Clinical Rounds: Transitional cell carcinoma
Thousands of dogs develop this form of cancer every year. Follow along as these clinicians delve in the particulars of a case in a senior Chihuahua-and see how you can best prolong survival in the next patient you diagnose with this form of neoplasia.
Transitional cell carcinoma (TCC) is the most common urinary tract cancer in dogs, affecting thousands each year.1-4 Risk factors for developing TCC are multiple and include obesity, female sex, exposure to older-generation flea control products, and exposure to herbicides and pesticides.2,5-8
Scottish terriers, Shetland sheepdogs, beagles, wire-haired fox terriers, and West Highland white terriers have a predilection to develop TCC.2,5-8 The Scottish terrier is the most at-risk breed for developing this tumor-an odds ratio of 18.09.2 Additionally, obese female dogs exposed to insecticides are 28 times more likely to develop TCC than normal weight dogs.6,8 Interestingly, consuming vegetables at least three times a week in addition to a normal diet seems to reduce the risk of developing TCC in dogs.9
A “field effect” has been proposed for these tumors and refers to the multifocal changes that occur in the bladder as a result of exposure to carcinogens in the urine that cause malignant changes throughout the bladder epithelium. Metastasis to the regional lymph nodes and the lungs is noted in about one of six cases at the time of diagnosis, but it is more common later in the course of disease, with about half of dogs developing metastasis to the lymph nodes, lungs, other abdominal organs, or bones at the time of death.5,10,11
Dogs usually present with lower urinary tract signs (e.g. hematuria, stranguria, pollakiuria, dysuria), and many have concurrent urinary tract infections (UTIs) that may initially delay the diagnosis. Resolving the infection may temporarily alleviate the clinical signs, and patients often present with a several-month history of lower urinary tract signs. A middle-aged dog with its first UTI should prompt imaging of the bladder to rule out bladder stones or a bladder mass.
Quick links
• Clinical pathology perspective
• Anatomic pathology perspective
• Medical oncology perspective
• Radiation oncology perspective
• Summary
CASE PRESENTATION
An about 16-year-old spayed female Chihuahua (5.5 lb [2.5 kg]) presented to the University of Tennessee Veterinary Medical Center for evaluation of a suspected bladder mass found on ultrasonographic examination by the primary care veterinarian. The owners reported that the dog had a history of hematuria for about three months before presentation.
Diagnostic testing
Staging tests included a complete physical examination, a complete blood count, a serum chemistry profile, a urinalysis, an abdominal ultrasonographic examination, an abdominal and thoracic (three-view) radiographic examination, and a urine culture. The abdominal ultrasonographic examination showed a thickening of the bladder wall, with two masses measuring 0.38 x 0.64 cm and 1.9 x 2.3 cm and extending along the craniodorsal and cranioventral wall of the bladder. No other abnormalities were noted. Thoracic and abdominal radiographs revealed no abnormalities and no evidence of metastatic disease.
The dog was anesthetized and positioned in dorsal recumbency for a cystoscopic examination, which revealed multiple botryoid masses along the dorsal bladder wall close to the ureters (Figure 1). Histopathologic examination of biopsy samples revealed TCC, and a culture was positive for Enterococcus species that was susceptible to amoxicillin-clavulanic acid.

Figure 1. A cystoscopy image of the dog's tumor revealing a polypoid mass and areas of necrosis and dystrophic mineralization.
Treatment
Surgical excision was not possible because of the proximity of the tumor to the ureters. Initial treatment included mitoxantrone chemotherapy administered intravenously every three weeks at a dose of 5 mg/m2 in conjunction with piroxicam given orally daily at a dose of 0.3 mg/kg. A complete blood count was performed before and seven days after each mitoxantrone treatment. Serum chemistry profiles were performed intermittently.
Follow-up
Treatment with mitoxantrone was continued every three weeks, and restaging tests were performed every six weeks to monitor tumor status. Restaging consisted of three-view thoracic radiographs, two-view abdominal radiographs, and abdominal ultrasonography to monitor primary tumor size as well as to monitor for evidence of the development of metastasis. For four months, the tumor remained stable based on imaging and clinical signs.
