Canine pyometra: Early recognition and diagnosis
Find out what you need to know to identify pyometra as early as possible.
Canine pyometra is an infectious and inflammatory disorder of the uterus typically occurring in adult, intact bitches during or immediately after the luteal phase of the estrous cycle. The clinical signs of pyometra are often nonspecific and vary among patients depending on the chronicity of the disease and the patency of the cervical canal. Early recognition, diagnosis, and treatment of pyometra are necessary to achieve a successful outcome.

Jeff Dennis, DVM, DACVIM; Brian Lucas Hamm, DVM
In this article, we review the pathophysiology, signalment, clinical signs, and diagnosis of canine pyometra. And in the next article, we summarize the surgical and medical management options available for treating this condition.
PATHOGENESIS
The physiologic changes responsible for predisposing a uterus to pyometra are not completely understood. The vagina is not a sterile environment. Many bacteria types have been cultured from the normal vaginal vault, including Escherichia coli and Staphylococcus, Streptococcus, Klebsiella, Pasteurella, Pseudomonas, and Proteus species.1-3 These same bacteria are commonly cultured from the uteri of patients with pyometra,4-10 which suggests that bacteria ascending from the dog's vaginal vault are the likely source of uterine infection in most patients developing pyometra.11 In a study of 10 dogs with pyometra, the bacteria isolated from the uterus were genetically similar to those found in the patients' gastrointestinal tracts, demonstrating that bacteria within a patient's own body—and not exogenous bacteria—are responsible for infection. Primary urinary tract infections and the hematogenous spread of bacteria from nongenitourinary sites have been suggested to be less frequent sources of infection than ascending infections from the vagina.11,12
However, bacterial contamination of the uterus does not appear to be solely responsible for the development of pyometra. Vaginal bacteria will normally cross the cervix into the uterus when the cervix is open (proestrus and estrus), yet pyometra does not routinely develop.2 Other uterine factors are thought to predispose the uterus to progressive infection.
Studies performed in the 1950s suggested that cystic endometrial hyperplasia is a prerequisite for the development of pyometra in a bitch.6,13 Cystic endometrial hyperplasia develops in most intact female dogs as they age. It is caused by chronic recurrent exposure of the endometrial lining to progesterone produced by the corpus luteum during diestrus. Binding to uterine receptors, progesterone induces endometrial gland proliferation, stimulates endometrial gland secretions, decreases myometrial contractility, and induces closure of the cervix.7 Progesterone has also been shown to interfere with immune function within the uterus, possibly increasing its susceptibility to bacterial infection.14,15 Progesterone's effect on the endometrium is cumulative from reproductive cycle to reproductive cycle.16
The studies suggested that accumulating uterine secretions, prominent endometrial gland crypts, and immunosuppression caused by progesterone stimulation during diestrus make the uterus an ideal environment for bacterial proliferation leading to pyometra.6 This condition has been subsequently termed cystic endometrial hyperplasia-pyometra complex.6,17
Not all dogs with pyometra have cystic endometrial hyperplasia. Other factors can play a role in the development of pyometra. Studies have demonstrated that irritants within the uterus, such as foreign material that has passed through the cervix or even a subclinical bacterial infection, may induce endometrial inflammation and hyperplasia.10,18 These endometrial changes contribute to a favorable environment for bacterial colonization or proliferation, leading to pyometra. The propensity of some pathogenic bacteria, such as E. coli, to attach to the endometrium may explain why some bitches without cystic endometrial hyperplasia develop pyometra.17 Exogenous hormones can also prime the uterus for infection. Pyometra has been noted to occur after the exogenous administration of estrogen used to inhibit pregnancy after a mismating.19-22 Exogenous estrogen enhances the uterus's sensitivity to endogenous progesterone.22
The sequence of pathophysiologic events leading to pyometra varies among bitches and continues to be studied. A consistent factor in the development of pyometra is the presence of a progesterone-primed uterus.
SIGNALMENT
It has been suggested that pyometra is a condition of middle aged and older dogs.22-25 However, pyometra has been reported in dogs as young as 4 months old and as old as 16 years.4,12,22 A study from Japan of 165 colony-raised beagles revealed a prevalence of 15.2% in nonspayed female dogs over the age of 4.23 In this study, the average age of onset was about 9 years. A Swedish study reported the prevalence of pyometra at about 25% in intact, publicly owned female dogs under the age of 10 and about 2% in bitches more than 10 years old.24 In yet another survey, the mean age of dogs presenting with pyometra was 2.4 years.12 The younger age was attributed to the frequent administration of estrogens for mismating in this population.
