Antimicrobial therapy in horses (Proceedings)
Shadow is a 7 yr, American Saddlebred Gelding.
"Shadow"
- 7 yr, American Saddlebred, Gelding
- Show horse, pleasure riding. Current light work schedule.
- Current vaccination for West Nile Virus, EEE, WEE, PHF, Influenza, EHV1 and Tetanus.
- Ivermectin q8wks for parasite control.
- Diet: 5lbs 12% sweet feed BID, free choice grass hay
- Housing: Stall, limited individual pasture turnout
- 2004: R eye trauma – corneal laceration & perforation, subsequent blindness & pthisis bulbi
- Intermittent bilateral forelimb lameness associated with foot conformation (club foot L fore) and sole bruising 1gm Phenylbutazone q24h for 6 days prior to presentation
- No abnormalities noted by the owner the evening prior to presentation
- 8am: No abnormalities noted, exercise (light riding), groomed, stall confined and fed normal ration.
- 10am: Found recumbent, depressed, sweating, owners unable to get horse to stand. Referring vet contacted
- 12pm: Referring vet examination
Referring Vet Examination
- HR 110, RR 60, Temp 101.5°F
- MM injected with a toxic line, CRT 3s
- Sunken L eye, prolonged skin tent test
- Skin and distal extremities cold to touch
- Decreased digital pulses in all limbs
- Decreased gut sounds all quadrants, no gastric reflux, no abnormalities on rectal examination
- Profuse watery diarrhea
Treatment: Procaine penicillin IM 20000 IU/kg, Gentamicin IV 6.6 mg/kg, lactated Ringer's solution 7L IV
Referred to VTH
Examination at 6pm
- HR 72, RR 42, Temp 101.4
- MM purple, tongue cyanotic, CRT 3s
- Bilateral serous nasal discharge
- Depressed, sweating
- Decreased GIT motility all quadrants
- Profuse watery diarrhea
- Shifting weight in all limbs, increased digital pulses all limbs
- Decreased jugular fill
- Increased thirst, decreased appetite
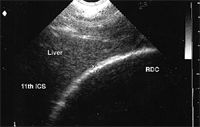
Abdominal ultrasound:
- left dorsal colon wall thickness 0.2mm
- right dorsal colon wall thickness 0.4mm
- fluid filled colon and small intestine
Nasogastric intubation:
- no reflux
Problem list:
- azotemia
- dehydration
- hypochloremia, hyponatremia, hypocalcemia,
- hyperphosphatemia
- hypoalbuminemia
- leukopenia, neutropenia
- diarrhea
- suspected decrease in blood pressure & peripheral perfusion
- laminitis
Differential diagnosis:
- Phenylbutazone associated right dorsal colitis
- PHF
- Salmonella
- Clostridial colitis
- Endotoxemia
Treatment
- Lactated Ringer's solution IV 120ml/kg/day (2.7L/hr) + Calcium gluconate
- Potassium Penicillin 22 000 IU/kg IV q 6h
- Gentamicin 6.6mg/kg IV q24h
- Metronidazole 20mg/kg PO q8h
- Polymixin B 5000 IU/kg IV loading dose, then 1000 IU/kg IV q 12h
- Pentoxifylline 8.5 mg/kg PO q 8h
- Omeprazole 4mg/kg PO q 24h
- Biosponge 120mls PO q12h
Sand bedding
Free choice grass hay and water (16L plain, 16L 10gm/L NaCl/KCl)
Day 2
- HR 60, RR 18, Temp 99.3
- MM dark pink, cyanotic tongue
- 20L water consumed in 12h
- Minimal appetite
- Profuse watery diarrhea
- PCV 42%, TP 5.6 g/dL
- Obel grade 2 laminitis score

Additional treatments:
- Ice feet q6h
- Aspirin 8.5 mg/kg PO q48h
Day 3
- HR 64, RR 30, Temp 99.6
- MM pink and moist, tongue pink
- Depressed
- Profuse watery diarrhea
- PCV 34%, TP 4.2 g/dL
- Obel grade 3 laminitis score
- Oxytetracycline 6.6mg/kg IV q12h
- Lactated Ringer's solution 60ml/kg/day
- Senior feed 1lb q 12h
Day 4-5
- HR 52-60, RR 30, Temp 99.6, MM pink and moist
- Depression, inappetance
- PCV 35%, TP 5.2 g/dL
Euthanasia elected by owner: cost, guarded prognosis for athletic activity, insurance.
