Blood pressure monitoring and hypertension (Proceedings)
Blood pressure is determined by total peripheral resistance (vascular tone) and cardiac output.
Blood Pressure Regulation
Blood pressure = cardiac output X total peripheral resistance
cardiac output = stroke volume X heart rate
Blood pressure is determined by total peripheral resistance (vascular tone) and cardiac output. Cardiac output is determined by heart rate and stroke volume, which is impacted by contractility and preload. Control of blood pressure is by a variety of mechanisms.
Blood Pressure Measurement
Measurement of blood pressure is a matter of much research and debate. Direct arterial pressure monitoring provides the most accurate reliable results, but is not conducive to outpatient measurement or repeated measurement over several different hospital stays, because of the need to cannulate an artery. Therefore, indirect pressure measurements are the method of monitoring outpatients. Oscillometric blood pressure monitors (e.g., Dinamap, Cardell, SurgiVet) have an air filled cuff that surrounds the vessel. The machine inflates the cuff and then measures the oscillations in the air as the pressure is slowly decreased. At the point at which the pressure in the vessel equals the pressure in the cuff, blood flow through the vessel will resume, increasing the oscillations in the cuff due to the pulsatile nature of blood flow. The machine detects this pressure, and will display the systolic, diastolic, and the mean pressure, as well as the heart rate. When using an oscillometric monitor, the first few readings should be discarded. Once 5-10 readings that are tightly clustered have been obtained, they can be averaged for a reasonably accurate measurement. If the heart rate registering on the machine is widely at variance with the measured heart rate, discard the reading.
Doppler ultrasound technology utilizes a Doppler crystal to amplify the sounds of blood flow through a vessel. The crystal is placed over the artery and positioned so that a strong signal is obtained. Common areas to use include just proximal to the metacarpal or metatarsal foot pad, the base of the tail, or the dorsal metatarsal artery on top of the hind foot. Shaving the hair decreases the trapped air that dampens the signal. In short coated breeds, alcohol may be sufficient without clipping. A cuff placed proximal to the crystal is inflated to occlude blood flow. As the pressure is released, the systolic pressure can be determined at the pressure at which blood flow resumes. Diastolic pressure measurement, determined by a change in the character of the blood flow (a dampening of the sound), is subjective and unreliable. A mean pressure is not obtained by this method. Doppler readings are more accurate in lower pressure ranges than oscillimetric machines.
The appropriate size cuff to use is one whose width is 40% of the circumference of the limb. Larger cuffs are needed for larger animals, and a larger cuff is used for measurements high on the hind leg compared to lower on the leg where the limb is smaller. Too large a cuff will lead to an artificially low blood pressure measurement; conversely, too small of a cuff will lead to inaccurately high readings.
Stress associated with the clinic visit ("whitecoat" effect) can transiently elevate the blood pressure, causing a diagnosis of hypertension to be made incorrectly. Minimizing the stress associated with measuring the blood pressure is critical in obtaining reliable results. The blood pressure should be measured in a quiet environment, such as the exam room, with the owner present. Ideally, the blood pressure is measured before the veterinarian starts the physical examination, and should definitely be done prior to taking the temperature or drawing blood samples. Because each brand of blood pressure monitor may give slightly different readings (for example, a reading of 120 mmHg on one machine may correspond to a 125 mmHg reading on another machine), consistency with repeated visits, including using the same type of machine, same environment, and hopefully even the same technician increases the reliability of measurements and makes analyzing trends more accurate.
Just as the reference range for creatinine varies with breed, the normal range for blood pressure varies between breeds. Reference ranges have been determined for some breeds.
Hypotension
The definition of hypotension will vary based on whether the patient is awake or under anesthesia.
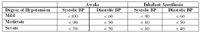
Definition of hypotension
Hypotension is caused by a decrease in one or more of the factors that determine blood pressure: decreased heart rate, decreased stroke volume (i.e., dehydration or heart failure), or decreased peripheral resistance. Signs of hypotension included a prolonged capillary refill time (> 2 seconds), pale mucous membranes, weak pulse, cold feet, reduced level of consciousness, and decreased or absent urine output.
Treatment of hypotension usually needs to occur rapidly to avoid permanent organ damage from lack of oxygen delivery.
- Fluid replacement: First treatment in most cases except cardiogenic causes. Fluid choices may include crystalloid fluids (i.e., LRS or saline, 10-20 ml/kg over 20 minutes), colloids (i.e., hetastarch 10-15 ml/kg in dogs, 5-10 ml/kg in cats), or blood transfusion.
- Remove the underlying cause when possible
- Vasopressors: May be required when peripheral resistance is decreased. Dopamine, dobutamine, and norepinephrine are administered by a constant IV infusion and have an onset of action within minutes of starting or changing the dose.
Hypertension
Definitions of hypertension vary, but a panel of experts including cardiologists, nephrologists, and ophthalmologists have set forth risk categories based blood pressure.

Definition of hypertension
Many conditions have been associated with hypertension, including renal failure, heart disease, hyperthyroidism, and hyperadrenocorticism. Primary hypertension is the most common cause in people but is rare in veterinary medicine. The incidence of hypertension in animals with CRF is high, around 20% in cats. Animals with nephrotic syndrome are at greater risk, with about 60% of dogs with glomerulonephritis having hypertension.
