Managing cats in respiratory distress (Proceedings)
Cats with respiratory distress represent a significant diagnostic and therapeutic challenge to the small animal veterinarian.
Cats with respiratory distress represent a significant diagnostic and therapeutic challenge to the small animal veterinarian. The most common causes of feline respiratory distress are pulmonary edema, pleural effusion, asthma, and neoplasia. Trauma may also cause respiratory distress, but it typically clear on examination. Available methods to try to elucidate the etiology of an individual cat's respiratory distress include evaluation of historical and physical examination findings, thoracic radiography, cytology and ultrasonography or echocardiography. Additionally, it is important to distinguish respiratory distress that is a presenting complaint from respiratory distress that develops during hospitalization for another problem and to quantify distress as mild, moderate, severe or immediately life-threatening.
Respiratory distress at presentation
Respiratory distress as a presenting complaint is a common condition for the emergency feline practitioner. Additionally, it is well-recognized that cats with respiratory difficulty are challenging to treat, as these cats create a large amount of (appropriate!) anxiety in many veterinarians, due to fears of either excessive stress associated with therapy or difficulty with determining the underlying diagnosis.
Pertinent historical findings may include a previous diagnosis of heart or lung disease. Many owners recall a prior diagnosis of a heart murmur, or past episodes of coughing which may suggest airway disease. Additionally, while cats have a lower incidence of traumatic pulmonary contusion or pneumothorax than dogs, access to the outdoors may support a traumatic etiology. Other factors, such as signalment and progression of clinical signs are less frequently helpful, although hypertrophic cardiomyopathy is more common in male cats and the Siamese breed has a reportedly higher incidence of airway disease.
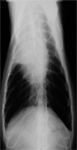
Figure 1. Ventrodorsal and lateral thoracic radiographs of a 13 year old cat with a history of congestive heart failure with pleural effusion, which had been presented with moderately severe tachypnea. Empiric thoracocentesis had been unproductive, and radiography was performed to better evaluate the thorax. The VD view documents a right cranial lung lobe torsion, likely secondary to the prior effusion.
Physical examination findings are often helpful in determining the cause of feline respiratory distress. The body temperature is frequently subnormal in cats with heart disease, but is generally normal or even elevated with pulmonary disease. Similarly, an elevated heart rate (>200 bpm) is often associated with heart failure, while cats with primarily respiratory disease may have a slower heart rate. However, cats who are hypothermic due to heart disease may be relatively bradycardiac as well. The presence of a heart murmur, gallop rhythm or arrhythmias is strong evidence for cardiac disease. Jugular venous distension may be present with heart disease, although some evidence suggests that jugular distension may accompany pleural effusion of any etiology. The heart failure cat rarely presents with ascites. Crackles may be present with both pulmonary edema and asthma. Diminished respiratory sounds, particularly ventrally, often signifies pleural effusion as does a significant abdominal component to respiration. Cats with severe pleural effusion may occasionally appear to have upper airway obstruction.
Thoracic Radiography
Thoracic radiography is quite useful in determining the etiology of respiratory distress. It is very important to remember that radiographs are not therapeutic, and should not be performed prior to stabilization. It is not necessary to have a perfect exposure and patient positioning. A cat with marked respiratory distress that is not responding to stabilization will often be content to lie directly on a radiographic cassette for a DV thoracic view that may then provide information without undue stress. Interpretation of radiographs may document the presence of cardiomegaly, pulmonary edema, pleural effusion, or a prominent bronchial pattern. The radiographic distribution of cardiogenic pulmonary edema in cats is variable
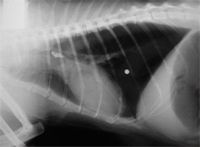
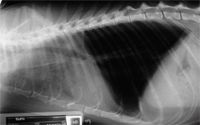
Figure 2. A lateral thoracic radiograph of a 14 year old cat with an acute onset of respiratory distress. The physical examination was unremarkable except for the respiratory distress. A tracheal foreign body (tooth) is evident in the region of the carina. The pellet was an incidental finding and located in the subcutaneous tissues. The stomach was also distended with air secondary to aerophagia. The tooth was removed with the aid of fluoroscopy and the cat made an uneventful recovery.
