Managing dogs with thoracic impalement injuries: A review of nine cases
Thoracic trauma is common in dogs and may result in marked morbidity and mortality because of injury to the lung parenchyma (pulmonary contusion), pleural space (hemopneumothorax), great vessels, thoracic wall (rib fractures), diaphragm, or myocardium.
Thoracic trauma is common in dogs and may result in marked morbidity and mortality because of injury to the lung parenchyma (pulmonary contusion), pleural space (hemopneumothorax), great vessels, thoracic wall (rib fractures), dia phragm, or myocardium.1-5 Thoracic injury may be classified as either blunt, such as vehicular trauma, or penetrating, such as stab wounds. Most cases of penetrating thoracic trauma in animals involve bite wounds in small-breed dogs, although a retrospective study of gunshot wounds at an urban veterinary referral hospital included 32 dogs (39%) with thoracic wounds.5
In people, most penetrating thoracic trauma is from gunshot wounds and stab wounds, although more unusual causes such as golf club injury and swordfish attack have also been described,6-12 as well as a recent well-publicized case involving fatal thoracic impalement from a stingray spine.
Impalement injuries represent an uncommon subset of penetrating trauma, in which the object responsible for the injury is left protruding from the victim or the victim is attached to an object.8 Some impalement injuries, such as those caused by large steel rods in association with motor vehicle accidents, may have components of both blunt force and penetrating trauma.
The tenets of impalement wound management have been well-described in the human medical literature.6-10 It is strongly recommended to leave the object in the individual until the object can be removed under controlled circumstances, either in the emergency room or operating room. Removing impaled thoracic foreign bodies under less-controlled circumstances may be associated with life-threatening hemorrhage or pneumothorax. Additionally, failure to adequately clean and débride the wound increases the risk of pyothorax or incisional infection.13
Conversely, reports concerning impalement injuries in the veterinary literature are limited. Two articles describe the management of penetrating thoracic wounds in horses, while another describes three cats with high-rise syndrome associated with impalement.14-16 In this article, we describe the clinical history, surgical and medical management, and outcomes for a series of dogs with thoracic impalement as well as provide guidelines for the practical management of affected patients.
MATERIALS AND METHODS
We reviewed the surgery logs of the Foster Hospital for Small Animals at Tufts University and Angell Memorial Animal Hospital in Boston from January 1996 to May 2003 to identify all dogs that had undergone thoracotomy for management of thoracic impalement injuries. Cases were included if the object was present within the thorax on presentation or if the object had recently been removed by the dog, owner, or referring veterinarian. Gunshot, stab, and porcupine quill wounds without residual foreign objects were excluded, as were cases with incomplete or missing medical records. The signalment, cause of impalement injury, results of diagnostic imaging, method of object removal, surgical approach, postoperative course, and long-term outcome were recorded for each dog. Collected data were statistically described as either mean ± standard deviation or median and range as appropriate.
RESULTS OF MEDICAL RECORD REVIEWS
Nine cases of thoracic impalement injuries were identified; two cases involved one dog that had two separate impalement episodes. All the dogs were large-breed with a median weight of 70.4 lb (32 kg) and a range of 50.6 to 79.2 lb (23 to 36 kg). Six of the eight dogs were male; five of these were castrated. One female was spayed, and one was intact. Six of the eight dogs were hunting breeds (three Labrador retrievers, a vizsla, a Weimaraner, and a German shorthaired pointer). A Doberman pinscher and a large terrier mix were also affected. The pointer had two separate impalements. The ages at injury ranged from 1 to 6.5 years old with a median age of 3.8 years.
Cause of injury
In seven cases, the impaling object was a stick. One dog fell from a second-story porch onto a branch, while the other six injuries resulted from running into a stick. One Labrador retriever was seen running into a stick, three of the dogs returned from running unobserved in the woods with a stick protruding from their thoraxes, and two were found nonambulatory with a stick protruding from their thoraxes.
In the other two cases, one dog was inadvertently shot with an arrow (Figure 1), and one dog jumped onto a broken plastic door.

Figure: 1. A Labrador retriever that presented after having been inadvertently shot with an arrow during hunting season. The arrow entered the thoracic cavity near the scapula. This dog recovered uneventfully with treatment.
Initial presentation and physical examination findings
Five dogs presented as emergencies immediately after injury, and three dogs were treated by their veterinarians before referral: A Labrador retriever was treated for four days, the Doberman pinscher was treated for two days, and one dog was stabilized and immediately referred for definitive therapy.