By the time the dog presented for its seventh mitoxantrone treatment, the owner noted that it was less active and was more particular about what it wanted to eat. A complete blood count, serum chemistry profile, urinalysis, and urine culture, as well as abdominal and thoracic imaging, revealed no explanation for the change in the dog's quality of life. No evidence of metastatic disease could be documented, and the tumor appeared relatively stable on abdominal ultrasonographic examination. The owner elected to discontinue chemotherapy since the dog's clinical signs were presumed to be from the chemotherapy treatment.
One month later, the dog presented to the primary care veterinarian because it was lethargic. Blood work revealed severe hyperglycemia, azotemia, and elevated liver enzyme activities. The owner elected to humanely euthanize at that time. The dog's survival time from diagnosis to death was five months. A necropsy was not performed to confirm the cause of the dog's declining quality of life.

CLINICAL PATHOLOGY PERSPECTIVE
Jennifer Scruggs, PhD, DVM
Cells can be acquired a number of ways for cytologic analysis of suspected TCC. Traumatic catheterization and fine-needle aspiration often provide highly cellular samples for analysis, although the potential for seeding neoplastic cells is a consideration.12 Free-catch urine samples may also provide enough cells for analysis, but prolonged cell immersion in urine can result in poor cellular preservation, causing the sample to be nondiagnostic.13
Samples are often highly cellular, with many polygonal to round cells present both individually and in variably sized clusters. Cells can exhibit marked anisocytosis and anisokaryosis, although well-differentiated tumors may exhibit less pronounced criteria of malignancy. Nuclei are often round and centrally placed, with coarse chromatin and one or more prominent nucleoli; mitotic figures, binucleation or multinucleation, and nuclear molding may also be observed (Figure 2). Cells often have moderate amounts of variably basophilic cytoplasm, and a small subset of the cells may contain one or more, large, diffusely to finely stippled, pale-pink to magenta inclusions.14 Large inclusions may displace the nucleus, often to the periphery of the cell.
When cells exhibit marked criteria of malignancy and there is no evidence of inflammation or infection, a diagnosis of carcinoma is not difficult. However, benign cells can exhibit marked atypia in response to inflammation and infection (e.g. cystitis), making interpretation difficult. Additionally, TCC cannot be distinguished from prostatic carcinoma based on cytomorphology alone.
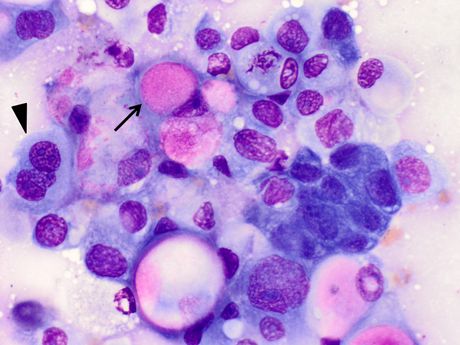
Figure 2. An impression smear made from a biopsy piece from a urethral mass in a dog. The sample contains a dense cluster of round to polygonal cells. The cells have varying amounts of pale-blue to more basophilic cytoplasm; pink inclusions are present in a few of the cells (arrow). Note the moderate anisocytosis and anisokaryosis, variable nuclear-cytoplasmic ratio, prominent nucleoli, and trinucleated cell (arrowhead).

ANATOMIC PATHOLOGY PERSPECTIVE
Jennifer Bernard, DVM, DACVP
Grossly, TCCs are usually a solitary papillary, polypoid, or sessile mass. The most common location in dogs is the trigone of the urinary bladder, but this neoplasm can spread throughout the urinary bladder or arise from the renal pelvis, ureters, urethra, or prostate. However, a dog may present with multiple masses inside the urinary bladder. While there are several differential diagnoses for bladder masses, polypoid cystitis is a common gross differential diagnosis, so histopathologic or cytologic confirmation of the diagnosis is always important.
TCCs are more invasive than other urinary bladder tumors and can extend into the muscular layers. Large, clear cytoplasmic vacuoles are a characteristic histologic feature of neoplastic cells (Figure 3). Nuclei are large and vesicular and contain prominent nucleoli. Mitoses and intravascular invasion are common. Desmoplasia, the fibrous connective tissue stroma induced by certain neoplasms, can be marked in both primary and metastatic sites.
