N-methyl-D-aspartate (NMDA) receptor antagonist (Proceedings)
Pain transmission is complex and pain itself is difficult to manage in some cases. While a standardized approach to pain management forms a cornerstone from which to work, there are a variety of analgesic options available with which to provide multimodal analgesia; many veterinarians already have some of these modalities on hand.
Pain transmission is complex and pain itself is difficult to manage in some cases. While a standardized approach to pain management forms a cornerstone from which to work, there are a variety of analgesic options available with which to provide multimodal analgesia; many veterinarians already have some of these modalities on hand. Use of NMDA antagonists, such as ketamine and amantadine, may reduce the incidence of pain due to their actions as NMDA antagonists. This lecture we will review NMDA antagonists and their role as analgesics.
N-methyl-D-aspartate (NMDA) antagonists work by binding the phencyclidine site of the NMDA receptor, which will decrease the excitability of neurotransmitters (glutamate) at the dorsal horn of the spinal cord. These receptors are critical to processing and spinal modulation of pain, and so in this fashion, NMDA antagonists are unique in their ability to reduce pain transmission. Evidence would suggest that these receptors are not as important in acutely painful events as they are chronic responses to noxious stimuli (which would lead to central sensitization). Additionally, there is some evidence suggesting that NMDA antagonists also work at opioid receptors and sodium channels (amongst other receptors). The dosage required for the analgesic effect of ketamine (0.5 mg/kg intravenously, or less) is much lower than the induction and anesthetic dose of ketamine. In human patients, it appears S-ketamine may have more analgesic effects than the racemic mixture, but this has been difficult to prove in veterinary medicine. Often regarded as an adjunctive analgesic, the successful inclusion of ketamine as an analgesic drug is dependent on the type of pain a patient experiences as well as the other analgesic modalities the patient is receiving. Ketamine is often regarded as a more effective analgesic for somatic rather than visceral pain, and studies in verbal responders (i.e. humans) confirm this, especially pain of an inflammatory origin. In addition to its direct analgesic actions, there is also a reduction in the amount of opioids a patient requires for pain management when ketamine is incorporated into the appropriate analgesic plan. Hyperalgesia is reduced secondary to the use of ketamine.
Ketamine is not without adverse effects, however. Ketamine can induce the release of catecholamines, which will increase heart rate and blood pressure indirectly. This increase in the workload on the heart, in addition to increased oxygen consumption, is detrimental in animals that already have cardiovascular compromise. When catecholamines are not present in an animal that is sympathetically exhausted (for example, a septic patient) ketamine's direct effect of negative inotropy are more likely. Ketamine can increase cerebral metabolic oxygen consumption, as well as cerebral blood flow and cerebral spinal fluid pressure. All of these characteristics make ketamine a suboptimal choice for the patient who has sustained head trauma (e.g. a dog presenting after being hit by car). The increase in intracranial pressure secondary to the use of ketamine remains a controversial topic. A reduction in the dose necessary to produce analgesia (as opposed to the dosage necessary for induction of anesthesia) may attenuate some of these effects. In cats, ketamine is metabolized only to nor-ketamine, which is an active metabolite and therefore may produce undesirable side effects.
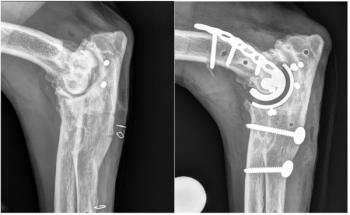
Ketamine is a reasonably priced drug to include in an analgesic regime. By way of example, for a 50kg dog presenting for a tibial plateau leveling osteotomy, when the estimating the cost of ketamine at $1.00/100mg, we would expect the following:
• Loading dose of 0.5mg/kg= 25 mg ($0.25)
• Constant rate infusion (CRI) of 10 mcg/kg/min for one hour= 30 mg ($0.30)
• Post-operative CRI of 10 mcg/kg/min for 6 hours= 180 mg ($1.80)
In total, it would cost $2.35 for including ketamine as an adjunctive analgesia for this patient. Additionally, ketamine may reduce the cost of other drugs by providing greater comfort and improved analgesia.