In addition to the impalement history, presenting clinical signs in all dogs included tachypnea (respiratory rate > 36 breaths/min) and labored breathing, tachycardia (> 120 beats/min), and apparent pain. Four dogs appeared hypovolemic (based on heart rate, pulse quality, and a delayed capillary refill time), and three dogs were hyperthermic (> 103 F [39.4 C]).
Initial stabilization
All dogs were treated with intravenous fluids on arrival. The dogs received an intravenous bolus (between 10 and 60 ml/kg) of a balanced electrolyte solution. During initial stabilization, all dogs received supplemental oxygen, usually administered as flow-by then either by an oxygen cage or nasal insufflation if further support was necessary. All dogs also received broad-spectrum antibiotics.
Mechanism of object removal
The externally visible portions of four foreign bodies were removed by the dog, the owner, or the referring veterinarian before anesthesia and surgical removal, and five foreign bodies were removed during surgical exploration by the surgeon at the referral hospital.
Laboratory testing
A CBC and serum chemistry profile were performed in all dogs before anesthesia and surgery. In seven dogs, samples were collected after dogs received intravenous rehydration therapy. In one dog, the timing of the sample collection could not be determined from the medical record. All dogs were hypoproteinemic (median total solids = 3.7 g/dl, range = 2 to 4.9 g/dl [reference range = 5.8 to 7.2 g/dl]), and four dogs were anemic (hematocrit < 35%; reference range = 37% to 55%). Three dogs had neutrophilic leukocytosis with a median total white blood cell count of 23,100/μl (range = 17,200 to 26,000/μl [reference range = 6,000 to 17,000/μl]). No other clinically relevant laboratory abnormalities were present in any dog.
Diagnostic imaging
All dogs had a thoracic radiographic examination before surgery. All radio graphs revealed abnormalities, including pleural effusion (eight dogs), subcutaneous emphysema (five dogs), pneumothorax (four dogs), pneumomediastinum (three dogs), and rib fractures (one dog). In five dogs with stick impalement, the stick appeared as a radiolucent area and soft tissue opacities compatible with local soft tissue swelling were present, probably secondary to hemorrhage. Ultrasonography or computed tomography was not used initially in any affected dog.
Surgical treatment
All dogs underwent exploratory thoracotomy a median of 31 hours after the initial injury (range = three to 96 hours). General anesthesia was induced and maintained with a variety of protocols. All dogs had controlled ventilation, either mechanically or manually, during the thoracotomies. Three dogs had lateral thoracotomies, and six dogs had median sternotomies in addition to wound explorations. The entry wound was explored, all foreign objects were removed, and the area was copiously lavaged with sterile saline solution. The surgical order was at the surgeon's discretion; however, most wounds were explored before the thoracotomy was performed.
Additional important intrathoracic injuries were detected in some dogs. Two dogs had full-thickness diaphragmatic lacerations; in each dog the abdomen was explored before the diaphragmatic rent was débrided and sutured. Another dog had severe pulmonary contusions of the right cranial lung lobe near the site of the foreign body penetration, and a complete right cranial lung lobectomy was performed.
One Labrador retriever, whose original injury occurred four days before surgery, had severe pleural thickening and a 5-cm-long stick fragment completely within the pleural space. The other dog, the Doberman pinscher, whose original injury occurred 48 hours before surgery, also had severe gross pleuritis and three stick fragments within the pleural space.
Thoracic closure was routine, with thoracostomy tubes placed in all dogs and additional closed suction (two) or Penrose (one) drains placed appropriately in relation to the wounds at the surgeon's discretion.
Bacterial culture
Samples were collected for aerobic and anaerobic bacterial cultures intraoperatively in six dogs; five culture results were positive. Mixed anaerobic infections were the most common, and bacteria identified included Bacillus species, coagulase-positive Staphylococcus species, Clostridiumsporogenes and Micrococcus species, Clostridium perfringens, Clostridium sordellii, and Enterobacter amnigenus biogroup 2.
Postoperative treatment
After surgery, all dogs were treated with intravenous fluids, analgesics (local and systemic), and antibiotics. Five dogs received supplemental oxygen. In two cases, surgically placed thoracostomy tubes became dislodged and were replaced percutaneously because of large volumes of on-going effusion. Thoracostomy tubes remained in place for a mean of three days (range = one to six days). Thoracostomy tubes were removed based on decreased fluid production. The volume of pleural effusion removed varied considerably from dog to dog, with a mean of 10.1 ml/kg/day and a range of 1.4 to 28.3 ml/kg/day.