Pyometra can occur in any breed of dog. Breeds thought to be predisposed to pyometra include rough-coated collies, rottweilers, miniature schnauzers, Cavalier King Charles spaniels, golden retrievers, Bernese mountain dogs, and English springer spaniels.16,24,26 Breeds thought to have a decreased predisposition to pyometra include Drevers, German shepherds, dachshunds, and Swedish hounds.24 Not all studies have confirmed a breed disposition.9 Meanwhile, previous pregnancy has been reported to be protective in some dog breeds but not in all.22,26
CLINICAL SIGNS
The clinical signs associated with pyometra typically appear one to three months after the completion of estrus.6,7 Most of the clinical signs are not specific for pyometra, including lethargy, depression, pyrexia, anorexia, vomiting, diarrhea, polydipsia, and polyuria. A serosanguineous to mucopurulent vaginal discharge can be seen if the cervix is open. Vaginal discharge may be the only clinical finding in some patients.
In patients with closed-cervix pyometra, vaginal discharge may not be present. Dogs with closed-cervix pyometra are often more seriously ill at the time of diagnosis than those with open-cervix pyometra.16 A closed cervix inhibits the elimination of the infectious uterine material, delaying the recognition of illness and increasing the likelihood of complications such as septicemia, endotoxemia (most commonly associated with E. coli infection), and septic peritonitis.5 Bacterial contamination in cases of septic peritonitis may be the result of uterine rupture, translocation of bacteria across the diseased uterine wall, or, less likely, oviduct leakage. More severely afflicted closed-cervix patients may present with signs of shock, dehydration, or collapse.5
DIAGNOSTIC TESTING
A history of recent estrus and typical clinical signs, especially vaginal discharge, should raise your suspicion for pyometra. In patients lacking vaginal discharge, the diagnosis can be more challenging. An enlarged uterus may be palpated within the abdomen; however, aggressive attempts at palpation should be avoided to prevent inadvertent uterine rupture. Other potential causes of vaginal discharge or uterine enlargement, including pregnancy, estrus, hydrometra, mucometra, vaginitis, neoplasia, and uterine torsion, need to be considered as differential diagnoses.
Laboratory findings
Laboratory findings in patients with pyometra are not specific for pyometra and frequently reflect the presence of inflammation and secondary metabolic disturbances. The results of a complete blood count will often demonstrate a neutrophilia with a regenerative left shift; however, a normal white blood cell count or even a neutropenia with a degenerative left shift may be identified in animals with endotoxemia.7,12 Chemotactic chemicals released from the inflamed uterus attract neutrophils to the uterine lumen where they become sequestered.7 Eventually, the bone marrow may not be able to keep up with the demand for mature neutrophils, leading to a degenerative left shift. A high white blood cell count may be seen after surgical removal of the uterus, as neutrophils are no longer sequestered. Mild normocytic, normochromic anemia has been documented in dogs, possibly secondary to bone marrow suppression associated with the uterine inflammation and its associated toxemia.7
The most commonly encountered biochemical abnormalities reported include elevated alkaline phosphatase and alanine transaminase activities, and blood urea nitrogen (BUN), creatinine, globulin, and total protein concentrations.12 Bacterial endotoxemia and reduced liver perfusion are thought to contribute to the elevated liver enzyme activities. Dehydration will frequently contribute to elevated BUN and creatinine concentrations, although concurrent kidney insufficiency in an older dog may also be responsible for the azotemia.4,27 Kidney damage secondary to immune complex deposition has not been substantiated in recent studies.28,29 Hyperglobulinemia and elevated total protein concentrations can occur secondary to chronic inflammation and dehydration. Although less commonly encountered, hypoglycemia can be attributed to septicemia.
Urinalysis findings can be variable. Many patients will have a high urine specific gravity secondary to dehydration. In other patients, the urinalysis will reveal isosthenuria, hyposthenuria, proteinuria, or bacteriuria.7,10 The loss of urine-concentrating ability by the kidneys reported in some patients may be secondary to bacterial endotoxin impairment of renal tubule function.10,12,28 Meanwhile, the presence of severe proteinuria at the time of treatment has been associated with the future development of renal failure in some dogs.29 To retrieve urine for evaluation, a free-catch sample is preferred. Collecting urine by cystocentesis—even if performed with ultrasound guidance—can lead to inadvertent uterine puncture and subsequent leakage of infectious material into the peritoneal cavity.
