-18 These cardiac changes are consistent with organ damage caused by hypertension secondary to increased intravascular volume.15
CLINICAL SIGNS AND PHYSICAL EXAMINATION AND CLINICOPATHOLOGIC FINDINGS
Feline hyperaldosteronism does not appear to have a sex or breed predilection, but affected cats are typically geriatric,4-6,10-13,16,17 with a single case report describing a 5-year-old cat.14
Clinical signs
Clinical signs are typically associated with potassium depletion and systemic arterial hypertension. Owners may report signs of episodic or acute muscle weakness including the inability to jump on and off surroundings, plantigrade stance of the hindlimbs, inability to raise the head (cervical ventroflexion), and lateral recumbency or collapse. Presenting complaints may also include concerns of sudden blindness, mydriasis, and hyphema.
Physical examination findings
The main physical examination abnormalities reported in cases of confirmed or suspected primary hyperaldosteronism include elevated arterial blood pressure; ocular signs consistent with hypertension such as tortuous retinal vessels and hemorrhage, retinal edema, and retinal detachment; and hypokalemic polymyopathy.4-6,10-12,14,16,18,19 Keep in mind that not all cats with hyperaldosteronism will present with classic signs associated with hypokalemia or hypertension and, in fact, could present with just one of these abnormalities or have a completely normal initial physical examination. Other reported findings that are less specific in nature include polyuria, polydipsia, enuresis, weight loss, palpable abdominal masses, polyphagia, and a heart murmur with or without an irregular cardiac rhythm.4-6,10-12,14,16,18,19
Clinicopathologic findings
Typical serum chemistry profile abnormalities in cats with hyperaldosteronism include moderate to severe hypokalemia and normal to mildly increased sodium concentrations. The water reabsorption that occurs secondary to sodium retention will dilute plasma sodium concentrations and is likely the reason that this electrolyte is rarely elevated.10-12,14,16,17 Serum creatine kinase concentrations are also usually markedly elevated in cats with hypokalemic polymyopathy.12 In one study of 13 cats with primary hyperaldosteronism, potassium concentration at presentation was a mean of 2.5 mEq/L (reference range = 4 to 5.5 mEq/L), sodium concentration ranged from 148 to 168 mEq/L (reference range = 140 to 160 mEq/L), severe elevations in creatine kinase were present with a mean of 6,837 IU/L (reference range = < 120 IU/L) and 12 of 13 were hypertensive (≥ 170 mm Hg).12
The effects of aldosterone also cause a markedly increased fractional excretion of potassium in the urine. Evidence of renal disease can also occur in cats with hyperaldosteronism including isosthenuria and elevated serum creatinine and blood urea nitrogen concentrations.6,10,12 Cats that are initially presented with normal renal function, or mild azotemia, may experience progression of renal disease since hyperaldosteronism may lead to glomerular sclerosis, tubular atrophy, hyaline arteriolar sclerosis, and interstitial fibrosis.6
INDICATIONS FOR DIAGNOSTIC INVESTIGATION
Any cat presenting with clinical findings of systemic arterial hypertension, hypokalemia, or mild azotemia should be considered for further evaluation of potential primary hyperaldosteronism. A thorough history and physical examination, complete blood count, serum chemistry profile, total T4 measurement, urinalysis, and indirect blood pressure measurement performed according to the American College of Veterinary Internal Medicine consensus statement20 will help rule out most other causes of hypokalemia and hypertension (Tables 1 & 2).
Table 1
If, based on the initial clinical examination and laboratory findings, primary hyperaldosteronism is considered a differential diagnosis, screening for abnormal regulation of aldosterone should be performed. If regulation is considered abnormal, the investigation should ideally continue to include diagnostic imaging to help determine potential treatment courses for the individual patient.
