Study investigates GME therapy choices
The definitive diagnosis of GME rests with CNS histopathologic sampling.
Cyclosporine has been employed in veterinary medicine in patients with keratoconjunctivitis sicca, renal transplants, immune-mediated hemolytic anemia, immune-mediated thrombocytopenia, perianal fistulas, and more recently, for pruritic dermatoses. This review discusses it's recently published use in the treatment of granulomatous meningoencephalitis (GME).
Drs. Adamo and O' Brien (in "Use of cyclosporine to treat granulomatous meningoecephalitis in three dogs", JAVMA Vol 225, No. 8, pgs 1211-1216) reported two dogs with imaging and cerebrospinal fluid (CSF) analysis evidence of GME and one dog with a histopathological diagnosis of GME where treatment included cyclosporine. Two of the three cases had favorable clinical responses to therapy. They cite a report by Dr. Kipar et al. in the journal Veterinary Pathology (1998; 35: 45-52) that suggests that GME is an immune-mediated disease of the central nervous system (thus the rationale for employing cyclosporine in this disease). These case reports are of major interest to veterinarians who are searching for more-effective treatments for this serious and often fatal inflammatory neurologic disease.
The definitive diagnosis of GME rests with central nervous system (CNS) histopathologic sampling. The working clinical diagnosis often results from typical CSF cytology, negative findings on cultures and infectious disease serology/PCR determinations, and CNS imaging by magnetic resonance (MRI) or computed tomography (CT), which support the diagnosis of GME. Figure 1 represents the CSF cytology in a canine with GME.
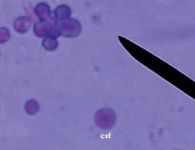
Figure 1 shows the CSF cytology in a canine with GME. Cyclosporine's method of action may be related to inhibition of cytokines that modulate macrophage and monocyte activation.
Cyclosporine's method of action may be related to inhibition of cytokines that modulate macrophage and monocyte activation. Its traditional use has been in suppression of organ-transplant rejection. The authors employed cyclosporine dosages of 3-10 mg/kg BID po in these GME cases, with and without concurrent corticosteroid therapy. It should be noted that cyclosporine has variable pharmacokinetics in our patients. Trough levels of the drug should be monitored in all patients receiving immunosuppressive dosages, and the patient should not be switched back and forth between different brand names of the drug. Cyclosporine trough levels may be checked as soon as 24-48 hours after beginning therapy. Individual laboratory reference ranges should be noted. Periodic CBC and biochemical profile monitering is also recommended.
Concurrent ketoconazole therapy will result in elevated cyclosporine blood levels in the canine. This combination has in fact been suggested by other authors in an attempt to reduce the cost of therapy (Daigle JC, "More economical use of cyclosporine through combination drug therapy". J Am Anim Hosp Assoc 2002; 38: 205-208). The clinician should also be aware that macrolide antibiotics, androgens and metoclopramide might increase cyclosporine levels. Conversely, omeprazole, phenobarbitol and calcium channel blockers may reduce blood levels of cyclosporine.
If the patient responds well to therapy with cyclosporine alone, or in combination with corticosteroids, gradually tapering both immunosuppresives is indicated, preferably with close monitoring of physical examinations, neurologic status, and CSF analysis.
Periodic urine analyses and cultures by cystocentesis should be performed to detect hidden urinary tract infections. Follow-up CNS imaging is usually beneficial in case management when available and permitted by the client.







