Gallbladder mucoceles: Surgery still recommended due to risk of rupture
In a recent publication (Walter, R., Dunn, M.E. et al. Nonsurgical resolution of gallbladder mucocele in two dogs. JAVMA, Vol 232, No. 11, June 1, 2008), the authors describe medical resolution of gallbladder mucoceles in two canine patients.
In a recent publication [Walter, R., Dunn, M.E. et al. Nonsurgical resolution of gallbladder mucocele in two dogs. JAVMA, Vol 232, No.11, June 1, 2008], the authors describe medical resolution of gallbladder mucoceles in two canine patients.
Presenting clinical signs and physical-exam findings in both patients were non-specific. Both were diagnosed with a gallbladder mucocele by ultrasound imaging. The first patient had a two-month history of inappetence, vomiting and diarrhea. The other had a history of intermittent diarrhea and recurrent otitis. Serum biochemical profiles detected elevations in ALP, ALT, GGTT and hypercholesterolemia. Complete blood counts showed elevations in the white blood-cell counts.
The first patient was treated with S-adenosyl-methionine, omega 3 fatty acids, famotidine, ursodiol and levothyroxine. After three months the clinical signs improved, and there was no ultrasonographic evidence of the gallbladder mucocele. This patient was lost to follow-up after the three-month recheck.
The second patient was treated with fenbendazole, ursodiol and levo-thyroxine and fed a hypoallergenic diet. Follow-up ultrasound exams showed the gallbladder mucocele began to resolve after one month of treatment. It was completely resolved four months later as determined by ultrasound imaging.
Even though these two reported cases suggest that surgery may not be necessary in all cases of canine gallbladder mucoceles, the authors recommend surgical intervention in all patients with gallbladder mucoceles in light of the high risk of eventual rupture and subsequent development of bile peritonitis.
For medical management, recommendations include regular physical examinations, biochemical profiles, ultrasound examinations and solid communication with the referring veterinarians and owners.
Dr. Heidi Hottinger, in Kirk's Current Veterinary Therapy XIV, states that medical management may not be successful, in part, because, at the advanced stage at which many mucoceles are diagnosed, it is difficult to dissolve the semisolid mucoid material so that it may easily exit the gallbladder (Photo 1).
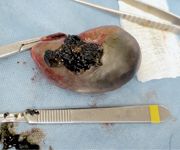
Photo 1: Post cholecystectomy. Note the turgidity and the semisolid material found inside the gallbladder.
Gallbladder mucoceles have been reported with more frequency over the last 30 years. They have distinct gross, histological and ultrasonographic characteristics.
In humans, the pathogenesis of mucoceles is felt to be a result of a functional or structural obstruction of the cystic or common bile duct. Studies have not shown this to be the case in the canine population. Dr. Hottinger says the development of the mucocele is believed to be caused by the dysfunction and proliferation of the mucus-secreting glands of the gallbladder, somehow resulting in an accumulation of the mucoid component of bile within the gallbladder.
Even though underlying hypo-thyroidism, hepatic disease, hyperadrenocorticism, chronic pancreatitis and diabetes have been suggested as predisposing factors for the formation of gallbladder mucoceles, no current studies support these claims. Therefore, one should consider additional diagnostics in all patients with gallbladder mucoceles to rule out other possible underlying causes (Table 1).

Table 1: Recommended diagnostic plan for patients with gallbladder mucoceles
Common blood test abnormalities include elevated liver enzyme activities, hypercholesterolemia and elevated white blood-cell counts.
Mucoceles are reported to be a major cause of extra-hepatic biliary obstructions, leading to gallbladder rupture in more than 50 percent of cases. Some are found incidentally while others are associated with non-specific clinical histories and physical-exam findings. These findings may include abdominal pain, tachycardia, icterus and fever. Clinical signs usually are acute to sub-acute and may include inappetence, vomiting, lethargy, increased drinking, increased urination and diarrhea.
Abdominal ultrasound is reported to be the most sensitive diagnostic test for gallbladder mucoceles. Nyland et al., in Small Animal Diagnostic Ultrasound (2nd edition), characterize mucoceles as having a thickened gallbladder wall, gallbladder distension, biliary sludge/mass effect that does not move with patient repositioning, intraluminal membranes and a "kiwi" or stellate pattern to the sludge (Photo 2).

Photo 2: Ultrasound image of an immature gallbladder mucocele showing a distinct "stellate" or "kiwi" pattern.
The treatment of choice is surgery via cholecystectomy, especially when there is clinical or biochemical evidence of hepatobiliary disease. At surgery it is common to find localized peritonitis that may progress to a generalized bile peritonitis if the disease progresses. Most bile sample cultures yield negative results in these patients.
If necrosis of the common bile duct is present, the prognosis is grave. Reported complications include preoperative and postoperative pancreatitis. As mentioned, full-thickness biopsies of multiple tissues should be obtained at surgery, including frozen liver samples for mineral analysis.
Early surgical intervention (before severe abnormalities develop in the hepatobiliary system) is essential for a favorable outcome in most patients with a biliary mucocele. The most significant danger appears to be in the immediate post-operative period, during which there can be significant mortality rates.
Dr. Lyman is a graduate of The Ohio State University College of Veterinary Medicine. He completed a formal internship at the Animal Medical Center in New York City. Lyman is a co-author of chapters in the 2000 editions of Kirk's Current Veterinary Therapy XIII and Quick Reference to Veterinary Medicine.
Dr. Runde is a 2001 graduate of the University of Pennsylvania School of Veterinary Medicine. He completed an internship at Hollywood Animal Hospital. He is an associate veterinarian at the Animal Emergency and Referral Center, Ft. Pierce, Fla., where he has been an internal medicine resident since 2007.