Results of Diagnostic tests
- Blood culture: negative
- PHF titer: low titer
Post mortem examination
- Stomach: focal area (8x8.5cm) of hemorrhage and edema in the non glandular portion adjacent to the margo plicatus
- Intestinal contents: watery and foul smelling
- Jejunum, cecum, large colon, small colon : diffuse edema and congestion yellow-green mucus coating
"Johnny"
8 yr old QH gelding

- Use- trail riding, jumping. Recent transport from MO to VA. Housed at boarding stable with 2 horses.
- De-worming & Vaccination current (?)
- 3 days prior to presentation @ VTH; inappetance, fever (103.8F),loose feces. Owner tx w/ PBZ (1gm QD x2)
- AHS visit- pcv 34%, WBC + chem WNL (fibrinogen 400),
- Tx; oxytetracycline (6.6 mg/kg q 12 hr), flunixin (1mg/kg q 12 hr)
- AHS day 2; Dark red MM, toxic line, anorexia T-101F, HR 76, RR 20, stranguria (dark w/ bld + protein),
- Referred to VTH; PCV- 40%, WBC- bands, Chemistry- Cr 1.7, Na 129, Cl 83, Ca 9.2 all other values WNL.
- DDx; colitis, salmonella, PHF, renal dz
- Tx; pentoxifylline, omeprazole, furosemide, ceftiofur (2.2mg/kg BID), LRS + Ca & KCL 2x
- All physical and biochemical parameters (labs, feces, appetite, UA) returned to normal over next 72 hours- Johnny discharged with ceftiofur for 2 days + AHS recheck.
- 4 days post discharge- PHF titer > 2560; tx doxycycline (10mg/kg PO BID)
- 8 days PD- loose feces, t 103F, anorexia, loose feces, WBC- 21.6, fibrinogen 400
- 10 days PD- 'feces hits rotary device' diarrhea, anorexia, depression....back to VTH
- VTH- T 103F, HR 64, RR 16, diarrhea, depression...PCV 51%, WBC 7.4 w/ 19% bands, BUN 29, Cr 2.7, Na 123, Cl 86, bld gas pH 7.19, HCO3 15, UA- bld + protein.
- Tx; Oxytet., metronidazole, pentoxifylline, flunixin, omeprazole, biosponge, LRS + bicarb.
- Ensuing 72 hrs; leukopenia....normal, diarrhea...normal, TP 4.5...normal, pH acidosis....7.34, PCV 32%, urine GGT/Cr=19,
- Discharged after 7 days on doxycycline.
- BAR, temp 98.7F, HR 36, RR 8, PCV 32%
- Salmonella cultures (x5) negative
N risticii
- Gram (-) obligate intracellular bacterium w/ trophism for monocytes.
- Incubation period +/- 10 to 18 days
- Infection of enterocytes in SI and LI = diarrhea.
- Oxytetracycline, doxycycline, erythromycin + rifampin
Pentoxifylline
- Vd = 1.15+/-0.30
- t½ = 0.38+/-0.23
- Suggested dose 10mg/kg BID PO results in comparable serum levels as in humans
- Note: if a decrease in clinical response is experienced increasing the total daily dose to 30mg/kg (either BID or TID dosing) (Liska,2006)
- Methylxanthine derivative.
