Veterinary emergency management of equine burn victims
As veterinarian and first responder to a barn fire, would you know how to treat a burn-compromised horse?
More than 1,000 structure fires strike barns and stables annually (data reported from 2002 to 2005), leaving their equine inhabitants vulnerable to smoke inhalation, severe burns and even death.1 See Table 1 for common causes of barn and stable fires.2
Potential for injury
"There are two major concerns of damage to the burn-compromised horse: thermal injury to the epithelial surfaces—skin, eyes, cornea, including the entire airway—and smoke inhalation damage to the lungs," says Ray Sweeney, VMD, DACVIM, of the Department of Clinical Studies at New Bolton Center, University of Pennsylvania School of Veterinary Medicine.

Table 1: Common causes of barn and stable fires
"These horses can develop complications such as laminitis," says Michelle Harris, VMD, DACVIM, Department of Clinical Studies, New Bolton Center, University of Pennsylvania School of Veterinary Medicine. "Depending on where the burns are, it may be very difficult to even treat them due to loss of venous access."
"More life-threatening to the burn-compromised horse, besides skin thermal injury, is probably the damage to the airway and the lungs, especially the smoke inhalation insult, which can include carbon monoxide and other toxins," says Sweeney. "Thermal injury can also damage the lining of the respiratory tract from the tip of the nose all the way down to the alveoli. You can also get thermal damage to the upper airway and burn damage to the inside of the nasal passages and the throat.
"With tissue death, the airway can become swollen, which may cause partial obstruction of the airway," continues Sweeney. "You can also have damage to the lower airway to the alveoli that can incite an inflammatory cascade and cause protein to exude into the lungs, which can cause a respiratory distress-type syndrome."
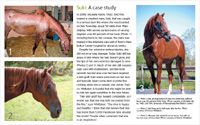
Suki: A case study
According to Emma Adam, BVetMed, DACVIM, DACVS, of Gluck Equine Research Center at the University of Kentucky, the thermal insult also causes microvascular damage and direct tissue coagulation, which can lead to systemic shock.3
"Systemic shock can lead to triggering of the inflammatory and coagulation cascades and decreased cardiac output," says Adam. "Microvascular damage—both direct and inflammatory cytokines—leads to an increased capillary pressure, with leaky capillaries followed by the formation of edema. As shock progresses, tissue perfusion is further compromised, vascular permeability increases and protein leaks into interstitial spaces, furthering circulatory collapse and edema formation."3
Treatment basics
The following steps can help you protect and stabilize your patients.
1. Contain the horses
If you are the first responder to a barn fire, it's important to know that horses may instinctively run back into a burning barn, returning to their traditional place of safety, according to Harris. "Once you get them out of the barn, put them in a safe place far away from the fire so that they are contained and can't attempt to run back in," Harris says.
2. Cool the tissue
Gently rinse burned skin with cool water, says Harris. Using ice or very cold water may further damage already compromised tissue. Keep in mind that the extent of burn injury to the lungs or skin is usually not obvious for several days.
3. Introduce fluids
"Depending on the extent of injury, these horses can require intensive care, including intravenous fluids, as they can have extreme fluid shifts within their body," says Harris. "Keeping their cardiovascular system stable is critical."
The fluid loss from the damaged skin and internal lining of the airway may cause the horse to lose protein and experience cardiovascular shock. "Intravenous fluids to stabilize blood pressure and volume is one of the first treatment regimens," Sweeney says. Intravenous fluids typically include balanced electrolytes, hypertonic saline solution, plasma extenders (e.g., hetastarch) or even plasma itself—all in an attempt to maintain an animal's fluid volume to support tissue perfusion.
4. Administer oxygen
Administering oxygen is the next important step, "particularly if the lungs are damaged and may have reduced ability to exchange oxygen," says Sweeney.
Hyperbaric oxygen therapy has been reported to benefit human patients with smoke inhalation. Although its use has been reported less frequently in lung-compromised horses, it has been used to assist healing of burn-compromised skin graft wounds in horses (see "A closer look at hyperbaric therapy"). Sites with hyperbaric oxygen units for horses are limited, but among them are the University of Tennessee Veterinary Medical Center and Hagyard Equine Medical Institute in Lexington, Ky.

A closer look at hyperbaric therapy
5. Mitigate the inflammatory response
"While IV fluids and oxygen are the mainstays of the first response, caregivers can then begin to abrogate the body's severe inflammatory response using vitamin E and nonsteroidal anti-inflammatory drugs, among others," says Sweeney. Dimethyl sulfoxide (DMSO) is often used because of its oxygen radical scavenging ability, and pentoxifylline is a commonly used anti-inflammatory drug.
Reactive oxygen species, peroxides and oxygen free radicals mediate a lot of the inflammation in these patients. "That is the reason for the supplemental vitamin E, which may help as an antioxidant," Sweeney says. A study in sheep found that pretreatment with vitamin E (1,000 IU alpha-tocopherol) ameliorated the acute lung injury caused by burn and smoke inhalation exposure.4
6. Manage the pain and prevent infection
Treating the dermal burns is vital, as extensive damage can be life-threatening. "Burns are very painful, so doctors must provide medication for analgesia," says Sweeney. "One might have to add an opioid or ketamine for pain control."
Burned skin will eventually die and form what is called eschar, or dead tissue on the surface of the wound. "In many instances, this eschar should be left in place until it comes loose on its own, as it can act as a protective coating over what is hopefully new skin growing underneath," says Harris.
Harris says her team typically treats skin damage with generous amounts of silver sulfadiazine, a cream made specifically for human burn patients. The cream kills a wide variety of bacteria and fungi and keeps the damaged skin moist.
When it comes to preventing infection, there is debate whether doctors should administer antibiotics as a preventive. "It is probably indicated in horses, as horses—unlike humans—live in a barn with greater potential for infection," Sweeney says.
7. Think long term
Growing new skin and healing burns requires a huge amount of calories, so proper feeding is critical. In addition to pain and inflammation control, it is important to maintain a high plane of nutrition for these equine burn victims. "If they're not in pain, they will keep eating, which is extremely helpful during the healing process," Harris says.
In the short term it is important to control the pain and potential skin infection. In the long term, that skin is going to slough, so there may be need for surgical débridement and skin grafting.
Ed Kane, PhD, is a researcher and consultant in animal nutrition. He is an author and editor on nutrition, physiology and veterinary medicine with a background in horses, pets and livestock. Kane is based in Seattle.
References
1. Flynn J. U.S. structure fires in barns. Quincy, Mass: National Fire Protection Association, 2008. Available at http://www.arfireprevention.org/pdf/Fire_Reports/U.S_Structure_Fires_in_Barns.pdf
2. Barn fire safety: fact sheet for horse farms. Lexington, Ky: Equine Risk Management Group LLC, 2011. Available at http://www.horse-safety.com/pdfs/DISASTERS_2011_ERMG_BARN_FIRE_SAFETY.pdf
3. Adam EN. How to cope with barn fires, in Proceedings. Am Assoc Equine Pract 2012;58:189.
4. Morita N, Shimoda K, Traber MG, et al. Vitamin E attenuates acute lung injury in sheep with burn and smoke inhalation injury. Redox Rep 2006;11(2):61-70.