Radiography
Abdominal radiography can raise suspicion for pyometra. Lateral radiographic projections may reveal craniodorsal displacement of the small bowel and a contorted homogeneous tubular opacity in the caudoventral abdomen (Figure 1).30 The ventrodorsal radiographic projection may reveal cranial and medial displacement of the small bowel.30 Both tissue-dense uterine horns can sometimes be visualized.

Figure 1. A lateral abdominal radiograph of a dog with pyometra. The largely distended uterus can be visualized filling the caudal and mid-abdomen. Cranial and dorsal displacement of the small bowel are evident.
However, radiography can be insensitive for detecting pyometra since uterine distention typically cannot be detected until the diameter of the uterus is larger than that of the adjacent small bowels. In addition, radiography cannot distinguish pyometra from other causes of uterine distension, such as mucometra or early pregnancy (prior to fetal skeletal mineralization).
Abdominal ultrasonography
Abdominal ultrasonography is the preferred method for evaluating patients for pyometra. The most common ultrasonographic finding is distention of the uterus with an anechoic to hyperechoic fluid (Figure 2).31,32 A thickened and cystic endometrium is suggestive of concurrent cystic endometrial hyperplasia.33 In patients with uterine rupture, free fluid may be identified within the abdominal cavity, and the omentum may be hyperechoic secondary to bacterial peritonitis. Abdominal ultrasonography can also be used to exclude other conditions that can cause uterine enlargement or vaginal discharge, such as early pregnancy.

Figure 2. An ultrasonographic image of an enlarged and tortuous uterine horn filled with an anechoic to hypoechoic fluid.
Cytology
Vaginal cytology in patients with open-cervix pyometra will typically demonstrate excessive numbers of degenerate neutrophils and intracellular and extracellular bacteria (Figure 3).12 A cytologic finding of inflammation can be seen in patients with vaginitis and, thus, is not diagnostic of pyometra without additional confirmatory testing. The absence of excessive neutrophils and bacteria in the vaginal discharge would warrant reconsideration of the cause of the patient's condition. Meanwhile, vaginal cytology findings in patients with completely closed-cervix pyometra may only reflect the patient's stage of estrous cycle. Expected cytologic findings during diestrus would include a predominance of intermediate and parabasal cells and, early in diestrus, an influx of nondegenerate neutrophils.
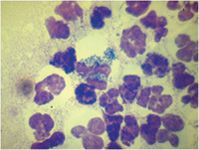
Figure 3. Degenerative neutrophils with intracellular bacteria present in vaginal discharge from a dog with open-cervix pyometra.
For guidance on how to treat canine pyometra—whether medically or surgically—see the article Surgical and medical treatment of pyoderma.
Brain Lucas Hamm, DVM
Jeff Dennis, DVM, DACVIM
BluePoint Specialty & Emergency Medicine for Pets
11950 W. 110th St., Suite B
Overland Park, KS 66210
REFERENCES
1. Bjurstrom L, Linde-Forsberg C. Long-term study of aerobic bacteria of the genital tract in breeding bitches. Am J Vet Res 1992;53:665-669.
2. Baba E, Hata H, Fukata T, et al. Vaginal and uterine microflora of adult dogs. Am J Vet Res 1983;44:606-609.
3. Watts JR, Wright PJ, Whithear KG. Uterine, cervical and vaginal microflora of the normal bitch throughout the reproductive cycle. J Small Anim Pract 1996;37:54-60.
4. Stone EA, Littman MP, Robertson JL, et al. Renal dysfunction in dogs with pyometra. J Am Vet Med Assoc 1988;193:457-464.
5. Nelson RW, Feldman EC, Stabenfeldt GH. Treatment of canine pyometra and endometritis with prostaglandin F2 alpha. J Am Vet Med Assoc 1982;181:899-903.
6. Dow C. The cystic hyperplasia-pyometra complex in the bitch. Vet Rec 1957;69:1409-1415.
7. Hardy RM, Osborne CA. Canine pyometra: pathogenesis, physiology, diagnosis and treatment of uterine and extra-uterine lesions. J Am Anim Hosp Assoc 1974;10:245-268.
8. Memon MA, Mickelsen WD. Diagnosis and treatment of closed-cervix pyometra in a bitch. J Am Vet Med Assoc 1993;203:509-512.
9. Wheaton LG, Johnson AL, Parker AJ, et al. Results and complications of surgical treatment of pyometra; a review of 80 cases. J Am Anim Hosp Assoc 1989;25:563-568.
