Advanced imaging modalities in veterinary medicine
CT and MRI continue to gain traction as they become more widely available and less costly. Their diagnostic superiority over radiography will improve the treatment of some common diseases in small animal patients.
Radiography has long been the staple imaging modality in veterinary medicine. Although CT and magnetic resonance imaging (MRI) have been available in large specialty and teaching hospitals for decades, the decreasing cost of ownership has recently made them more readily available in smaller settings. In addition, improved technology, with a decreased need for radiation shielding, has allowed for a small number of mobile CT practices to spring up throughout the country. Although radiography will always have a place in veterinary medicine, increased access to advanced imaging modalities allows for better diagnosis and treatment of common diseases. In particular, many diseases of the head, brain, spine, vasculature, and musculoskeletal system are more readily diagnosed with these advanced modalities.
Head
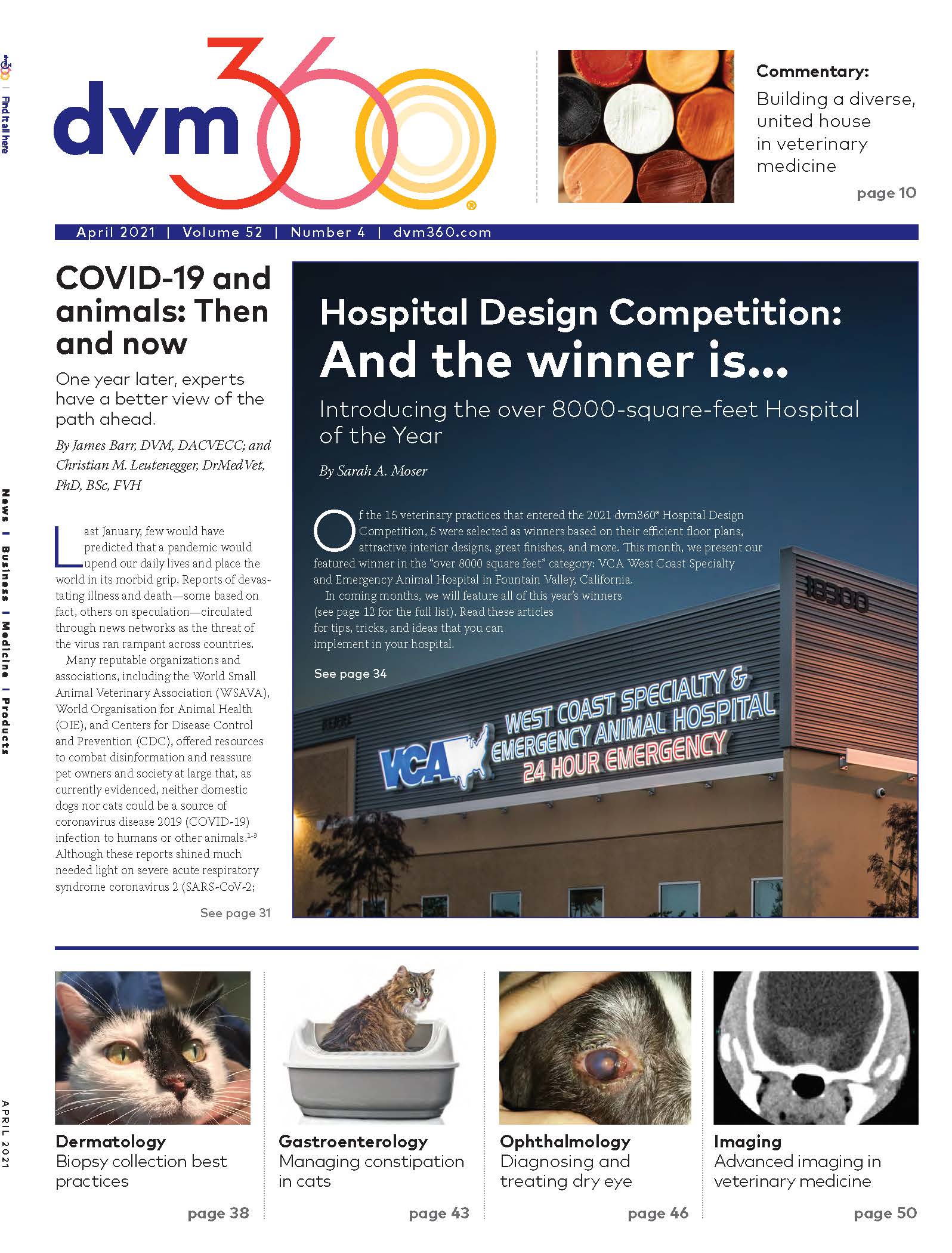
Compact anatomy and superimposition make CT the ideal modality for imaging of the head. One of the most common clinical complaints seen by our internal medicine service is chronic nasal discharge in geriatric patients. Skull radiographs are limited in their ability to contribute significant information toward a diagnosis, are technically difficult, and require heavy sedation or anesthesia for well-positioned images. Although radiographs can help the clinician assess for increased or decreased opacity within the nasal cavity, as well as regional osteolysis, subtle disease is often