- Beneficial effects include: improved hemodynamics, inhibition of platelet aggregation, > erythrocyte and leukocyte deformability, > prostacycline release, inhibition of endothelial cell activation and altered leukocyte adhesion.
- Effects attributed to inhibition of cellular phosphodiesterase with > cAMP concentration.
"Imperial"
- 4 month old miniature colt
- Weaned @ 2 months and constantly shown since. Vaccines (?) and daily 'strongid'. Moved to owners farm 2 weeks prior (w/ 3 others). Depressed, febrile and anorectic- wt loss noted. Ventral edema w/ intermittent loose feces.
- rDVM tx= chloramphenicol, metronidazole, ranitidine, omeprazole, probios, panacur x5
- "Imperial"
- rDVM labs- WBC 14.7 (mature neut), fibrinogen 500, Tot prot. 2.1, albumin 0.7, globulin 1.4, Ca 7.0. Treatment for 1 week w/o improvement.
- Presentation @VTH; T 98F, HR 50, RR- rapid shallow, CRT <2, ventral edema ++, loose feces, depressed....
- Labs- lymphocytosis, panhypoproteinemia TP 2.9, albumin 0.9, globulin 2.0, fibrinogen 300; Ca 7.6, phos 5
- DDx; acute bld loss, GI ulceration, protein losing enteropathy (parasites etc), peritonitis, glomerulonephritis, R equi infection...
- Thoracic US- WNL, rads- mild interstitial, Trach asp- mild mixed inflammation, culture= B bronchiseptica. Abdominal US- very thick SI (0.5cm diameter) (minimal free abd fluid) gastric endo.- slight hyperkeratosis, Sheathers (-),
- Tx; plasma (2x 500ml), azithromycin (10mg/kg PO q24 x5 then EOD) flunixin (1.1mg/kg IV BID), omeprazole (4mg/kg QD), SMZ-TMP (25mg/kg PO BID), dexamethaxone (0.1mg/kg PO QD) nutrition consult.
- More Labs; Lawsonia intracellularis PCR (-), serology 1:120 (+). Salmonella (x5) negative
- Progress; following plasma- TP +/- 4.0, edema resolved over 72 hrs, appetite ++, day 6 abdominal US – SI wall thickness much improved, dex discontinued, discharged on day 12 w/ azithromycin (2 weeks), SMZ-TMP, omeprazole.
- 2 weeks post discharge gaining weight and doing well. (** owners recalled that 2 weeks prior to shipping mini's- trailer used to transport pigs!)
Lawsonia intracellularis
- Obligate intracellular bacteria- proliferative enteropathy in swine, dog, rabbit, sheep, deer & horse. Transmission fecal-oral (equine?) tropism for crypt epithelial cells- normal villus structure lost & replaced w/ undifferentiated crypt cells. Minimal inflammatory response. AB's – macrolides, doxycycline, chloramphenicol
"lil appy"
- 7 day old Appaloosa colt
- Two day hx of lameness and lethargy. Mare purchase 2 months prior- unknown vaccination and anthelminitc hx. Foaling unattended and colt discovered under fence unable to rise.
- rDVM – colostrum, ceftiofur. Foal did well until 2 days ago.
- Presentation; 35kg (poor body condition), weak, depressed, HR 100, RR 24, temp 102F lame & effusion rt tarsocrural joint, 5% dehydrated, [umbilicus, mm, crt, resp & GI WNL]
- Initial labs; CBC- leukocytosis (19.8) w/ neutrophilia (17.8) & left shift, fibrinogen 900 Chemistry- hyperglycemia and FPT
- Arthrocentesis of rt tarsocrural joint- cloudy w/ 46.6 nucleated cells (neutrophils) & protein 2.8
- Joint flushed + amikacin (IA)
- Abdominal US- umbilicus normal, increased hyperechoic peritoneal fluid (52.2 nucleated cells + protein 4.4) All fluids submitted for culture.