TCCs within the urethra of male dogs may be mistaken for prostatic carcinoma when glandular differentiation is present. Also, immunohistochemical expression of uroplakin III can be used to confirm the origin of the tumor, which is especially useful for identification in metastatic sites when a urinary bladder mass has not been previously identified (e.g. skin or bone).15,16 Samples that are too small or superficial, which may be more likely to occur with endoscopically obtained samples, may lead to an inconclusive biopsy result.
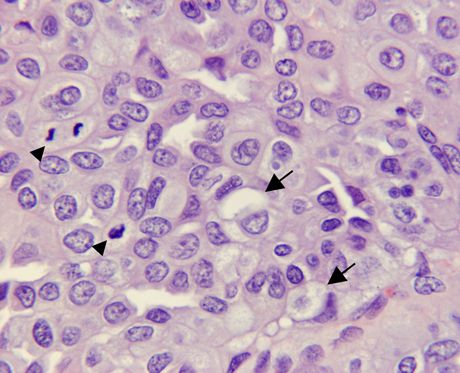
Figure 3. TCC in a dog. Neoplastic cells contain large cytoplasmic vacuoles (arrows), and mitoses (arrowheads) are common (hematoxylin and eosin; 40X).

RADIOLOGY PERSPECTIVE
Silke Hecht, Dr. med. vet., DACVR, DECVDI
Diagnostic imaging in dogs with suspected bladder or urethral TCC is performed to identify lesions and, if identified, assess the extent of disease, evaluate for metastatic disease, and monitor tumor response to treatment. Survey radiographs of the abdomen are useful to identify enlarged sublumbar lymph nodes and evaluate the lumbar and sacrocaudal spine and the pelvis for evidence of osseous metastases or extension of the tumor into the spinal column or pelvis. The primary mass is usually not identified; however, dystrophic mineralization within the tumor or a thickened urethra may be seen in some cases (Figure 4).

Figure 4. A lateral radiograph of the caudal abdomen of a 14-year-old Belgian shepherd with urinary bladder TCC. The radiograph shows irregular stippled mineralization in the plane of the caudal bladder and an unusual contour to the bladder neck area (arrows). Additional findings include mild sublumbar lymph node enlargement (asterisk) and incidental spinal degenerative changes.
Radiographic contrast procedures (cystography, urethrography) have largely been replaced by ultrasonography in the diagnosis of urinary tract neoplasia. However, lesions in an intrapelvic location may be better evaluated by using urethrography or computed tomography (CT) instead of ultrasonography in select cases.
It is important to note that 2D ultrasonography has historically been shown to be an inaccurate method of consistently measuring bladder masses.17 Recently, however, 3D ultrasonography and CT have been shown to provide accurate bladder mass measurements, although the availability of CT and 3D ultrasonography is more limited than the availability of 2D ultrasonography.18 On abdominal ultrasonographic examination, bladder TCCs are usually sessile, irregularly shaped masses of variable echogenicity.19 They are most commonly located at the level of the trigone but may be found in any location. Diffuse infiltration of the bladder wall instead of formation of a distinct mass is less common but possible. Urethral TCCs result in hypoechogenicity and irregular thickening of the urethral wall, often with a hyperechoic line along the epithelial surface.20
Possible concurrent findings include abnormalities of the prostatic gland, hydronephrosis or hydroureter secondary to ureteral obstruction (Figure 5), and evidence of metastatic disease to the lumbar spine, medial iliac lymph nodes, or other abdominal organs. Samples of bladder or urethral masses should ideally be obtained by means of ultrasound-guided traumatic catheterization (“suction biopsy”) instead of percutaneous tissue sampling because of the risk of tumor cell implantation along the needle tract.12 This is especially important for apical tumors in which surgery may be possible.