missed. Important aspects of disease such as cribriform plate lysis, nasopharyngeal polyps, or intranasal foreign bodies can be difficult to diagnose with radiography. CT is not only useful for assessing the nasal cavity in these patients but provides additional information on disease of the regional lymph nodes (Figures 1 and 2). In these cases, CT is best used as a complimentary modality to rhinoscopy with biopsy sampling, with both performed during the same anesthetic event.
Figure 1. Although no definitive diagnosis was made, CT reveals a very large, aggressive mass originating from this cat’s left ear canal. The mass invades the calvarium and regional soft tissues and is a presumed neoplasm.
Similarly, in the case of head trauma, subtle and nondisplaced fractures can be missed due to the summation of multiple bones. In addition, appropriate skull radiographs require heavy sedation or anesthesia with numerous oblique views obtained. Although CT also requires sedation, images are captured quickly in all planes, with the ability to reconstruct images into oblique planes, as well as 3-dimensional volumes.
Figure 2. On CT, a large nasal adenocarcinoma is noted within the right nasal cavity, causing both paranasal bone lysis and subtle cribriform plate lysis.
Brain
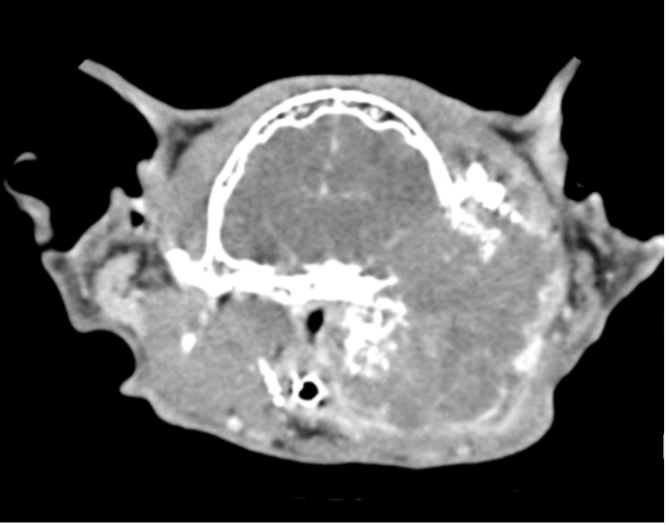
Both MRI and CT can be used in patients in whom clinical signs refer to the brain. Radiography has very limited use in these cases, with findings such as hyperostosis of the calvarium reported in cases of meningiomas.1 MRI is traditionally more expensive and less readily available than CT, but its superior soft tissue contrast and detail make it the ideal modality for most neurologic patients.