The effects of hypertension are mainly on the small arteries and arterioles. These changes are often the cause of the end organ dysfunction. Left ventricular hypertrophy is a common cardiac change, which can be associated with a murmur if severe. Retinal changes include dilated tortuous retinal vessels, hemorrhage, edema, and detachment. Prognosis for return to vision after an acute retinal detachment is 50%, if blood pressure can be controlled in a timely fashion (within 24 hours). This should be treated as an emergency if vision is to be restored. The renal changes due to hypertension lead to progression of the renal failure by exacerbating glomerular sclerosis. A cerebrovascular accident can cause abrupt onset of neurologic signs.
Treatment of Hypertension
Calcium Channel Blockers: Calcium channel blockers cause relaxation of vascular smooth muscle, an effect that is more profound in vessels with a high resting tone (i.e., in coronary and skeletal muscle beds), which decreases peripheral resistance and thus blood pressure. Cardiac effects include decreasing heart rate and decreasing stroke volume. Certain calcium channel blockers are more selective for peripheral blood vessels with fewer cardiac effects, and include amlodipine (Norvasc). This makes them ideal for treating hypertension without causing adverse heart effects.
Amlodipine is effective for single agent therapy in 60% of cats with hypertension. Cats that were not adequately controlled (blood pressure < 165 mmHg) still had substantial decreases in systolic blood pressure with amlodipine therapy. Amlodipine has a slow onset of action and long lasting effect, which results in a gradual and sustained decrease in blood pressure. Side effects have not been reported in cats. The recommended dose is 0.625-1.25 mg per cat once daily. It does not cause hypotension if given to a normotensive cat, and has effect within 7 days. For many, amlodipine has become the first drug of choice.
Angiotensin Converting Enzyme Inhibitors: Hypotension and hypovolemia cause low sodium delivery to specialized cells of the nephron called the macula densa. This causes release of renin, which cleaves angiotensinogen to angiotensin I. Angiotensin converting enzyme in endothelial cells in the lungs converts angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor, in addition to decreasing salt and water excretion. ACE inhibitors block conversion of angiotensin I to angiotensin II and are effective antihypertensive agents. ACE inhibitors (and angiotensin receptor antagonists) can also decrease proteinuria, making them a good choice for patients with hypertension and proteinuria. Because of the mechanism of action of ACE inhibitors, use of ACE inhibitors in hypovolemic animals may decrease renal blood flow, thus decreasing glomerular filtration rate and worsening azotemia. Other side effects include hypotension.
A variety of ACE inhibitors are available, including enalapril (Enacard, Vasotec), benazepril (Lotensin, Fortekor), captopril, and lisinopril.
The oral dose of enalapril is 0.25-0.5 mg/kg q 12-24 hours, and for benazepril 0.5-1.0 mg/kg q 24 hours. I typically start at the low end of the dose range and titrate upwards as needed to control blood pressure. I recommend rechecking a chemistry panel for worsening azotemia and hyperkalemia 1 week after starting an ACE inhibitor or adjusting the dose.
Beta-Adrenergic Antagonists: Beta-blockers can help control hypertension by decreasing cardiac output and decreasing renin release. The dose for atenolol is 6.25-12.5 mg/cat q 24 hours and for propranolol is 2.5-5 mg/cat q 8-12 hours. Cats with hypertension secondary to hyperthyroidism may respond well to beta-blockade.
Alpha Adrenergic Antagonists: Alpha-blockers (i.e. prazosin, phenoxybenzamine) oppose vasoconstriction and act as antihypertensives. They carry the risk of symptomatic hypotension, especially after the first dose. These drugs are not commonly used for hypertension. Prazosin (Minipress) is an alpha-adrenergic antagonist that reduces preload and afterload. It is supplied in 1 mg capsules, with a dose of 1 mg per 15 kg PO BID-TID, making it inconvenient for cats or small dogs.
Vasodilators: Hydralazine is a direct acting arteriolar dilator. It may be useful in emergency situations when immediate blood pressure control is necessary (i.e. retinal detachment, CNS signs) because the onset of action is rapid (about 1 hour with oral administration, 15 minutes if subcutaneous). It should be given in conjunction with a B-blocker to control heart rate.
Sodium nitroprusside is an arterial and venous vasodilator that is administered as a constant rate intravenous infusion. Because of the potential for cyanide toxicity in cats, the dependence on renal excretion of metabolites, and the need to administer it as a constant infusion with direct arterial pressure monitoring, it is rarely used in treating hypertension.
Diuretics: Diuretics are a standard therapy in primary hypertension in humans (an uncommon condition in animals) and hypertension induced by heart disease. Thiazide diuretics or spironolactone are occasionally used to treat hypertension associated with renal failure. Loop diuretics, although more potent, carry such a great risk of volume depletion that worsens renal failure that they are rarely used.
Diet: A low salt diet (to avoid fluid retention) is almost always recommended in therapy for hypertension, despite any proof of efficacy in animals.
Monitoring
The goal of treatment is to maintain systolic blood pressure at less than 160 mmHg. Blood pressure should be rechecked one week after starting a drug or changing the dose. Once the dog or cat is stable on medications, reevaluation should be performed every 2-3 months.