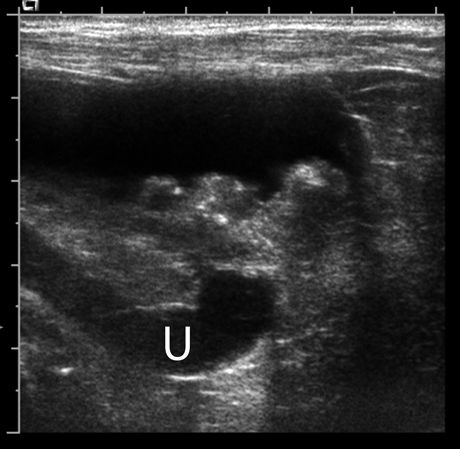
Figure 5. A sagittal ultrasonogram of the urinary bladder demonstrating an irregularly marginated, broad-based mass of mixed echogenicity with multiple strongly hyperechoic foci associated with the dorsal wall of the urinary bladder. A markedly dilated ureter (U) is seen dorsal to the bladder, consistent with ureteral obstruction by the mass.
When monitoring a patient's response to treatment, it is important to keep the ultrasound technique and protocol (e.g. positioning, degree of bladder filling, radiologist) as consistent as possible between examinations to minimize the chance of measurement errors.
CT and magnetic resonance imaging (MRI) of the abdomen are useful in evaluating the primary tumor and associated changes. However, because of the need for general anesthesia, high cost, and low availability, the use of cross-sectional imaging in veterinary practice is currently limited. Thoracic imaging (radiography or, optimally, CT) should be routinely performed in patients with urinary tract TCC to evaluate for metastatic disease to the lungs or osseous structures.


MEDICAL PERSPECTIVE
Joe Bartges, DVM, PhD, DACVIM, DACVN, and Amanda Callens, BS, LVT
Dogs with TCC often have clinical signs of lower urinary tract disease (dysuria, stranguria, hematuria, and inappropriate urination) that may or may not be associated with concurrent bacterial UTIs. Alpha1 antagonists may decrease lower urinary tract signs. Conventionally, prazosin (1 mg/15 kg body weight orally every 12 to 24 hours) and phenoxybenzamine (0.25 to 1 mg/kg body weight orally every eight to 24 hours) have been used; however, tamsulosin (0.001 to 0.1 mg/kg orally every 24 hours) has been shown to be superior.21 Tamsulosin accumulates in urethral and prostatic tissues, providing a more sustained effect.22,23
Bacterial UTIs
Dogs with TCC are prone to bacterial UTIs, which are considered complicated because of urine retention due to mechanical blockage and presence of the cancer. Antimicrobial agents should be based on culture and sensitivity results since resistant UTIs are common. Although cystocentesis is controversial in dogs that have TCC due to the possibility of seeding tumors along the needle tract, urine should be collected by cystocentesis for culture and sensitivity testing. Not all bacterial UTIs require treatment; if clinical signs are not present or are no worse with a positive bacterial culture, then not treating is reasonable.24
Other nonantimicrobial treatments may be considered to aid in the control of bacterial UTIs, such as urinary antiseptics: methenamine mandelate (10 to 20 mg/kg orally with food every eight to 12 hours), methenamine hippurate (500 mg orally with food every 12 hours), or nitrofurantoin (3 to 4 mg/kg orally every 24 hours). Also consider probiotics, cranberry extract, and D-mannose.
Urethral obstruction
With time and despite treatment, urethral obstruction commonly occurs due to growth of the TCC at the urethral opening and down the urethral wall. Many patients still appear to feel well and do not have metastatic disease but are unable to urinate. There are several options for these obstructed patients-intermittent urinary catheterization, transurethral catheter placement, cystostomy catheter placement, and urethral stents. Intermittent urinary catheterization is only a temporary solution. If euthanasia is not considered, then alternative options for promoting urine voiding should be pursued.
Cystostomy catheters are low-profile tubes that are surgically placed into the urinary bladder and exit the abdominal cavity in the inguinal area. Owners empty the urinary bladder three to four times a day by using a syringe. We use bladder irrigation to help control bacterial UTIs with a cystostomy tube. Bladder irrigation is performed with a 0.02% chlorhexidine solution, and 20 to 30 ml is instilled in the bladder through the cystostomy tube after the urine is removed. It is allowed to dwell for 10 to 15 minutes, and then all but 10 ml is removed. This 10-ml 0.02% chlorhexidine solution is allowed to remain in the urinary bladder until the next time urine is removed.
