Get your fix on fracture repair
We all know orthopedic surgery and fracture repair is sexy, but does that mean you should be performing it? Veterinary surgeon Dr. David Dycus addresses this question, and more.For the average general practitioner, performing complex fracture repairs lives in the realm of referrals. Whether you repair or refer, there are important rules and new techniques that David Dycus, DVM, MS, CCRP, DACVS (small animal), wants you to know.Fracture repair is NOT typically an emergency surgery
For the average general practitioner, performing complex fracture repairs lives in the realm of referrals. Whether you repair or refer, there are important rules and new techniques that David Dycus, DVM, MS, CCRP, DACVS (small animal), wants you to know.
Fracture repair is NOT typically an emergency surgery
Many patients that present for fracture repair are victims of vehicular trauma. It's imperative to check and stabilize vitals on these patients before working up any lameness, Dr. Dycus says. HBC patients can suffer from pulmonary contusions and arrhythmias secondary to traumatic myocarditis. Letting them recover a couple of days before attempting surgery usually resolves these life-threatening issues.
Dr. Dycus recommends thoracic and abdominal radiographs, with or without AFAST, and bloodwork. And don't forget proper analgesia as soon as possible with a pure mu agonist, such as morphine, hydromorphone, oxymorphone, methadone or fentanyl. Butorphanol is not adequate, Dr. Dycus says.
Client commmunication tip: Have a problem with commitment?
When surgical plans change, clients can feel like it's a bait and switch, even when we know it's not. When presenting a surgical plan, Dr. Dycus likes to have options. He knows that you really can't commit to one surgical fixation technique until you get in there. When presenting a surgical plan to clients, he says, “I will either do option A or option B. There may also be option C, but I don't know until I am in surgery. You need to trust me that I will fix the fracture the way I feel is best.”
Why exactly is that patient not walking?
While a fracture may be evident on radiographs, it may not be the only reason your patient isn't walking. Perform thorough orthopedic and neurologic examinations, and advise your client about the risk of temporary or permanent nerve damage. Dr. Dycus says neuropraxia can cause temporary deficits, distal humeral fractures can cause radial nerve damage, and ilial fractures can damage the sciatic nerve, even to the point of shearing right through the nerve.
Open fracture? Cover that up ASAP!
No matter how dirty, infected or nasty that open fracture is or how clean you think your hospital is, the bacteria that rode in on that wound will be no match to super bugs that are lurking in your clinic. Dr. Dycus advises covering open fracture wounds with a sterile dressing as soon as possible to prevent implant infection, osteomyelitis and potential sequestrum formation.
Dr. Dycus recommends flushing open fracture wounds with copious amounts of sterile saline solution, to the tune of 2 to 4 liters. He advises against using dilute povidone-iodine or chlorhexidine to avoid potential cytotoxicity-the success of your fracture repair will depend on healthy tissue. He also recommends the use of external skeletal fixators for open fractures in order to access the wounds daily for cleaning and inspection.
See both sides of the issue
If there is one thing Dr. Dycus wants you to remember, it is to take orthogonal radiographs. This includes at least two views-a lateral and a craniocaudal-of any fracture. Fracture classification depends on six factors: anatomic location, severity, configuration, whether or not a growth plate is involved, contamination and displacement. Dr. Dycus says you can NOT determine displacement without orthogonal views. “For example, in Figure 1 and Figure 2, if you took just a lateral radiograph, the fracture may be missed,” says Dr. Dycus. “By taking orthogonal views, you can see there is a right Salter-Harris IV distal lateral humeral condylar fracture.”

