Solutions for challenging canine demodicosis cases
Demodicosis is a common skin condition in dogs. Dogs have three recognized species of Demodex mites.
Demodicosis is a common skin condition in dogs. Dogs have three recognized species of Demodex mites. Clinically, the most common mite is Demodex canis (photo 1). This mite is limited to the hair follicle and sometimes the sebaceous gland. Dogs can also develop demodicosis due to the large-bodied Demodex mite or D. injai (photo 2). This mite usually causes a dorsal, seborrheic dermatitis. The third species of canine Demodex is the short-bodied D. cornei. Its clinical signs are similar to those of D. canis.

Photo 1. An adult Demodex canis mite (40X). (PHOTOS: COURTESY OF KATHY TATER, DVM)
Treating dogs with demodicosis can be challenging for both the veterinarian and the client. This article discusses some of the common reasons why demodicosis can be so challenging and offers solutions for how to meet the challenges head-on.

Photo 2. An adult Demodex injai mite (40X).
CHALLENGE: If demodicosis isn't on your radar, you may forget to check for demodicosis and miss the diagnosis.
SOLUTION: Know the common clinical signs of canine demodicosis so you never miss a case!
Canine demodicosis can be diagnosed with simple equipment. Most cases of demodicosis can be diagnosed with hair plucks or skin scrapes using mineral oil, a scalpel blade, a hemostat, glass slides, and a light microscope. Skin biopsies and histopathology are sometimes necessary to diagnose demodicosis, but this occurs more commonly in dogs with thickened or scarred skin.
Since everyone has the tools to diagnose demodicosis, why do veterinarians sometimes miss demodicosis cases? On rare occasions, the veterinarian's scraping or plucking technique is at fault. It is important to sample multiple lesion sites, scrape until capillary bleeding is evident, and obtain hair plucks in addition to skin scrapes, especially when the sites are already hemorrhagic and difficult to scrape. More commonly, I find that a veterinarian misses demodicosis cases because he or she didn't have demodicosis on the differential list.

Photo 3. Follicular casting on the muzzle of a dog with demodicosis.
Remember that canine demodicosis can present with a variety of clinical signs. The primary lesions of canine demodicosis include spontaneous alopecia, scaling, follicular casts [keratosebaceous material adhered to the hair shaft (photo 3 and photo 4)], papules, and comedones. Comedones are sometimes misidentified by veterinarians as non-specific, post-inflammatory hyperpigmentation unless a thorough dermatologic examination under good lighting is performed (photo 5). Other lesions of demodicosis include crusts, erythema, hyperpigmentation, and lichenification. Demodicosis can occur with or without pruritus. It is usually more pruritic if concurrent secondary infections are present. Demodicosis due to the short-bodied form of the mite (D. cornei) is often pruritic.