Self-expanding nitinol urethral stents are placed by fluoroscopic or ultrasonographic guidance and permanently open the urethra. Most female dogs are incontinent after urethral stent placement, which may cause some concerns for home and owner exposure to chemotherapy if treatment is pursued after stent placement. Median survival times after stent placement are 32 to 78 days, with some dogs living up to a year.25,26 Complications of stent placement include incontinence (39%), reobstruction (22%), stent migration, and bladder atony. About 20% of dogs with stents may develop urethral obstruction due to progressive growth of the tumor; of these about 10% obstruct due to ingrowth of the tumor through the stent, while about 90% obstruct due to growth of the tumor around the cranial and/or caudal aspects of the stent.27
Ureteral obstruction
If ureteral obstruction occurs due to a TCC, urinary diversion can be performed by either ureteral stents or a subcutaneous ureteral bypass device. Recently, laser ablation of TCC has been described, which may provide relief of clinical signs and possibly longer control of the cancer when used in conjunction with chemotherapy.28

SURGICAL PERSPECTIVE
Rachel Seibert, DVM
Complete TCC resection is difficult because masses usually involve the trigone region and are commonly multifocal, either within the bladder or in the bladder and urethra (in 56% of dogs in one study).2 Because the important neurovascular structures of the bladder are located dorsally, resection of this area is likely to result in incontinence, ischemia, or both. In the aforementioned study of 67 dogs undergoing surgery for TCC, complete resection was possible in less than 3% of affected dogs.2 For these reasons, surgical treatment is considered palliative in most cases and is often used in combination with chemotherapy and nonsteroidal anti-inflammatory drug (NSAID) therapy.
Partial cystectomy
Partial cystectomy is indicated to alleviate obstruction and for debulking in combination with chemotherapy. Major complications of partial cystectomy include dehiscence resulting in uroabdomen, incontinence if the neurovascular supply is damaged, pollakiuria due to reduced bladder capacity, incomplete tumor resection, and recurrence. Urinary catheters are recommended after cystectomy to keep the bladder decompressed, reducing tension on the suture line. In a study of 10 dogs undergoing partial cystectomy for TCC, nine of the dogs developed recurrence or metastasis, and 50% were euthanized within seven months of surgery.29
Although wide surgical margins can be attempted for apical masses, reduction in bladder capacity may result in persistent pollakiuria.29,30 In people, more than 75% of the bladder can be excised with development of a near-normal capacity within three months31; however, the percentage of bladder that can be excised in dogs without long-term pollakiuria or incontinence is unknown. In dogs undergoing 90% cystectomy with only the trigone left intact, mean bladder capacity nine months after surgery was still decreased 72% from baseline, and all dogs had pollakiuria.30 The rate of persistent pollakiuria is 20% when cystectomy includes 40% to 70% of the bladder.29
Because of metabolic complications and poor quality of life, complete cystectomy with urinary diversion is no longer performed.32 An alternative to complete cystectomy is en bloc removal of the bladder neck and proximal urethra with preservation of the dorsal neurovascular pedicle. The goal of en bloc resection is to optimize the probability of achieving long-term tumor control, while attempting to preserve function. This technique was recently described in two dogs in which tumors were causing life-threatening obstruction of the urethra and ureters.33 Both dogs regained continence by 17 days after surgery.
Surgical resection of TCC has been associated with tumor seeding of the abdominal wall or other distant sites.34-36 Seeding of TCC is also suspected to occur with cystocentesis, traumatic urethral catheterization, cystoscopy, and laparoscopy.12,36 When TCC is suspected, the surgeon should minimize tumor handling and change gloves and instruments before body wall closure to reduce the risk of iatrogenic spread.
Palliative treatment
Options for palliative treatment of trigonal TCC include placement of a permanent cystostomy tube, radiation therapy with or without placement of a self-expanding urethral stent, stent placement alone, or laser debulking. A permanent cystostomy tube permits urine diversion in patients that have urethral obstruction but patent ureters. Complications are reported in 49% of dogs and cats undergoing cystostomy catheter placement and include tube dislodgement or obstruction, urine leakage around the tube, persistent fistulation after tube removal, inflammation around the tube exit site, and death secondary to tube complications.37 UTIs are also expected with long-term tube placement.