Table 2
SCREENING TESTS
Aldosterone:renin ratio
The gold standard for screening for feline primary hyperaldosteronism is the aldosterone:renin ratio.5,6,21 This test will allow determination and differentiation of primary vs. secondary hyperaldosteronism. The plasma renin activity (PRA) is taken into account, as an elevated plasma aldosterone concentration (PAC) with low PRA is indicative of aldosterone secretion independent of stimulation from the renin-angiotensin-aldosterone system.6 These patterns are consistent with primary hyperaldosteronism and the autonomous secretion of aldosterone by the adrenal glands.6,10 In cases of either unilateral or bilateral adrenal tumors, the PAC is typically markedly elevated, and the PRA is usually completely suppressed.5,6,10
This test has some disadvantages, mainly attributable to the sensitivity of the renin assay. The accuracy of the aldosterone:renin ratio depends on preservation of renin activity during sample collection and storage.5 A large volume of blood (4 ml) and instant freezing of separated plasma are necessary, and reference intervals for PRA differ markedly among laboratories, making comparison difficult.5 Thus clinicians are often left to rely on PAC alone.10 It is important to interpret the PAC concurrently with the cat's potassium concentration, since potassium is the main determinant of aldosterone secretion.6 A PAC within or above the laboratory's reference interval is inappropriate in a cat that is volume-overloaded or hypokalemic.
ACTH stimulation
ACTH is an additional stimulant of aldosterone production and can also be used to evaluate adrenal mineralocorticoid production.9 Exogenous ACTH administration causes a reliable increase in aldosterone secretion. A standard dose of cosyntropin (125 μg/cat intravenously) has been used for ACTH stimulation tests traditionally.8 However, a recent study has determined that a cosyntropin dose of 2.5 μg/kg given intravenously will cause a peak aldosterone response analogous to that obtained with the 125-μg/cat intravenous dose, and blood sample collection after cosyntropin administration can be obtained 15 to 75 minutes after administration with no significant difference in aldosterone concentration.8
If it is necessary to evaluate plasma cortisol response simultaneously, then a cosyntropin dose of 5 μg/kg given intravenously is recommended, with a sample collected 60 to 75 minutes after stimulation.8 When evaluating a cat for primary hyperaldosteronism, an ACTH stimulation test is typically unnecessary, and diagnosis can usually be made from the PAC alone.
Future alternative testing
Ideally, a test using an agent that will suppress aldosterone production in healthy cats but have little to no effect in those with primary hyperaldosteronism would be the best method to confirm a suspected diagnosis and prove that hyperfunction of the zona glomerulosa is the cause of an elevated PAC. In people, several tests have been developed to show that an elevated aldosterone:renin ratio is due to primary hyperaldosteronism, including a captopril stimulation test, oral sodium loading, saline infusion, and a fludrocortisone suppression test.5 Since such diagnostic tests have yet to be developed and validated in cats, the patient's clinical presentation, electrolyte concentrations, PAC, and diagnostic imaging all need to be taken into consideration to make a diagnosis.
DIAGNOSTIC IMAGING
Imaging should be performed in all cats that you suspect have primary hyperaldosteronism, and it is a necessity in those cats whose screening tests indicate abnormal regulation of aldosterone production. Determining the laterality of disease is important to direct proper treatment, as unilateral primary hyperaldosteronism can potentially be cured surgically, while bilateral or confirmed metastatic disease should be managed medically.
Abdominal ultrasonography, magnetic resonance imaging (MRI), and computed tomography (CT) can be used to identify adrenal abnormalities and potentially evaluate distant metastases to other abdominal organs and local invasion of the tumor into the caudal vena cava and surrounding structures. Thoracic radiography can be used to detect the presence of pulmonary metastases.
What to look for
In cats, the most common ultrasonographic changes observed with primary hyperaldosteronism include adrenal masses, adrenal calcification, and changes in adrenal echogenicity (Figure 2).11,12,14,18 In cases of unilateral adrenal masses, the contralateral adrenal gland can appear normal or may not be able to be visualized ultrasonographically. The median dorsoventral width of the adrenal glands of healthy cats has been reported to be 3.9 mm for the left (range: 3 to 5.3 mm) and 3.9 mm for the right (range: 2.9 to 4.5 mm).9,22 Results have also shown that parameters of body size, including body weight and surface area, were not significant determinants of adrenal dimensions in cats, thus allowing for a single reference interval for all cats.22
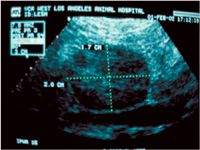
2. An ultrasonogram of a unilateral adrenal tumor measuring 1.7 x 2 cm. Note the enlarged, rounded hypoechoic appearance of the adrenal gland with architectural loss.