Photo 4. Follicular casts after the hairs have been plucked from the skin.
If you think demodicosis is a differential diagnosis for a particular patient, check for the mite. It is rarely wrong to perform skin scrapes and hair plucks in a patient presenting with dermatologic lesions because these tests are inexpensive and not invasive, and missing demodicosis could result in other, more expensive diagnostic tests.
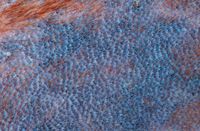
Photo 5. Comedones on a dog with demodicosis.
CHALLENGE: If the patient's other health problems aren't identified and treated, cases of demodicosis may not improve, or may improve and then reoccur.
SOLUTION: Use the patient history, physical exam, clinical signs, and diagnostic testing results to identify any other health problems.
Demodex mites can lead to secondary pyoderma. Superficial staphylococcal pyoderma is treated empirically by using a beta-lactamase-stable antibiotic for a minimum of four weeks. In dogs with unresponsive superficial pyoderma or deep pyoderma, or when rod-shaped bacteria are identified on cytologic examination, a bacterial culture and antimicrobial sensitivity testing is strongly recommended to help select an antibiotic. Continue antibiotic therapy until the pyoderma is clinically and cytologically resolved. Deep pyodermas may need several weeks of antibiotic therapy. Topical therapy with a shampoo containing an antibacterial active ingredient (benzoyl peroxide, chlorhexidine, or ethyl lactate) can also help treat the pyoderma.
Cases of adult-onset demodicosis usually have an underlying cause. Ask clients about any medications that the pet is receiving, as certain medications, such as glucocorticoids, can contribute to the development of demodicosis. I question clients about their use of topical and over-the-counter medications. I've found that some clients don't consider these "medications" even though topical and over-the-counter glucocorticoids can also contribute to the development of demodicosis, especially if applied frequently. Adult-onset demodicosis can be a sign of an underlying systemic condition such as Cushing's disease, hypothyroidism, diabetes mellitus, or heartworm disease. A complete blood count, serum chemistry profile, urinalysis, and heartworm test are useful to explore predisposing conditions. With the history and any other findings from the physical examination, this minimum database may lead to other diagnostic testing such as hormonal assays and stimulation studies. In cases with an underlying systemic condition, resolution of the demodicosis may not occur until the pet's other health problems are well controlled.
CHALLENGE: There are several options for treating demodicosis. Which one should you choose?
SOLUTION: Educate yourself and your client on the treatment options for demodicosis so that you select the appropriate therapy for each patient.
Most of the various treatments for canine demodicosis fall into two categories of medication. Amitraz is a monoamine oxidase inhibitor (MAOI), prostaglandin synthesis inhibitor, and an alpha2-adrenergic agonist. It is available in the United States as a liquid concentrate (Mitaban—Pfizer Animal Health) to be used as diluted dip and as a spot-on with metaflumizone (ProMeris for dogs, Fort Dodge Animal Health). Ivermectin, milbemycin oxime, and moxidectin are all macrocyclic lactones.
When dosed appropriately, both amitraz and the macrocyclic lactones are effective therapies for demodicosis. Each therapy has its benefits and drawbacks. It's important to evaluate each dog with demodicosis on a case-by-case basis and educate clients about the different miticidal options.
Amitraz is the only active ingredient approved by the U.S. government for treatment of Demodex mites. It is an especially important miticidal option in dogs that are sensitive to macrocyclic lactones. Drawbacks of amitraz dips include the need to apply the treatment topically and potential side effects such as lethargy, hypothermia, bradycardia, and hyperglycemia. The spot-on formulation of amitraz recently became approved for the treatment of demodicosis and is more convenient to apply; however, it potentially has the same side effects of amitraz dip. More studies are currently being performed on this product that will give us more information on how to use it for the treatment of demodicosis.
The two most commonly used macrocyclic lactones for the treatment of demodicosis are milbemycin oxime and ivermectin. Both are given orally once daily at 1.5 to 2 μg/kg for milbemycin oxime and 300 to 600 μg/kg for ivermectin. Milbemycin oxime is more expensive than ivermectin, but for some clients, its tablet form may be easier to administer than liquid ivermectin. Dogs should test negative for heartworm disease before starting macrocyclic lactone therapy. Side effects can include lethargy, mydriasis, muscle tremors, ataxia, blindness, and seizures. When using macrocyclic lactones for generalized demodicosis, clients should understand their extra-label use and potential for side effects. To identify ivermectin-sensitve dogs, a test to screen dogs for a genetic mutation that causes ivermectin sensitivity is available at the Washington State University Veterinary Clinical Pharmacology Laboratory (www.vetmed.wsu.edu/vcpl). I also recommend starting dogs on a low dose (50 μg/kg) of ivermectin once a day and incrementally increasing the dose by 50 μg/kg during the first days of treatment until the target dose is achieved.
In my experience, one of the most common reasons for a seemingly resistant case of demodicosis is the premature discontinuation of treatment. Any miticidal treatment for canine demodicosis should continue until two consecutive negative skin scrapings are obtained two to four weeks apart. Client compliance can be an issue because cases of canine demodicosis may look clinically normal to the client before they are truly mite-free, tempting clients to stop the use of the miticide early. A client handout on the need to continue the miticide as directed can be very helpful.
A patient with demodicosis may respond better to one miticide than another. A good rule of thumb is to give each treatment plan several weeks to demonstrate an effect. If the number of eggs, immature mites, or total mites do not decrease significantly in four to eight weeks, consider altering the dose of the the given treatment before switching active ingredients.