Insulinoma in a senior pit bull: Medical perspective
Dr. Lauren Adelman provides the medical perspective on this challenging veterinary oncology case.

Dr. Lauren AdelmanThe pancreas is composed of two main tissue types; the acini that secrete digestive enzymes into the duodenum, and the islets of Langerhans that contain alpha, beta, delta and pancreatic-polypeptide cells (Figure 1).
The alpha cells make up about 25% of all islet cells and secrete glucagon, which raises the blood glucose concentration.1 The delta cells comprise about 10% of the total cell population and secrete somatostatin, a polypeptide that decreases insulin and glucagon production and motility of the stomach, duodenum and gallbladder.1 Beta cells make up most of all islet cells (60% to 75%) and secrete insulin, the major glucose-lowering hormone, along with amylin whose function remains unclear.1
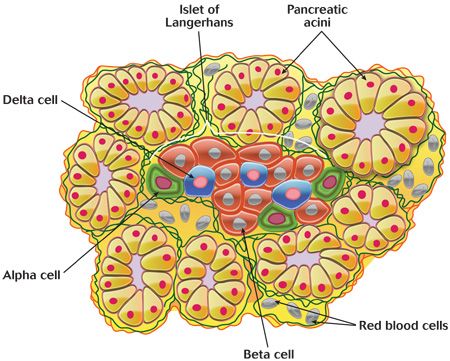
Figure 1. The physiologic anatomy of the pancreas. (Illustration by Mathews)Insulin promotes uptake, storage and use of glucose by a variety of tissues, including the liver, muscle and adipose tissue. In the liver, insulin promotes glycogen synthesis and decreases gluconeogenesis. Insulin also promotes both fat and protein synthesis and storage. The blood glucose concentration is normally maintained within a narrow physiologic window between 70 and 110 mg/dL.2 When the blood glucose concentration becomes too high (greater than 100 to 110 mg/dl), insulin secretion from beta cells increases. In contrast, when the blood glucose decreases below a certain threshold (about 60 mg/dl), insulin secretion stops, thereby raising blood glucose back to normal concentrations.
Insulinomas are functional insulin-secreting tumors arising from the beta cells of the islets of Langerhans. These neoplastic beta cells secrete insulin continuously and are not responsive to the normal negative feedback of hypoglycemia.2 As a result, patients experience intermittent and recurrent periods of hypoglycemia. Compensatory mechanisms for hypoglycemia include inhibition of insulin secretion and release of counter-regulatory hormones (glucagon, catecholamines, growth hormone and glucocorticoids).3 Most clinical signs result from the effect of hypoglycemia on the brain (neuroglycopenia) or hypoglycemia-induced release of catecholamines. Clinical signs of neuroglycopenia include weakness, ataxia, nervousness, disorientation, dullness or seizures.3 Clinical signs related to catecholamine release and stimulation of the sympathetic nervous system include tremors, increased appetite and nervousness.3 Signs of hypoglycemia may also be exacerbated by excitement, exercise or fasting.4
Differential diagnoses for insulinoma include other causes of hypoglycemia in dogs. These can be organized into four major categories.
- The first category includes conditions that result in excess secretion of insulin or insulin-like factors, including islet cell hyperplasia and paraneoplastic syndromes of nonpancreatic tumors (i.e. hepatocellular carcinoma, leiomyoma, lymphoma).2,3
- The second category includes diseases resulting in decreased glucose production such as extreme malnutrition or starvation, neonate or toy breed hypoglycemia, hepatic insufficiency (portosystemic shunt, glycogen storage disease, cirrhosis), hormone deficiency (i.e. hypoadrenocorticism, hypopituitarism, growth hormone deficiency) and hunting dog hypoglycemia.2,3
- The third group of conditions result in hypoglycemia secondary to increased glucose consumption such as that which occurs with sepsis, extreme exercise, polycythemia, periparturient hypoglycemia and artifact secondary to prolonged storage of blood before separation of serum and plasma.3
- The fourth category includes exogenous substances that may result in hypoglycemia, such as insulin overdose, xylitol toxicosis and a variety of drugs that have been reported to result in hypoglycemia in human patients (sulfonylurea, propranolol, high-dose aspirin, acetaminophen and many others).2,3
Clinical suspicion of insulinoma is based on appropriate clinical signs and documentation of hypoglycemia with concurrent elevated insulin. Further diagnostic work-up may include imaging to document the presence of a pancreatic mass and histopathology.
References
1. Guyton AC, Hall JE. Insulin, glucagon and diabetes mellitus. In: Textbook of medical physiology. 12th ed. Philadelphia: Elsevier, 2011.
2. Goutal CM, Brugmann BL, Ryan KA. Insulinoma in dogs: a review. J Am Anim Hosp Assoc 2012;48:151-163.
3. Ettinger SJ, Feldman EC. Insulin secreting islet cell neoplasia. In: Textbook of veterinary internal medicine. 6th ed. Philadelphia: Elsevier, 2005.
4. Steiner JM, Bruyette DS. Canine insulinoma. Compend Contin Educ Pract Vet 1996;18:13-25.
Podcast CE: A Surgeon’s Perspective on Current Trends for the Management of Osteoarthritis, Part 1
May 17th 2024David L. Dycus, DVM, MS, CCRP, DACVS joins Adam Christman, DVM, MBA, to discuss a proactive approach to the diagnosis of osteoarthritis and the best tools for general practice.
Listen