Tumors that obstruct the urethra and trigone can also be debulked with ultrasound-guided endoscopic diode laser ablation. When laser debulking is combined with medical management, the median survival time was 380 days in one report.28 Multiple treatments are required for up to 50% of cases because of reobstruction with tumor or scar tissue. Other complications include stranguria, hematuria, urethral perforation, and spread of TCC within the urinary tract.28

MEDICAL ONCOLOGY PERSPECTIVE
Sara D. Allstadt, DVM, DACVIM (oncology)
Chemotherapy is often used to treat TCC because of the common trigone location of these tumors as well as common urethral and/or prostatic involvement. Reduction of tumor burden for TCC in dogs has not been well-studied but has been shown to prolong survival times.38-40
Chemotherapy agents
Systemic chemotherapy is often the primary form of treatment for TCC. Standard approaches include either treatment with NSAIDs alone or in combination with systemic chemotherapy agents. Treatment with NSAIDs such as piroxicam, deracoxib, and firocoxib has been reported, although piroxicam is commonly favored as the first-line NSAID by most oncologists, likely because of the higher-reported complete response rate to this drug.41-43 Complete responses have been reported in a small number of cases treated with piroxicam alone, with a median survival time of 5.9 months.41 In a report of 26 deracoxib-treated dogs, the median survival time reported was longer; however, those dogs received other chemotherapy agents after deracoxib treatments, likely influencing their overall survival times.43
Chemotherapy agents used in combination with NSAIDs include mitoxantrone, carboplatin, vinblastine, gemcitabine, vinorelbine, and metronomic chlorambucil. Intravesicular treatment with mitomycin C has also been reported.44 While favorable tumor responses to cisplatin chemotherapy and piroxicam are noted, this combination is not recommended because of the high nephrotoxicity and risk of renal failure (see Table 1).45,46
Mitoxantrone combined with piroxicam is one of the more commonly used chemotherapy protocols for canine TCC.47 The dose of mitoxantrone is typically 5 to 5.5 mg/m2 administered intravenously every three weeks, and piroxicam is administered at 0.3 mg/kg orally once daily with food. Mitoxantrone can cause marked bone marrow suppression, so it is important to monitor the nadir via complete blood counts seven days after administration.
Piroxicam can cause both gastrointestinal upset and nephrotoxicosis, so routine monitoring of a patient's gastrointestinal signs and renal function is recommended. Omeprazole and famotidine are commonly used to reduce risk of gastrointestinal upset. Misoprostol is a synthetic prostaglandin E1 analogue commonly used to prevent NSAID-induced ulceration; however, in my experience, a high number of dogs experience gastrointestinal cramping and upset from this drug. It is also an abortifacient and, thus, women of child-bearing age should not be exposed to this drug.
Prognostic factors
Overall, the prognosis for dogs with TCC is poor, and most dogs succumb to this disease. But new treatments are being identified on a regular basis, and quality of life can be excellent in most dogs while receiving chemotherapy. Dogs with more advanced-stage TCC (e.g. larger tumors invading loco-regionally or with evidence of metastasis) have a less favorable prognosis than those with a lower-stage disease (e.g. smaller, more superficial tumors with no evidence of metastasis).48 Younger dogs have an increased risk of metastasis to lymph nodes, dogs with prostate involvement have an increased risk of distant metastasis, and dogs with larger tumors have an increased risk for both nodal and distant metastasis.49,50 Those with either loco-regional or distant metastasis, as well as dogs whose tumors invade the prostate, urethra, uterus, vagina, and pelvic canal, typically succumb to their disease or experience obstruction from their tumors quicker than those with smaller or more apically located tumors and without evidence of metastasis.49,50
The survival data for dogs with TCC is hard to summarize since many publications describe heavily pretreated dogs or dogs that go on to receive other treatments. However, some deductions may be made from the published data. With NSAID therapy alone, the expected median survival time is about six months, while adding chemotherapy to NSAID therapy is expected to increase the median survival time to approximately nine to 11 months (see Table 1). It is unknown at this time how new procedures such as urethral and ureteral stents and radiation therapy may affect survival times, but these modalities are expected to potentially increase survival.