The two dogs with the longest duration of medical treatment before definitive surgical exploration and repair (the Doberman pinscher and a Labrador retriever) had marked on-going suppurative effusion for five and six days, respectively. The Doberman pinscher's pleural effusion resolved, while the Labrador retriever was discharged eight days after surgery with mild pleural effusion, which was thought to be resolving, and then returned 48 hours later with respiratory distress. Severe suppurative pleural effusion was identified on radiographic examination (Figure 2). Indwelling thoracostomy tubes were placed, and the effusion finally resolved after 10 additional days of supportive care, including aspiration of the tube every four to six hours and intravenous antibiotics (metronidazole 10 mg/kg every eight hours and enrofloxacin 10 mg/kg every 24 hours). Ultrasonography during this hospitalization documented suspected multiple small intrapleural and intraparenchymal abscesses. The 1- to 3-mm fluid pockets were considered too small to percutaneously drain and too extensive to warrant another thoracotomy.

Figure: 2. A ventrodorsal thoracic radiograph of a Labrador retriever that presented for evaluation of dyspnea 10 days after thoracotomy. Note the wires in the sternebrae and the large volume of primarily right-sided pleural effusion.
Long-term outcome
All the dogs survived to hospital discharge. The dogs were hospitalized for a median of seven days (range = three to 12 days). One Labrador retriever's total hospitalization was 18 days over two admissions.
The German shorthaired pointer developed a draining tract 48 months after the first injury and 12 months after the second injury in a separate site, caudal to the first injury. Thoracic radiographs at this point revealed mild bony proliferation, swelling, and a possible draining tract adjacent to the ninth rib. A subsequent ultrasonographic examination revealed a 3-cm-long echogenic linear foreign body as well as a smaller linear foreign body within a convoluted hypoechoic draining tract. Both foreign bodies were associated with faint acoustic shadowing. Wooden fragments were subsequently removed surgically; they were found in the same region as the first traumatic injury four years earlier and on the same side as the second injury a year earlier.
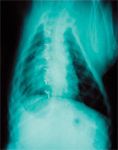
Figure: 3. A ventrodorsal thoracic radiograph of the same dog as in Figure 2 at its six-month recheck after medical therapy for pyothorax. No clinical signs of restricted activity were present, although an increased interstitial pattern is observed.
Follow-up evaluations were obtained in all remaining cases for a mean of two years after surgery (range = five months to nine years). All dogs had been normal at home, and no abnormalities were found on physical examination. The Labrador retriever with the extensive pyothorax had no clinical signs of pulmonary compromise such as exercise intolerance or tachypnea (Figures 3 & 4).

Figure: 4. The Labrador retriever shown in Figures 2 & 3 about six months after recovery. (Photograph courtesy of Deenie Galipeau.)
DISCUSSION
Our results indicate that most thoracic impalement injuries that were managed surgically occurred in young, active large-breed dogs. These dogs were commonly injured by running into sticks protruding from the ground or fallen tree branches and were presented for evaluation of entry wounds in the ventral cervical area or thoracic inlet. Impalement in this location is particularly dangerous because the foreign body may traverse the thorax and damage intrathoracic structures on either side. Fallen wood may be rotten and prone to splintering, leaving debris within the tissues that may lead to chronic pyothorax or draining tracts.
Case management recommendations
Direct your initial diagnostic evaluation of animals with thoracic impalement injuries at determining whether the foreign body entered the thoracic cavity, since this may influence case management including decisions about the location and timing of surgery. Direct the initial therapeutic efforts at stabilizing the patient. The index of suspicion of intrathoracic injury should be high in animals with severe tachypnea or dyspnea.
Radiography and endoscopy
Obtain thoracic radiographs as soon as the patient is stabilized. Although wood and plastic foreign bodies are radiolucent, based on our results, most dogs with intrathoracic impalement injuries have radiographic evidence of damage to thoracic structures. Pleural effusion was noted in all the dogs in this case series, and subcutaneous emphysema, pneumothorax, and pneumomediastinum were also common. Because none of the dogs were found at surgery to have major lacerations of the pulmonary parenchyma, trachea, or esophagus, subcutaneous and intrathoracic air most likely entered the thorax through the entry wounds. However, endoscopy or tracheoscopy may be warranted in certain cases, such as in dogs with massive pneumomediastinum, marked ptyalism, or evidence of dysphagia.