10. Verstegen J, Dhaliwal G, Verstegen-Onclin K. Mucometra, cystic endometrial hyperplasia, and pyometra in the bitch: advances in treatment and assessment of future reproductive success. Theriogenology 2008;70:364-374.
11. Wadas B, Kuhn I, Lagerstedt AS, et al. Biochemical phenotypes of Escherichia coli in dogs: comparison of isolates isolated from bitches suffering from pyometra and urinary tract infection with isolates from faeces of healthy dogs. Vet Microbiol 1996;52:293-300.
12. Feldman EC, Nelson RW. Cystic endometrial hyperplasia/pyometra complex. In: Canine and feline endocrinology and reproduction. 3rd ed. St. Louis, Mo: Saunders, 2004; 852-867.
13. Dow C. Experimental reproduction of cystic hyperplasia-pyometra complex in the bitch. J Pathol Bacteriol 1959;78:267-278.
14. Sugiura K, Nishikawa M, Ishiguro K, et al. Effect of ovarian hormones on periodical changes in immune resistance associated with estrous cycle in the beagle bitch. Immunobiology 2004;209:619-627.
15. Faldyna M, Laznicka A, Toman M. Immunosuppression in bitches with pyometra. J Small Anim Pract 2001;42:5-10.
16. Pretzer SD. Clinical presentation of canine pyometra and mucometra: a review. Theriogenology 2008;70:359-363.
17. De Bosschere H, Ducatelle R, Vermeirsch H, et al. Cystic endometrial hyperplasia-pyometra complex in the bitch: should the two entities be disconnected? Theriogenology 2001;55:1509-1519.
18. Arora N, Sandford J, Browning GF, et al. A model for cystic endometrial hyperplasia/pyometra complex in the bitch. Theriogenology 2006;66:1530-1536.
19. Bowen RA, Olson PN, Behrendt MD, et al. Efficacy and toxicity of estrogens commonly used to terminate canine pregnancy. J Am Vet Med Assoc 1985;186:783-788.
20. Sutton DJ, Geary MR, Bergman JG. Prevention of pregnancy in bitches following unwanted mating: a clinical trial using low dose oestradiol benzoate. J Reprod Fertil Suppl 1997;51:239-243.
21. Whitehead ML. Risk of pyometra in bitches treated for mismating with low doses of oestradiol benzoate. Vet Rec 2008;162:746-749.
22. Niskanen M, Thrusfield MV. Associations between age, parity, hormonal therapy and breed, and pyometra in Finnish dogs. Vet Rec 1998;143:493-498.
23. Fukuda S. Incidence of pyometra in colony-raised beagle dogs. Exp Anim 2001;50:325-329.
24. Egenvall A, Hagman R, Bonnett BN, et al. Breed risk of pyometra in insured dogs in Sweden. J Vet Intern Med 2001;15:530-538.
25. Johnston SD, Root Kustritz MV, Olson PS. Disorders of the canine and uterine tubes (oviducts). In: Canine and feline theriogenology. 3rd ed. Philadelphia, Pa: Saunders, 2001;206-224.
26. Hagman R, Lagerstedt AS, Hedhammar A, et al. A breed-matched case-control study of potential risk-factors for canine pyometra. Theriogenology 2011;75:1251-1257.
27. Asheim A. Pathogenesis of renal damage and polydipsia in dogs with pyometra. J Am Vet Med Assoc 1965;147:736-745.
28. Maddens B, Daminet S, Smets P, et al. Escherichia coli pyometra induces transient glomerular and tubular dysfunction in dogs. J Vet Intern Med 2010;24:1263-1270.
29. Heiene R, Kristiansen V, Teige J, et al. Renal histomorphology in dogs with pyometra and control dogs, and long term clinical outcome with respect to signs of kidney disease. Acta Vet Scand 2007;49:13.
30. Root CR. Abdominal masses. In: Thrall DE, ed. Textbook of veterinary diagnostic radiology. 4th ed. Philadelphia, Pa: Saunders, 2002;493-515.
31. Voges AK, Neuwirth L. Ultrasound diagnosis-cystic uterine hyperplasia. Vet Radiol Ultrasound 1996;37:131-132.
32. Fayrer-Hosken RA, Mahaffey M, Miller-Liebl D, et al. Early diagnosis of canine pyometra using ultrasonography. Vet Radiol Ultrasound 1991;32:287-289.
33. Bigliardi E, Parmigiani E, Cavirani S, et al. Ultrasonography and cystic hyperplasia-pyometra complex in the bitch. Reprod Domest Anim 2004:39:136-140.