Why, when and how to perform percutaneous renal biopsies
Can you assess when this diagnostic procedure is best indicated?
A colleague in private practice asked my opinion about the likely benefit of obtaining an ultrasound-guided percutaneous needle biopsy of the kidney of a 15-year-old spayed female domestic shorthaired cat. He said evaluation of a serum chemistry profile, hemogram and urinalysis revealed findings (isosthenuria, intrarenal azotemia, hypoproliferative anemia, acidemia, hyperphosphatemia) consistent with idiopathic chronic renal failure (CRF). No evidence of bacterial urinary tract infection was noted. The cat's systolic blood pressure was increased. The cat's owners requested the veterinarian pursue additional diagnostics, especially if they could help in devising a treatment for the renal failure and prolong the cat's life.
Ultrasonographic evaluation of the cat's kidneys by a board-certified radiologist revealed that both kidneys were reduced in size. Uroliths were not observed. An advantage of ultrasonography is the biopsy needle can be guided into portions of the kidney so as to minimize the risk for damage to large renal vessels and the renal pelvis. In addition, the kidney can be scanned for evidence of significant post-biopsy hemorrhage.
The consulting radiologist, who had considerable experience with ultrasound-guided percutaneous needle biopsies of the kidney, was willing to perform this procedure if requested to do so. Are the probable benefits associated with needle biopsy of this cat's kidneys likely to outweigh the risks associated with the procedure?

Table 1
Why and when should percutaneous renal biopsies be performed?
Information obtained by renal biopsy may confirm, support or eliminate diagnostic probabilities formulated on the basis of the history, physical examination, laboratory data and radiographic or ultrasonographic evaluation. The results of biopsy may be very helpful in formulating prognoses and treatment plans for some diseases, including protein-losing glomerulopathy and acute or subacute renal failure (Table 1; Figure 1).
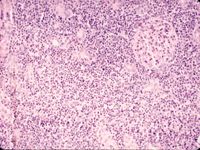
Figure 1: A photomicrograph of a renal cortex section of a 15-year-old neutered male domestic shorthaired cat's right kidney. The cat developed signs of renal failure eight to 10 days ago. Notice the extensive accumulations of neutrophils in the tubulointerstitium. These biopsy results indicate this suppurative nephritis potentially is reversible.
In cases in which renal biopsy permits establishment of a specific diagnosis, knowledge of the etiology facilitates formulation of a specific therapy designed to eliminate or control the underlying cause of renal disease. Although the specific therapy may not alter existing lesions, it may prevent further damage to nephrons and adjacent structures. In situations in which the light microscopic, immunofluorescence or electron microscopic changes do not indicate a specific diagnosis, the character and distribution of lesions may allow one to determine whether the disease process is likely to undergo partial or complete resolution, remain static or become progressive and irreversible. Such information may be especially helpful when evaluating patients with acute renal failure associated with declining renal function and/or oliguria despite appropriate specific and supportive therapy. In some patients, properly performed serial biopsies of the kidney also may be used to monitor therapeutic efficacy, morphologic resolution of the disease or progression of renal disease.
In the current state of knowledge, however, biopsies are usually of little value to patients with CRF associated with kidneys of reduced size (Figure 2). Once the disease process has progressed to this state of chronicity, it typically follows an irreversible and progressive course, ultimately leading to uremia and death. In this situation, biopsy results are unlikely to provide information that would alter the long-term prognosis or the therapeutic plan. Results of a renal biopsy would not alter treatment, which consists primarily of supportive therapy designed to modify or eliminate abnormalities that occur secondary to altered renal function. Irrespective of the underlying cause, supportive therapy of CRF is usually formulated to minimize retention of metabolic wastes and alterations (deficits and excesses) in fluid, electrolyte, acid-base, endocrine and nutrient balance.
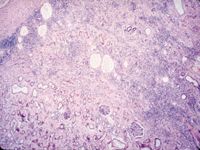
Figure 2: A photomicrograph of a section of a renal biopsy obtained from a 14-year-old spayed female Siamese cat with renal failure. This cat had severe hypoproliferative anemia and bilateral reduction in renal size-changes consistent with CRF. In this case, since the clinical presentation suggested that a specific finding on biopsy would not alter therapy, nor provide prognostic information, the procedure was not justified.
What are some potential risks for renal biopsy associated with CRF?
Biopsy complications usually occur in inverse proportion to the experience of the individual performing this procedure. For veterinarians who have not been formally trained in a specialty requiring these types of techniques, some extensive practice is needed. Before attempting renal biopsy in a patient, individuals unfamiliar with the use of biopsy needles and techniques should gain experience by obtaining samples from animals at the time of euthanasia or from cadavers. Familiarity with punch biopsy needles may be gained initially by substituting apples or pears for kidneys. Careful attention to procedural detail is essential if adequate biopsy samples are to be consistently obtained with minimal risk to patients.