The observed morphology of normal feline adrenal glands has been described as bean-shaped to ovoid and hypoechoic to the surrounding tissue.22 In one case series, dorsoventral measurements of ultrasonographically confirmed unilateral adrenal masses ranged from 1 to 3.5 cm, and some showed evidence of compression, close association with the caudal vena cava, or both.12 Finding an enlarged adrenal gland or mass is not definitive for a diagnosis of primary hyperaldosteronism, as other considerations for these findings include pheochromocytomas, cortisol-secreting tumors, nonfunctional tumors, and progesterone-secreting tumors.17
Limitations
Diagnostic imaging has limitations associated with identifying the underlying cause of primary hyperaldosteronism. Functional tumors and clinically relevant hyperplasia of the zona glomerulosa may not be large enough to be revealed by conventional diagnostic imaging techniques, and adrenal glands could appear normal. One cat was determined via ultrasonography to have a right adrenal mass and a normal left adrenal gland, but postmortem examination revealed bilateral adrenocorticol adenomas.12 In another report of 11 cats with histologic confirmation of primary hyperaldosteronism, diagnostic imaging with ultrasonography revealed absent to minor changes in the size and morphology of the adrenal glands.6 Two of these cats had CT performed in addition to ultrasonography, which also revealed no abnormalities of the adrenal glands, but nodular hyperplasia was confirmed by histologic examination.6
These cases suggest that primary hyperaldosteronism due to idiopathic bilateral nodular hyperplasia probably occurs more frequently than is reported and that this disease is not always associated with an adrenal tumor or ultrasonographic abnormalities. Distant metastatic disease in cases of adrenocorticol adenocarcinomas can be missed if their size is below the detection limit of the imaging technique, as occurred in one cat in which thoracic radiographs failed to reveal a 3-mm pulmonary metastatic nodule.23
SUMMARY
Feline primary hyperaldosteronism has become increasingly recognized and diagnosed in cats, and its prevalence is likely underestimated. CKD is often thought to be the causal disorder for cases with classic presenting signs, when, in fact, CKD may be a consequence of primary hyperaldosteronism.
Screening for this disease should be performed in any cat presenting with hypokalemia or hypertension, as well as the subset of cats presenting with mild azotemia, if preliminary minimum database diagnostics fail to identify other underlying disease processes. Diagnostic tests should include a complete physical examination, complete blood count, serum chemistry profile, total T4 measurement, urinalysis, and blood pressure measurement.
If primary hyperaldosteronism is suspected, the plasma aldosterone concentration should be measured and compared with a concurrent serum potassium concentration. Abdominal ultrasonography can be pursued to attempt to differentiate neoplasia from nodular hyperplasia and determine the laterality of disease, but the adrenal glands could also appear normal.
In the next article, find out when medical or surgical treatment is recommended and the likely prognosis for affected cats.
Joseph Bisignano, DVM
Department of Veterinary Clinical Sciences
College of Veterinary Medicine
University of Minnesota
St. Paul, MN 55108
David S. Bruyette, DVM, DACVIM VCA
West Los Angeles Animal Hospital
1818 S. Sepulveda Blvd.
Los Angeles, CA 90025
Veterinary Diagnostic Investigation and Consultation
26205 Fairside Road
Malibu, CA 90256
REFERENCES
1. Conn JW. Presidential address: I: Painting background. II: Primary aldosteronism, a new clinical syndrome. J Lab Clin Med 1955;45(1):3-17.