Practioners who do not have advanced equipment such as syringe pumps can still easily incorporate a CRI such as ketamine into their patients' plan. Simply calculate the amount of fluids that the patient would receive over the duration of the CRI administration, calculate the amount of ketamine necessary and combine the two. Using the above example, for the 50kg patient, practically would suggest a liter of fluid in the post-operative period. This volume could receive A. the patient's six-hour requirement (180mg) added to the liter, and the animal could receive this liter over 6 hours (receive 3.3ml/kg/hr, just over maintenance) or B. a fluid rate could be selected and the appropriate number of milligrams of ketamine added to the liter. In this later example, if 2.2 ml/kg/hr were selected, the total fluids required equals 660 mls. Therefore, to a one-liter bag, 273 mg of ketamine is added.
Various routes of administration will balance an analgesic plan. Traditionally, systemic administration of ketamine is most common, with even a single bolus (i.e. an induction dose) of ketamine assisting in reduction of noxious spinal cord traffic. As discussed previously, CRIs offer intraoperative and postoperative analgesia. Additionally, amantadine (an oral NMDA antagonist) is available in veterinary medicine, and has some usefulness long term in chronic pain associated with arthritis, in patients receiving non-steroidal anti-inflammatories (Lascelles et al. 2008).
Local, as opposed to systemic, administration of ketamine has been examined as well. This is likely due to ketamine blocking the sodium and potassium channels. Indeed, ketamine can produce an area of regional analgesia like local anesthetics (although local anesthetics are still far superior for this in that they are not controlled substances). There may be a role in intravenous regional analgesia for ketamine.
Ketamine administered via an epidural route has been examined. Ketamine is well absorbed from the epidural space, and has a rapid onset with a short but intense blockade lasting under an hour. However, the reduction of hyperalgesia present may last longer. Again, ketamine is unlikely to displace some of our traditionally administered epidural drugs, especially because it does not come in a preservative-free formulation, which is important when administering drugs epidurally.
Additionally there are some non-traditional routes by which ketamine might benefit a patient. Ketamine has provided cutaneous analgesia and been successfully used topically on oral or skin mucosa to reduce pain from radiation therapy. It has also been combined with electro-acupuncture to increase its efficacy.
Many veterinary practioners incorporate opioid constant rate infusions for intraoperative and post-operative pain reduction. A period of intense response to pain (hyperalgesia) after use of certain opioids is gaining recognition in the human medical field. This opioid induced hyperalgesia is reduced by fairly low doses of ketamine in human patients—as little as 0.25-0.33mg/kg of ketamine can prevent this phenomena from occurring.
With better routine care and the growth of small companion animal medicine, a growing reason to seek veterinary care is for chronic pain—pain from conditions such as cancer, degenerative joint disease, or neuropathies. There is little information to base the use of ketamine for chronic pain in veterinary medicine, but there is promise in the human medical field. The body of evidence does not suggest ketamine would be a first line therapy for such pain, but there is mild to moderate support of ketamine as an adjuvant pain therapeutic (Hocking and Cousins 2003).
NMDA antagonists, such as ketamine and amantadine, possess unique analgesic properties that make these drugs suitable for adjunctive therapeutics. As veterinarians expand their analgesic options, the incorporation of these drugs will help build upon a solid foundation of traditional analgesic options, such as opioids and non-steroidal anti-inflammatory drugs. Given the complexity of pain, this advancement will improve care for many patients.
References
Hocking, G. & M. J. Cousins (2003) Ketamine in chronic pain management: an evidence-based review. Anesth Analg, 97, 1730-9.
Lascelles, B. D., J. S. Gaynor, E. S. Smith, S. C. Roe, D. Marcellin-Little, G. Davidson, E. Boland & J. Carr (2008) Amantadine in a multimodal analgesic regimen for alleviation of refractory osteoarthritis pain in dogs. J Vet Intern Med, 22, 53-9.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.