CT is particularly useful in trauma patients, as the quick image acquisition can minimize sedation. CT can be used to easily identify skull fractures, evaluate for cerebellar herniation, and assess for intracranial hemorrhage (Figure 3). When the cost of MRI is prohibitive, CT can also be used to assess for brain neoplasms, especially those that typically contrast enhance, such as meningiomas.
Figure 3.Severe congenital hydrocephalus in a juvenile Chihuahua with a history of seizures. Although MRI is often used for brain disease, this CT accurately depicts the degree of ventricular dilation.

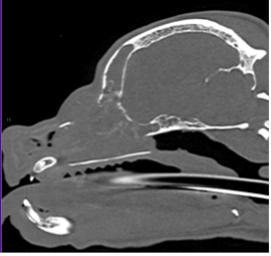
MRI offers superiority in the diagnosis of brain neoplasms, inflammatory disease, and ischemic infarctions. Its main drawbacks are cost and the lack of availability (Figure 4).
Figure 4. An avidly contrast-enhancing mass is noted on MRI within the right central cerebrum of this geriatric cat with vestibular signs. No definitive diagnosis was made, but the association with the lateral ventricle raises concern for an ependymoma.
Spine
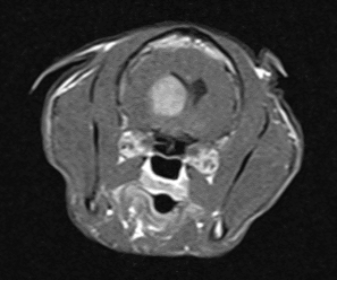
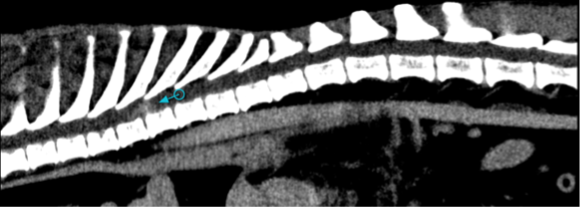
Similar to imaging of the brain, MRI and CT are both useful for imaging the spine (Figure 5). When particular focus is needed on the bony structures, such as with trauma, CT is superior. CT is also beneficial when there is concern for a pathologic fracture, osteolytic lesions such as diskospondylitis, or osteoproliferative lesions such as osseous-associated caudal cervical spondylomyelopathy. In addition to standard imaging, CT myelography can improve the conspicuity of compression lesions and increase diagnostic accuracy in many cases.
Although radiographic myelography remains a commonly used modality for patients with intervertebral disk degeneration, its strength is in quickly identifying the site of spinal cord compression, rather than assessing for spinal cord disease. In clinics where it is available, MRI allows for evaluation of the spinal cord at the site of compression. Additionally, it can assist in diagnosing neoplasms of the spinal cord, ischemic myelopathy, acute hydrated nucleus pulposus extrusions, and congenital abnormalities.
Figure 5.A poorly circumscribed, contrast-enhancing intramedullary mass is noted within the midthoracic spinal cord on CT (arrow). No definitive diagnosis was made, but neoplasia is suspected in this geriatric canine patient.
Vasculature
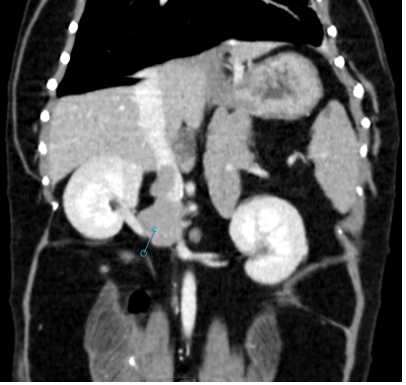
Ultrasound has long been the most common modality for assessing abdominal and limb vasculature. Although ultrasound is a noninvasive, point-of-care tool for assessing for thrombi in the large vasculature (Figure 6), such as the abdominal aorta, its use in diagnosing anomalous vessels, such as portosystemic shunts, is limited by operator experience. Additionally, gastrointestinal gas and noncompliant patients can further hinder identification of anomalous vasculature.