Our study included only dogs that underwent thoracic exploratory surgery, and these dogs were identified by a review of surgical logs. The utility of thoracic radiography for predicting thoracic penetration may be overestimated by our results since it is possible that some dogs with thoracic penetration during this period did not have surgery and that a proportion of these dogs may have had normal thoracic radiographic findings.
Wound exploration and thoracotomy
Wound exploration and exploratory thoracotomy are indicated in all dogs with clinical or radiographic evidence of thoracic penetration.7-9 In animals without apparent thoracic penetration, the wounds should also be explored, and the surgeon should be prepared to enter the thorax if intraoperative exploratory findings dictate it. These findings include a palpable instability of the thoracic wall, evidence of air bubbling from the thorax, or evidence of a tract extending into the thorax. Additionally, in wounds near the diaphragm, the abdominal cavity may require surgical exploration as well.9 Consider emergency surgery in patients with severe respiratory difficulty that cannot be relieved by oxygen administration or percutaneous placement of a thoracostomy tube and in patients with evidence of ongoing intrathoracic hemorrhage. No dog in this study had evidence of severe intrathoracic hemorrhage documented in its medical record. It seems likely that most dogs with a laceration of a great vessel would die before presentation to a veterinary hospital.

Recommendations for managing dogs with impalement injuries
After anesthesia induction, remove any remaining exposed foreign material. If the object cannot easily be removed with gentle traction, cut away the exposed portion and remove the remainder intraoperatively. Using excessive traction to dislodge the object risks enlarging the entry wound or damaging intrathoracic structures. After removing the exposed portion of the foreign object, prepare a wide area surrounding the entry wound for surgery.
Base the choice of a thoracotomy approach on the location of the entry wound and radiographic findings. In patients with entry wounds in the ventral cervical area or near the thoracic inlet, sternum, or spine, use a median sternotomy since structures on either side of the thorax may have been damaged.7,8 For patients with entry wounds on the lateral side of the thorax distant from the midline, an intercostal thoracotomy may be considered, particularly if radiographs suggest that damage is confined to the side of the thorax in which the entry wound is located. A disadvantage of intercostal thoracotomy is that it requires an accurate estimation of the object's entry site into the thorax. If the impaling object passes through the thoracic wall at an oblique angle, it may enter the pleural space several intercostal spaces distant from the site of skin penetration. Additionally, the opposite side of the thorax may have been penetrated. For this reason, use a median sternotomy if you are uncertain about the impaling object's course.
In unstable patients, perform thoracic exploration before wound exploration so that life-threatening intrathoracic injuries can be addressed without delay. All patients with thoracic impalement injuries have the potential to be unstable, so the surgeon and surgery team must be prepared to address any changes in patient status. The surgeon should also be prepared to completely or partially remove damaged lung lobes and to ligate or repair lacerated blood vessels. While only one dog in this case series required lung lobectomy and none of the dogs damaged major vascular structures, it would be prudent to be prepared for any surgical finding.
Once all major intrathoracic damage has been addressed, try to remove all remnants of the foreign body. In many cases, debris from penetrating sticks can be found near the thoracic entry wound. In addition, thoroughly inspect any areas within the thorax that appear discolored or demonstrate evidence of prior hemorrhage. Finally, explore, débride, and lavage the entry wound itself.
The entry wound is best examined while the thorax is open, allowing the surgeon to digitally explore the wound for residual foreign material from both the skin and the thoracic sides. Obtain aerobic and anaerobic bacterial cultures of the wound, and place drains in wounds that appear infected or that have marked dead space that cannot be obliterated during closure. If possible, close the thoracic entry wound to prevent contaminated fluid within the wound tract from entering the thoracic cavity and to prevent postoperative pneumothorax. Place a thoracostomy tube in all patients.
Antibiotic therapy
Thoracic impalement injuries carry a real risk of infection of the wound or thoracic cavity; three of the dogs in this case series developed persistent pyothorax or draining tracts after their initial hospitalization and treatment.13 It is likely that early surgical intervention and removal of all visible foreign material are the most important factors in preventing chronic infections and that antibiotic therapy plays a complementary role.