RADIATION ONCOLOGY PERSPECTIVE
Nathan Lee, DVM, DAVCR (radiation oncology)
Radiation therapy alone-or in combination with chemotherapy, surgery, or both-has been shown to be the best treatment in people with invasive TCCs, which are similar to canine TCC of the bladder.51-55 Radiation therapy has not been extensively studied or recommended as treatment for canine TCC, most likely because of the relatively low availability of veterinary radiation centers. An early report looking at canine bladder cancers treated with intraoperative radiotherapy reported a high rate of post-radiation complications, with 46% of dogs experiencing increased frequency of urination, 46% urinary incontinence, 38% cystitis, and 15% stranguria.56 The complications reported in that article were not surprising since the investigators treated the entire bladder and used a very high fraction dose of 21.88 to 27.00 Gy.56 Even with the reported complications, the median survival time in that report was 16.8 months, which may indicate that radiation therapy may have a role in treatment of this tumor.56
A more recent report in 2004 investigated the use of piroxicam, mitoxantrone, and palliative radiation therapy (six weekly fractions of 5.75 Gy) in 10 dogs with TCC.57 That study concluded that the combination of therapies, which has a response rate of 22% based on ultrasound measurements, was not superior to reports using mitoxantrone and piroxicam alone, which had a response rate of 34.5% based on ultrasound measurements.46,57 Although this finding was not as promising as expected, 90% of patients had amelioration of their urinary clinical signs, and only three dogs were reported to have urinary incontinence as a late side effect.57
A recent study in 2012 investigated the use of radiation therapy to treat TCCs using intensity-modulated radiation therapy, along with image guidance in 21 dogs.58 That study found that the combination of definitive radiotherapy (54 to 58 Gy delivered in 20 daily fractions on a Monday to Friday basis) and chemotherapy resulted in a median survival time of 654 days.58 Acute urinary complications included hematuria (1) and stranguria (1).58 Late complications reported were rectal (1), ureteral (1), and urethral (2) strictures.58 Overall, 19% of patients developed grade three late gastrointestinal or genitourinary toxicosis that typically occurred six to 18 months after radiation therapy.58 All late complications were successfully palliated with either stenting or surgery.58
At the University of Tennessee, we have successfully palliated patients with TCCs of the urinary bladder using 8-Gy fractions once a week for three treatments. With this therapy, we have seen clinical improvement with amelioration of urinary signs in most patients. Anecdotally, we see the most significant improvement seven to 14 days after radiotherapy. Palliative radiation therapy is typically reserved for patients that have failed chemotherapy options. The use of higher fraction sizes to treat TCCs was recently validated in a study from the University of Florida that determined the alpha/beta ratio of three established canine TCC cell lines was low, ranging from 2.67 to 4.59 Cells with a low alpha/beta ratio tend to respond to large fraction sizes better than small fraction sizes, similar to late responding tissues in the body.
It is difficult to figure out the role of radiation therapy in the treatment of canine TCCs because of the few studies available, the small number of patients in each study, and the absence of practice standardization in veterinary radiation oncology. More study is required to fully define the role of radiation therapy in management of canine TCC of the bladder and determine how to reduce complications associated with this therapy. However, my experience combined with literature in both people and dogs affected by this disease suggest that this treatment modality should play a role in management of these dogs.
SUMMARY
At the University of Tennessee, piroxicam is the NSAID of choice for medical management of canine TCC, although deracoxib may be considered as well.41,43 Mitoxantrone is typically chosen as the first-line chemotherapy drug, although other drugs considered and used in the treatment of canine TCC include vinblastine, carboplatin, and chlorambucil, based on the literature and clinical tolerance of canine patients.45,47,60-63 It is important to note that several of these chemotherapy drugs should be dosed differently in small dogs (< 22 to 33 lb [10 to 15 kg]). Urethral and ureteral stenting, as well as radiation therapy, may all be considered as part of a management plan for TCC dogs.
For dogs being treated (particularly those treated with chemotherapy), we use imaging and restaging about every six to eight weeks to monitor response to treatment and determine if alternative therapy is indicated.
ACKNOWLEDGMENT
The authors thank Misty Bailey and Karen Tobias, DVM, MS, DACVS, for editing of the manuscript.
SUGGESTED READING
> Zinkl JG. Examination of the urinary sediment. In: Cowell RL, Tyler RD, Meinkoth JH, eds. Diagnostic cytology and hematology of the dog and cat. 3rd ed. St. Louis: Mosby Elsevier, 2008;350-368.