- Tx; Kpen, amikacin (25mg/kg IV QD), flunixin, omeprazole, plasma (1 L), IV balanced fluids
- Colt improved over 24 hr, stood, suckled, temp 101F
- Radiographs of tarsus & carpus- adequate calcification, no signs of osteomyelitis, septic physitis. Throacic rads & UA = WNL
- Day 3- patent urachus! Confirmed w/ US (Also noted absence of hyperechoic peritoneal fluid!)
- Surgical resection of urachus + abdominal & joint lavage (cell ct 16.1 & protein 2.7)
- Regional perfusion of rt pelvic limb (kpen-22,000 iu/kg QD) for 3 days
- Culture results (peritoneal & synovial) = Listeria monocytogenes
- Sensitivity; amikacin, chloro, enrofloxacin, erythromycin, gentamicin, penicillin, tetracycline, smz-tmp.
- CBC; persistent leukocytosis (27.5) w/ lymphopenia, fibrinogen 300.
- Mare's milk and fecal culture- (-) for Listeria.
- Colt discharged on day 10 w/ smz-tmp (20mg/kg BID PO), flunixin (0.5mg/kg QD PO) omeprazole (4mg/kg QD PO)
- Listeria monocytogenes; gram (+), commonly affects ruminants, fowl, man.
- Clinical; septicemia (neonates), abortion, neurologic dz,
- In horses; depression, diarrhea, pneumonia, neurologic (seizures)
- Caused by ingestion (environment, feces, silage)
- Prognosis favorable w/ early diagnosis & prompt, appropriate treatment
"Darla"
- 35 day old QHx filly
- Intermittent coughing +/- 7 days with increased resp. rate. Appetite decreased but still suckling. No previous issues and adequate PT at birth.
- Presentation; BAR, temp 102F, HR 96, RR 40, wt.94 lbs. Lung sounds diffusely bilat. (no crackles or wheezes) cough easily elicited, mild bilateral ocular discharge, all other systems WNL
- Labs; CBC= leukocytosis (16,000), neutrophilia, fibrinogen 700, Chemistry- glucose 187, otherwise- WNL.
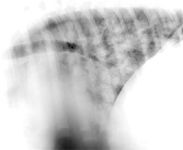
- Thoracic radiographs and US; multiple areas of consolidation (abscessation) bilateral. Diffuse nodular- interstitial pattern w/ cranioventral consolidation.
- Tracheal aspirate; marked neutrophilic septic inflammation. Cultures submitted.
Use of Thoracic ultrasound to screen foals for R. equi at affected farms
Slovis N, McCracken J. Proceedings AAEP, December 2005

Left lateral thorax of foal with R. equi pneumonia. Diffuse nodular opacities greatest near hilus (lymphadenopathy?)
- Hx and initial findings suggestive of Rhodococcus equi infection.
- Treatment; clarithromycin (7.5mg/kg PO BID), rifampin (5mg/kg PO BID) omeprazole, albuterol (MDI- 2 'puffs' BID), beclomethazone (1 'puff' BID 3 days),'Equioxx' (0.2ml PO QD) ophthalmic ointment,
- Day 3; cultures confirmed R.equi, WBC- 11,000, fibrinogen 500.
- Discharged after 2 weeks; continue AB tx & rDVM closely monitor.
"Jordan"
- 13 yr old AQH mare, pleasure horse, trails...
- One week prior, discharged from VTH following colic sx (rt dorsal displacement). All cultures (salmonella, & toxins- C difficile & perfringes (-) PHF titers (-). Discharged w/ flunixin & omeprazole PO.
- Currently- inappetance, diarrhea (profuse, watery), lethargy, dark toxic mm.
- Biopsy (colon) from previous visit- edema, pmn infiltrate, (I/R event?)
- Physical exam; T 99.6, HR 52, RR 16 CRT> 3 w/ dark 'injected' mm.