Our culture results suggest that most dogs have mixed aerobic-anaerobic contamination of tissues, and resistant organisms are uncommon because of the community-acquired source of contamination. (Most multidrug-resistant organisms develop only in the hospital setting with antibiotic use selecting for the resistant strains. In contrast, most bacteria outside of hospitals are susceptible to the common antibiotics as dictated by their intrinsic characteristics. For example, streptococcus is consistently resistant to the fluoroquinolones, while anaerobes are resistant to the aminoglycosides.) So obtain both anaerobic and aerobic cultures during surgery. Institute broad-spectrum antibiotics before surgery if the injury occurred more than a few hours before presentation; otherwise, antibiotics may be instituted after culture samples are obtained. Antibiotic selection should be based on the results of sensitivity testing, if possible. Since a high incidence of anaerobic contamination was noted in our study, antibiotics effective against anaerobes should be administered.
CONCLUSION
The present study was limited by its retrospective nature, the small number of dogs, and the selection of only dogs that underwent thoracotomy. We did not attempt to identify dogs that were treated by more conservative means, and the number of these cases at our institutions during the study period was not determined. In addition, some dogs may have died of hemorrhage, pneumothorax, or other sequelae of impalement before surgery. Despite these limitations, we conclude that dogs that undergo early controlled removal of impaling thoracic foreign bodies combined with surgical exploration of the thorax can have an excellent long-term prognosis.
Julia Zitz, DVM*
Elizabeth Rozanski, DVM, DACVIM (internal medicine), DACVECC
Dominique Penninck, DVM, DVSc, DACVR
John Berg, DVM, DACVS
Department of Clinical Sciences
Cummings School of Veterinary Medicine
Tufts University
North Grafton, MA 01536
*Dr. Zitz's current address is The Ohio State University, College of Veterinary Medicine, Columbus, OH 43210.
REFERENCES
1. Ludwig LL. Surgical emergencies of the respiratory system. Vet Clin North Am Small Anim Pract 2000; 30:531-553.
2. Powell LL, Rozanski EA, Tidwell AS, et al. A retrospective analysis of pulmonary contusion secondary to motor vehicular accidents in 143 dogs: 1994-1997. J Vet Emerg Crit Care 1999;9:127-136.
3. Spackman CJ, Caywood DD. Management of thoracic trauma and chest wall reconstruction. Vet Clin North Am Small Anim Pract 1987;17:431-447.
4. Campbell VL, King LG. Pulmonary function, ventilator management, and outcome of dogs with thoracic trauma and pulmonary contusions: 10 cases (1994-1998). J Am Vet Med Assoc 2000;217:1505-1509.
5. Fullington RJ, Otto CM. Characteristics and management of gunshot wounds in dogs and cats: 84 cases (1986-1995). J Am Vet Med Assoc 1997;210:658-662.
6. Cartwright AJ, Taams KO, Unsworth-White MJ, et al. Suicidal nonfatal impalement injury of the thorax. Ann Thorac Surg 2001;72:1364-1366.
7. Kelly IP, Attwood SE, Quilan W, et al. The management of impalement injury. Injury 1995;26:191-193.
8. Morgan T, Butler S, Schwab CW. Impalement injury: case study and management guidelines. Crit Care Nurse 1988;8:82-85.
9. Thomson BN, Knight SR. Bilateral thoracoabdominal impalement: avoiding pitfalls in the management of impalement injuries. J Trauma 2000;49:1135-1137.
10. Wick JM. Case report: survival of a type 1 transthoracic impalement. Int J Trauma Nurs 2001;7:88-92.
11. Galbis Caravajal JM, Mafe Madueno JJ, Baschwitz Gomez B, et al. Swordfish attack: an unusual cause of penetrating thoracic wound. Eur J Cardiothorac Surg 2002;21:926.
12. Watson JM, Goldstein LJ. Golf club shaft impalement: case report of a zone III neck injury. J Trauma 1996;41:1036-1038.
13. O'Brien J, Cohen M, Solit R, et al. Thoracoscopic drainage and decortication as definitive treatment for empyema thoracis following penetrating chest injury. J Trauma 1994;36:536-540.
14. Collins MB, Hodgson DR, Hutchins DR. Pleural effusion associated with acute and chronic pleuropneumonia and pleuritis secondary to thoracic wounds in horses: 43 cases (1982-1992). J Am Vet Med Assoc 1994;205:1753-1758.
15. Laverty S, Lavoie JP, Pascoe JR, et al. Penetrating wounds of the thorax in 15 horses. Equine Vet J 1996;28:220-224.
16. Pratschke KM, Kirby BM. High rise syndrome with impalement in three cats. J Small Anim Pract 2002;43:261-264.