Figure 3: A photograph illustrating infarction of the caudal pole of a dog's right kidney. A percutaneous needle biopsy containing cortex and medulla was obtained from this kidney one week previously.
Even when ultrasound-guided biopsies are performed by experienced individuals, they still can cause further renal damage. In addition to mechanical trauma directly caused by advancing the needle through the renal parenchyma, varying degrees of ischemia and infarction also occur secondary to disruption of blood perfusion through vessels damaged by biopsy needles. Because renal arteries are end-arteries without collateral blood supply, sudden occlusion or transection of any portion of the arterial tree will be followed by ischemia and infarction of parenchyma distal to the sites deprived of perfusion. Therefore, the overall severity of damage caused by needle biopsy of the kidney depends primarily on the size and number of renal vessels through which blood flow has been compromised. This mechanism (ischemia and infarction) may result in a significantly greater quantity of damage to nephrons than mechanical damage along the biopsy tract directly caused by the needle.

Figure 4: Results of high-resolution angiography of the kidney of a normal young adult mixed-breed dog illustrating the arborizing architecture of interlobar, arcuate and interlobular arteries. Confining renal biopsy tracts to the renal cortex will minimize damage to larger vessels. (Angiogram courtesy of Dr. James W. Wilson.)
Damage to larger renal arteries, such as arcuate arteries located at the corticomedullary junction, may result in wedge-shaped infarcts (which, in three dimensions, are cone-shaped; Figure 3). Because the kidneys of most cats are smaller than the kidneys of most dogs, the risk of damaging larger renal arteries is greater in cats when standard punch biopsy needles are used. Likewise, biopsy samples that contain tissue from the renal medulla are more likely to be associated with damage to larger vessels than samples obtained from the renal cortex (Figures 4 and 5). For this reason, it is usually best to direct the long axis of the biopsy needle so the biopsy tract is confined to the renal cortex (Figure 6). Even in those instances, however, linear infarcts are likely to occur (Figures 7 and 8).
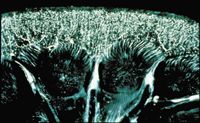
Figure 5: Results of microangiography of a 1.5-mm slice of kidney obtained from a normal adult mixed-breed dog illustrating afferent arterioles, glomeruli and some peritubular vessels. Note that larger arteries are not present in the renal cortex. (Angiogram courtesy of Dr. James W. Wilson.)
Renal size should be considered when evaluating the risks of needle biopsy of the kidney. Reduction in the thickness of the renal cortex as a consequence of chronic progressive renal disease increases the likelihood of needle damage to larger intrarenal vessels such as the arcuate arteries.

Figure 6: A schematic illustration of a biopsy of the renal cortex using a Tru-Cut biopsy needle. Note that the needle has not traversed the corticomedullary junction.
Because excessive hemorrhage is a potentially serious complication of this procedure, patients with a hemorrhagic tendency should not be undergo a biopsy unless abnormalities in hemostasis can first be adequately controlled. Likewise, hypertension has been associated with an increased incidence of hemorrhage and arteriovenous fistulas in humans after renal biopsy. Therefore, hypertension should be controlled before needle biopsy of the kidney.
How should renal biopsy samples be handled?
If a decision to perform a renal biopsy is deemed to be in the patient's best interest, before performing the procedure, contact a laboratory familiar with evaluation of kidney biopsy samples, and ask for specific directions on how to process the sample. For example, request information about how to process samples for standard light, immunofluorescent and electron microscopy, as well as immunohistochemical techniques.

Figure 7: A photograph illustrating a linear infarct in the renal cortex of a dog's right kidney. A needle biopsy sample taken from this region one week previously contained only tissue from the renal cortex.
Now what's your opinion?
Key point: Since renal biopsy procedures are associated with significant risks, they should not be performed unless the associated benefits are likely to outweigh those risks for the patient's welfare. After considering this information, how would you respond to the question: Are the probable benefits associated with needle biopsy of this cat's kidney likely to outweigh the risks associated with this procedure?

Figure 8: A photograph illustrating a large, healed infarct in the caudal pole of the right kidney of an adult female miniature schnauzer. A Tru-Cut biopsy needle was used to obtain a sample containing cortex and medulla from this region six months previously.
In formulating your answer, consider the following:
1. What diagnostic, prognostic or therapeutic goals are likely to be achieved by evaluation of kidney biopsy samples?
2. Will the benefits associated with the technique of ultrasound-guided kidney biopsy be sufficient to justify the associated risks and costs?
Dr. Osborne, a diplomate of the American College of Veterinary Internal Medicine, is professor of medicine in the Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Minnesota.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.