Frequently, after evaluation of the historical and physical examination findings, and interpretation of the thoracic radiographs, it is possible to determine whether heart or lung disease is the most likely cause for the respiratory distress. If pulmonary infiltrates compatible with edema are present on thoracic radiographs, the cat should be treated with diuretics, oxygen, cage rest and possibly vasodilators. In our practice, furosemide (1-4 mg/kg im or iv q 2-6 hours) is most frequently used. An intravenous catheter is ideal, and may often be placed with minimal restraint. However, if a cat seems to struggle, catheter placement should be stopped immediately and furosemide administered intramuscularly. Oxygen is most easily administered by placing the cat within an oxygen cage. Nitrogylcerin may be applied topically in the pinna or on the lateral thoracic (after clipping the fur) to help promote vasodilation. In severe cases, nitroprusside (0.5-5 μg/kg/min in 2-3 ml D5W/hr may be used. Diffuse pulmonary infiltrates may also be present with hemorrhage, pneumonia or metastatic neoplasia. Severe lower airway disease may mimic metastatic neoplasia.
If a moderate to large volume of pleural effusion is present, it should be removed in order to improve the stability of the cat as well as to help aid in reaching the final diagnosis. Thoracocentesis is performed by first clipping a small amount of fur at the 7-9th intercostal space at the costochondral junction. The skin should be sterilely prepared and then thoracocentesis performed by carefully advancing a butterfly catheter (21gauge) through the skin and into the chest cavity. The intercostal vessels, which run on the caudal aspect of the rib, should ideally be avoided, but in practice this may be hard to appreciate in an average-sized cat. All the available fluid should be withdrawn. An aliquot of fluid should be retained in a serum tube and EDTA tube for culture (if indicated) and cytology respectively. As cats do not have an intact mediastinum, it is rare for fluid to pocket on only one side of the chest. However, it is common to try to retrieve fluid from both sides of the chest. Occasionally, in large or obese cats, it is necessary to use a longer needle (1.5 inch 22 gauge needle with an extension set) in order to enter the chest cavity. Cats with chronic effusions (eg. Chylothorax) may have fibrosis of the pleural; this may predispose them to iatrogenic pneumothorax after thoracocentesis. Cytologic analysis of thoracic fluid, when present, may be diagnostic of heart disease, pyothorax, chylothorax or neoplasia.
Thoracic radiographs may also document bronchial infiltrates compatible with allergic airway disease. Occasionally, mild right-sided cardiomegaly (cor pulmonale) is also appreciated. After stabilization with oxygen and glucocorticoids, a transoral tracheal wash may be performed to evaluate the cat for signs of airway inflammation, infection or respiratory parasites. A transoral tracheal wash is performed by first pre-oxygenating the cat, then inducing a moderate place of anesthesia with propofol (2-10 mg/kg iv SLOWLY). A sterile tracheal tube should be placed and then 3-5 ml aliquots of sterile saline should be infused and the aspirated back through the tube. Frequently, better yields are obtained if the tube is also allowed to drain into a sterile specimen cup. Heartworm and lung worm testing is warranted in cats from endemic areas.
Finally, in some cats with respiratory distress, echocardiography is required to document the presence or absence of heart disease. Heart disease can be present without auscultable abnormalities, and not all murmurs (even in dyspneic cats!) are associated with heart disease. Echocardiography in particular is useful to document cardiac function and to assess for signs of left atrial enlargement. Echocardiography should not be performed if a patient has marked respiratory distress.
Respiratory distress developing in the hospital
Occasionally, a hospitalized cat will develop moderate to severe respiratory distress while being treated for some other unrelated disease. While in dogs a differential list of aspiration pneumonia, pulmonary thromboembolism, acute respiratory distress syndrome (ARDS) or fluid overload/heart failure may exist, in cats, almost all new onset respiratory distress is volume overload. Cats have a smaller intravascular space that dogs, and several days of "3X maintenance fluids" will trigger volume overload in many cats. Echocardiograpy or radiography may document previously occult heart disease and appropriate therapy involves decreasing or stopping the fluids and thoracocentesis (if a large volume of fluid is present).

Figure 3. Thoracic radiographs from a 7 year old cat before (left) and after (right) receiving intravenous fluids for several days for treatment of a urinary obstruction. A grade 2/6 murmur had been ausculted prior to beginning therapy, but respiratory distress did not develop until the morning of the third day. The pulmonary infiltrates resolved with discontinuing the fluids and a single dose of furosemide, but echocardiograpy confirmed hypertrophic cardiomyopathy.
A guide for assessing respiratory emergencies
November 15th 2024Mariana Pardo, BVSc, MV, DACVECC, provided an overview on breathing patterns, respiratory sounds, lung auscultation; and what these different sounds, patterns, and signs may mean—and more—in her lecture at the 2024 NY Vet Show
Read More