- Labs; PCV 60%, TP 3.9, WBC 12.3 (PMN 8.5 w/ 7% bands) fibrinogen 200. glucose 235, BUN 58, Cr 3.3, Na 109, Cl 80, albumin 1.9, Bld gas- met acidosis (bicarb 19.9, pH 7.2)
- US- rt. Dorsal colon- 0.4cm
- DDX; salmonella, rt dosal colitis, clostridium, PHF.....
- Initial Tx; balanced fluids (+ bicarb & cmpk) at 2x maintenance. K pen, gent., metronidazole, pentoxifylline, flunixin, polymixin B (6000 IU/kg BID) biosponge, omeprazole, ice feet.
- Day 2- mare BAR & physical parameters improved (mm still injected), diarrhea, ventral edema, adm. 4 L plasma
- Immunology; + for C difficile A/B
- Day 3/4; BAR, diarrhea frequency less, TP still 3.9, PCV 37%, WBC 4.7, fibringen 400
- Nutrition consult; formulated to maximze protein absorption- 3.5lbs alfalfa-grass mix BID, 1 lb 'senior' (Purina) q 5hrs. ½ lbs alfalfa pellets q 6hrs.
- Days 5-12; all parameters improve, CBC improves (10.3, no left shift, TP 5.5, fibrinogen 300); Chemistry & bld gas normalizes, feces formed (loose), appetite good, drinking, (kpen & gent D/C day 10), doxycycline (10mg/kg BID PO) continue metronidazole, flunixin, pentoxifylline, omeprozole....
- Discharged day 15 (flunixin 0.5mg/kg q24)
Clostridium difficile
- Gram- positive, anaerobic, spore-forming rods.
- Ubiquitous, soil, commensal bacterium of intestine. Resistant to most AB's.
- Produces several toxins; entertoxin (toxin A) & cytotoxin (toxin B).
- most commonly associated w/ diarrhea/colitis. Notoriously unpredictable (sever disease to asymptomatic shedding)
- Susceptibility to metronidazole & vancomycin. Increased resistance to metronidazole noted.

JAVMA, Vol 228, No.5, March 2006
Results: Horses may be infected with a number of heterogeneous isolates of C. diff. Toxigenicity and antimicrobial susceptibility vary and metronidazole-resistant strains may be associated with severe disease.
"Blazin"
- 2 day old AQH colt
- Presented for depression, ill thrift and lack of suckling.
- Initial exam; alert, responsive, T 102F, HR 104, RR 28, CRT 2 sec, dehydrated, auscultation- GI 'watery', joints- thorax- umbilicus NAF.
- Initial labs; PCV 39%, WBC 1.5, bands 15%, lymphs 0.46, bld gas- met acidosis pH 7.28, HCO3 19, Chem- albumin 2.9, Ca 10.6
- Condition quickly deteriorates (colic & diarrhea)
- More samples- bld & fecal culture (+ salmonella PCR), sheathers, urine, PT(snap)
- Abd. US- distended loops +/- peristalsis, umbilicus WNL, abd rads- multiple gas filled loops, no reflux.
- Immunology- C perfringes- entertoxin (+). C difficile A & B (-), rotavirus (-)
- Initial Tx; K pen, amikacin, metronidazole, esomeprazole 40mg IV q24), flunixin (1mg/kg q12) 'Plasmalyte' + bicarb & dextrose, biosponge.
- Next 48 hrs; CBC improves- PCV 29.5%, WBC 7.15 (9% bands) lymphs 2.1, TP 5.9, Chemistry- respectable, bld gas- better.
- Foal is BAR, suckling, diarrhea resolving. Salmonella cultures pending- PCR (-)
- Discharged; metronidazole, naxcel 2.2mg/kg IM BID), biosponge.
Clostridium perfringens
- Gram-positive, anaerobic, spore forming
- Found in soil and GI tract of most vertebrates.
- Foals with C perfringens – associated enterocolitis that are < 3 days often have bloody diarrhea but dz is sporadic.
- Reports suggest that > 90% of foals at 3 days of age shed organism in feces.