2. Douma S, Petidis K, Doumas M, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet 2008;371(9628):1921-1926.
3. Fogari R, Preti P, Zoppi A, et al. Prevalence of primary aldosteronism among unselected hypertensive patients: a prospective study based on the use of an aldosterone/renin ratio above 25 as a screening test. Hypertens Res 2007;30(2):111-117.
4. Eger CE, Robinson WF, Huxtable CR. Primary hyperaldosteronism (Conn's syndrome) in a cat: A case report and review of comparative aspects. J Soc Adm Pharm 1983;24:293-307.
5. Djajadiningrat-Laanen S, Galac S, Kooistra H. Primary hyperaldosteronism: expanding the diagnostic net. J Feline Med Surg 2011;13(9):641-650.
6. Javadi S, Djajadiningrat-Laanen SC, Kooistra HS, et al. Primary hyperaldosteronism, a mediator of progressive renal disease in cats. Domest Anim Endocrinol 2005;28(1):85-104.
7. Aguilera G, Catt KJ. Participation of voltage-dependent calcium channels in the regulation of adrenal glomerulosa function by angiotensin II and potassium. Endocrinology 1986;118(1):112-118.
8. DeClue AE, Martin LG, Behrend EN, et al. Cortisol and aldosterone response to various doses of cosyntropin in healthy cats. J Am Vet Med Assoc 2011;238(2):176-182.
9. Zimmer C, Hörauf A, Reusch C. Ultrasonographic examination of the adrenal gland and evaluation of the hypophyseal-adrenal axis in 20 cats. J Small Anim Pract 2000;41(4):156-160.
10. Schulman RL. Feline primary hyperaldosteronism. Vet Clin North Am Small Anim Pract 2010;40(2):353-359.
11. Flood SM, Randolph JF, Gelzer AR, et al. Primary hyperaldosteronism in two cats. J Am Anim Hosp Assoc 1999;35(5):411-416.
12. Ash RA, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: a series of 13 cases. J Feline Med Surg 2005;7(3):173-182.
13. Ahn A. Hyperaldosteronism in cats. Semin Vet Med Surg (Small Anim) 1994;9(3):153-157.
14. MacKay AD, Holt PE, Sparkes AH. Successful surgical treatment of a cat with primary aldosteronism. J Feline Med Surg 1999;1(2):117-122.
15. Reusch CE, Schellenberg S, Wenger M. Endocrine hypertension in small animals. Vet Clin North Am Small Anim Pract 2010;40(2):335-352.
16. Rose SA, Kyles AE, Labelle P, et al. Adrenalectomy and caval thrombectomy in a cat with primary hyperaldosteronism. J Am Anim Hosp Assoc 2007;43(4):209-214.
17. DeClue AE, Breshears LA, Pardo ID, et al. Hyperaldosteronism and hyperprogesteronism in a cat with an adrenal cortical carcinoma. J Vet Intern Med 2005;19(3):355-358.
18. Moore LE, Biller DS, Smith TA. Use of abdominal ultrasonography in the diagnosis of primary hyperaldosteronism in a cat. J Am Vet Med Assoc 2000;217(2):213-215,197.
19. Maggio F, DeFrancesco TC, Atkins CE, et al. Ocular lesions associated with systemic hypertension in cats: 69 cases (1985-1998). J Am Vet Med Assoc 2000;217(5):695-702.
20. Brown S, Atkins C, Bagley R, et al. Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med 2007;21(3):542-558.
21. Javadi S, Slingerland LI, van de Beek MG, et al. Plasma renin activity and plasma concentrations of aldosterone, cortisol, adrenocorticotropic hormone, and alpha-melanocyte-stimulating hormone in healthy cats. J Vet Intern Med 2004;18(5):625-631.
22. Zatelli A, D'Ippolito P, Fiore I, et al. Ultrasonographic evaluation of the size of the adrenal glands of 24 diseased cats without endocrinopathies. Vet Rec 2007;160(19):658-660.
23. Rijnberk A, Voorhout G, Kooistra HS, et al. Hyperaldosteronism in a cat with metastasised adrenocortical tumour. Vet Q 2001;23(1):38-43.