Figure 1. A lateral radiograph. All looks good! (Photos courtesy of Dr. David Dycus)

Figure 2. In a craniocaudal radiograph of the same limb as in Figure 1, a fracture is evident.External coaptation or internal fixation? Now THAT is the question.
Now that you know you have a fracture, the question is how do you fix it? Surgical repair will lead to earlier return to function and may better to maintain joint motion, but when is it clearly indicated?
According to Dr. Dycus, correct application of external coaptation requires immobilization of the joint proximal and distal to the fracture, and it should only be used in fractures distal to the elbow and stifle.
Dr. Dycus says internal fixation is indicated for fractures that are subjected to compression, shearing, or tensile forces, that are comminuted or long oblique, or that cannot be reduced appropriately. Use the 50/50 rule to determine whether or not reduction is appropriate. The 50/50 rule, according to Dr. Dycus, states that fracture ends should have at least 50% contact to expect fracture healing, and 50% reduction (contact) is the absolute minimum for bone healing to be possible, not probable. If the fracture cannot be reduced at least 50%, then internal fixation is indicated.
Ethical questions, #tbh
Even if you know you can repair a fracture, Dr. Dycus advises to ask yourself if you really should. Fracture repair is highly individualized based on fracture classification; configuration of the fracture (transverse, oblique, spiral); the patient's age, activity level, and body condition; any comorbidities; and client finances and postoperative compliance. Additional factors include the availability of fixation techniques and your own experience and skill set. If you are going to repair fractures, then Dr. Dycus stresses the need to have multiple types of implants available. The downside is implant sets are expensive. If you only have intramedullary pins and cerclage wires, then ethically, you are limited as to what type of fractures you should repair.
It doesn't have to be pretty
The first stage of secondary bone healing after trauma is hematoma formation. You may be tempted to remove the hematoma to get better visualization. Don't! This hematoma is a massive source of growth factors and cytokines that establish the blood supply needed for healing, says Dr. Dycus. Leave it there. Furthermore, leave bony fragments that have soft tissue attachments. The body will reabsorb fragments or incorporate them into the bony callous.
Dr. Dycus goes on to say that the historical technique of fracture repair was complete anatomic construction, very neat and clean with everything put back in its place, similar to the work of a carpenter. The downside to this technique is hematoma and blood flow disruption, which delays healing. Carpenter-type fracture repair is now only indicated for fractures that involve the articular surface.
The new thought process is less like a carpenter and more like an organic gardener. The idea is to be minimally invasive, be friendly to tissues, and use indirect fracture reduction to preserve blood flow, says Dr. Dycus. Blood supply comes from the surrounding soft tissues, so be kind. Overall, joint alignment and function is the goal of fracture repair. Neatness doesn't count.
What is MIPO and why should you care?
Do you know what MIPO is? It stands for minimally invasive plate osteosynthesis. Dr. Dycus says this technique involves using fluoroscopy to reduce the fracture and then sliding a long plate in via stab incisions. MIPO is rapidly becoming popular and could have benefits for your patients with various fractures-yet another good reason (I think) to refer.

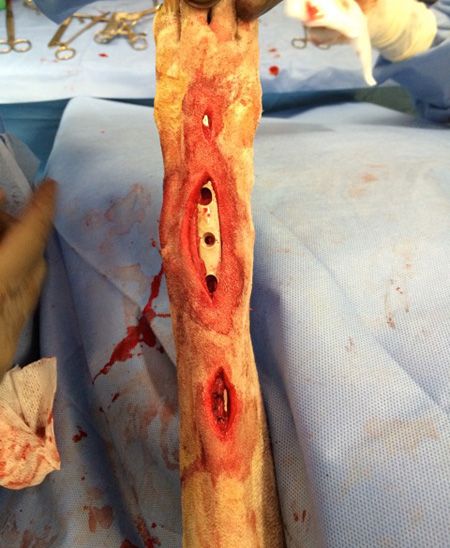
Figures 3 and 4: Intraoperative photos of MIPO.Keep calm and mind the gap
One final note: If you are rechecking your fractures at four weeks following external coaptation or after surgery and notice that the fracture line seems to have widened slightly, don't panic! “Part of the healing process involves the fracture maintaining an interfragmentary strain of < 2%,” says Dr. Dycus. “The interfragmentary strain is the deformation occurring at the fracture site relative to the size of the gap. By keeping the interfragmentary strain < 2% the body is able to allow bone to be laid down in the fracture gap.” This process can cause apparent widening of the fracture line seen on radiographs and can give you the wrong impression that that fracture is getting worse! Understanding this phenomenon will help you interpret your radiographs and, more important, help you sleep at night.