Figure 6. A well-defined right adrenal mass (arrow) can be seen invading the adjacent caudal vena cava as a fingerlike tumor thrombus within this canine patient on CT.
CT angiography (CTA) has largely supplanted ultrasonography in academic institutions for diagnosing portosystemic shunts (Figure 7). In 1 study, the sensitivity of CTA in diagnosing portosystemic shunts was 96% compared with just 68% for ultrasound. In addition to providing better characterization of shunt morphology, CTA was 5.5 times more likely to discern whether a patient had a portosystemic shunt.2 In the past, the need for anesthesia may have deterred clinicians from choosing CTA as a first imaging step, but the speed of image acquisition with newer machines allows for the use of heavy sedation instead.
Figure 7. Three-dimensional reconstruction of a single, extrahepatic portocaval shunt in a juvenile Yorkshire terrier.

Musculoskeletal system
Patients with traumatic fractures, especially following vehicular trauma, commonly present to our emergency service. Radiographs are a first-line imaging modality in these cases, but patients often have complex fractures or luxations, especially of the pelvis. Summation can complicate the accurate diagnosis of these fractures, especially in small bones such as the carpal bones. CT not only allows for an increased conspicuity of fractures, but 3-dimensional models can be produced to facilitate surgical planning.
In addition to traumatic cases, common disease processes such as medial coronoid fragmentation, pathologic fractures, and angular limb deformities can be diagnosed with much more sensitivity and accuracy using CT compared with radiography (Figure 8).
Figure 8. Although medial coronoid fragmentation was evident on radiography in this patient, the adjacent osteochondral lesion of the medial humeral condyle (arrow) was only noted on CT. CT also allowed better evaluation of joint incongruity.

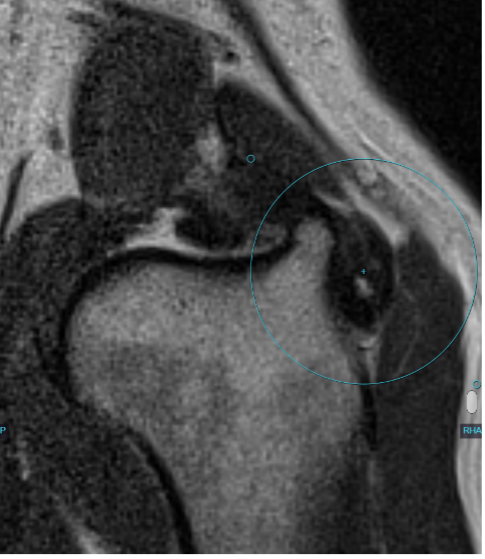
MRI is not yet widely used for musculoskeletal imaging in veterinary medicine, but its ability to diagnose tendinopathies and desmopathies is unmatched by other modalities. Although MRI lacks the portability and cost-effectiveness of musculoskeletal ultrasound, it allows for imaging of some deeper structures that cannot be otherwise assessed (Figure 9).
Figure 9. Thickened infraspinatus tendon with heterogeneous signal (large circle) on MRI. This finding was noted in a geriatric Labrador retriever with a chronic history of bilateral forelimb lameness.
References
- Jeffery ND, Thakkar CH, Yarrow TG. Introduction to computed tomography of the canine brain. J Small Anim Pract. 1992;33(1):2-10. doi:10.1111/j.1748-5827.1992.tb01004.x
- Kim SE, Giglio RF, Reese DJ, Reese SL, Bacon NJ, Ellison GW. Comparison of computed tomographic angiography and ultrasonography for the detection and characterization of portosystemic shunts in dogs. Vet Radiol Ultrasound. 2013;54(6):569-574. doi:10.1111/vru.12059
Eric Van Eerde, DVM, DACVR, is a 2012 graduate of the University of Florida College of Veterinary Medicine in Gainesville. He has worked as an associate radiologist and as director of radiology at BluePearl Specialty and Emergency Pet Hospital in Tampa, Florida.