Respiratory monitoring (Proceedings)
Delivery of adequate oxygen to tissues and cells is the overall goal of the cardiovascular system. Oxygenation is dependant on cardiac output (heart rate and stroke volume), arterial blood pressure, circulating blood volume, and pulmonary function. Critically ill patients often have impairments to one or several of these processes resulting in hypoxemia, ischemia and cell death. Restoring these functions to normal insures oxygenation.
Delivery of adequate oxygen to tissues and cells is the overall goal of the cardiovascular system. Oxygenation is dependant on cardiac output (heart rate and stroke volume), arterial blood pressure, circulating blood volume, and pulmonary function. Critically ill patients often have impairments to one or several of these processes resulting in hypoxemia, ischemia and cell death. Restoring these functions to normal insures oxygenation.
Pulse oximetry
A pulse oximeter provides immediate and continual estimations of oxyhemoglobin saturation (SpO2) by transmission of varying light through the skin. Light absorption during arterial pulses is differentiated from absorption due to bone and venous blood.
Oxygen saturation is not the same as arterial pO2 (as measured on a blood gas) but is related to the extent that normal SpO2 is thought to imply normal pO2 and decreased SpO2 correlates with a low pO2. Specifically, due to the oxygen dissociation curve; at arterial pO2 of 60-70 mm Hg, hemoglobin is expected be fully saturated although normal pO2 is>85 mm Hg.
SpO2 measurement gives important information about delivery of oxygen to tissue and may be used to assess the effectiveness of supplemental oxygen therapy. Oximetry is also used as an indicator for peripheral perfusion in the anesthetized patient as well as to monitor patients who are being mechanically ventilated. The limitations of pulse oximetry include inability to obtain readings or inaccurate readings in patients who have serious perfusion problems, severe hypothermia or gross anemia. Unfortunately these are often the patients who most require oxygenation assessments. Because of these limitations arterial blood gas measurement remains essential in critical patients although frequency of sampling can be greatly reduced by pulse oximetry.
Pulse oximetry has the added advantage of being non-invasive and requires less expensive equipment than blood gas analysis.
Capnography
Expired or end tidal CO2 can be continuously monitored in the intubated patient by attaching a sensor device to the endotracheal tube. End tidal CO2 correlates well with CO2 measured on a blood gas (PaCO2) and provides an accurate non-invasive measure of alveolar ventilation. Capnography is useful for assessing and regulating breathing rate particularly in the hypoventilating patient as is extremely valuable in weaning from mechanical ventilation.
Combined, pulse oximetry and capnography give the most complete picture of respiratory function available by non-invasive means. They should not be thought of as substitute for arterial blood gas analyses in patients with respiratory disorders, however their usefulness for continual monitoring and detection of changes in patient status is unquestionable.
Arterial blood gas analysis
Blood gas analysis provides information about respiratory function and acid/base status. This information is vital in determining and monitoring treatment of patients with primary or secondary respiratory disease and/or metabolic disturbances Acid/base disturbances can severely impede successful treatment of illness and can be, in and of themselves, life threatening. For example, "sick" keto-acidotic diabetics require careful monitoring and treatment to restore normal blood pH. Previously, the costly , large, high maintenance analyzers required to perform blood gas measurement have prohibited use at most veterinary clinics. The advent of relatively inexpensive, hand-held, user friendly analyzers such as the i-STAT® has allowed for any veterinary practice to perform blood gas analyses.
Blood gas (BG) can be assessed on arterial (ABG) or venous (VBG) samples although oxygenation assessment is made on arterial blood only. Results are dependent on the specific patient temperature and hematocrit. Both of these parameters are entered into the blood gas analyzer prior to evaluation. Understanding the basic principles of blood gas analysis allows simple, rapid interpretation of results. The basic components of BG analysis include:
• oxygen (PaO2)
• carbon dioxide (PaCO2)
• blood pH
• bicarbonate (HCO3)
• base excess (BE-B)
Together, these parameters convey an accurate and complete picture of respiratory function and metabolic state.

5 step blood gas interpretation
1. Evaluate the PaO2 and determine if the patient is hypoxemic (needs oxygen).
2. Evaluate the pH and determine if the patient is normal, acidotic or alkalotic.
3. Evaluate the PaCO2 and determine if it supports the pH findings. (if YES then the condition is primarily respiratory, if NO the condition is not primarily respiratory).
4. Evaluate the HCO3 and determine if it supports the pH findings. (if YES then the condition is primarily metabolic, if NO the condition is not primarily metabolic).
5. Evaluate the parameter NOT responsible for abnormal condition to assess for compensation.
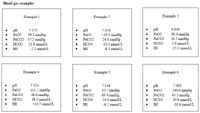
Blood gas examples
A guide for assessing respiratory emergencies
November 15th 2024Mariana Pardo, BVSc, MV, DACVECC, provided an overview on breathing patterns, respiratory sounds, lung auscultation; and what these different sounds, patterns, and signs may mean—and more—in her lecture at the 2024 NY Vet Show
Read More