> Borjesson DL, Dejong K. Urinary tract. In: Raskin RE, Meyer DJ, eds. Canine and feline cytology: a color atlas and interpretation guide. 2nd ed. St. Louis: Saunders Elsevier, 2009;249-259.
> Henry CJ. Bladder and urethral tumors. In: Henry CJ, Higginbotham ML, eds. Cancer management in small animal practice. St. Louis: Saunders Elsevier, 2010;290-295.
> Bryan J. Prostate tumors. In: Henry CJ, Higginbotham ML, eds. Cancer management in small animal practice. St. Louis: Saunders Elsevier, 2010;296-298.
> Knapp DW, McMillan SK. Tumors of the urinary system. In: Withrow SJ, Vail DM, Page RL, eds. Withrow and MacEwen's small animal clinical oncology. 5th ed. St. Louis: Saunders Elsevier, 2013;572-582.
REFERENCES
1. Mutsaers AJ, Widmer WR, Knapp DW. Canine transitional cell carcinoma. J Vet Intern Med 2003;17(3):136-144.
2. Knapp DW, Glickman NW, Denicola DB, et al. Naturally-occurring canine transitional cell carcinoma of the urinary bladder: a relevant model of human invasive bladder cancer. Urol Oncol 2000;5(2):47-59.
3. Valli VE, Norris A, Jacobs RM, et al. Pathology of canine bladder and urethral cancer and correlation with tumour progression and survival. J Comp Pathol 1995;113(2):113-130.
4. Knapp D. Animal models: naturally occuring canine urinary bladder cancer. In: Lerner S, Schoenberg M, Sternberg C, eds. Textbook of bladder cancer. Oxon, United Kingdom: Taylor and Francis, 2006;171-178.
5. Norris AM, Laing EJ, Valli VE, et al. Canine bladder and urethral tumors: a retrospective study of 115 cases (1980-1985). J Vet Intern Med 1992;6(3):145-153.
6. Hayes HM Jr. Canine bladder cancer: epidemiologic features. Am J Epidemiol 1976;104(6):673-677.
7. Knapp DW, McMillan SK. Tumors of the urinary system. In: Withrow SJ, Vail DM, Page RL, eds. Withrow and MacEwen's small animal clinical oncology. 5th ed. St. Louis: Saunders Elsevier, 2013;572-582.
8. Glickman LT, Raghavan M, Knapp DW, et al. Herbicide exposure and the risk of transitional cell carcinoma of the urinary bladder in Scottish terriers. J Am Vet Med Assoc 2004;224(8):1290-1297.
9. Raghavan M, Knapp DW, Bonney PL, et al. Evaluation of the effect of dietary vegetable consumption on reducing risk of transitional cell carcinoma of the urinary bladder in Scottish Terriers. J Am Vet Med Assoc 2005;227(1):94-100.
10. Tarvin G, Patnaik A, Greene R. Primary urethral tumors in dogs. J Am Vet Med Assoc 1978;172(8):931-933.
11. Santos M, Dias Pereira P, Montenegro L, et al. Recurrent and metastatic canine urethral transitional cell carcinoma without bladder involvement. Vet Rec 2007;160(6):557-558.
12. Nyland TG, Wallack ST, Wisner ER. Needle-tract implantation following US-guided fine-needle aspiration biopsy of transitional cell carcinoma of the bladder, urethra, and prostate. Vet Radiol Ultrasound 2002;43(1):50-53.
13. Batamuzi EK, Kristensen F. Diagnostic importance of urothelial cells of the dog and cat. J Small Anim Pract 1995;36(1):17-21.
14. LeBlanc CJ, Roberts CS, Bauer RW, et al. Firm rib mass aspirate from a dog. Vet Clin Pathol 2004;33(4):253-256.
15. Ramos-Vara JA, Miller MA, Boucher M, et al. Immunohistochemical detection of uroplakin III, cytokeratin 7, and cytokeratin 20 in canine urothelial tumors. Vet Pathol 2003;40(1):55-62.
16. Reed LT, Knapp DW, Miller MA. Cutaneous metastasis of transitional cell carcinoma in 12 dogs. Vet Pathol 2013;50(4):676-681.
17. Hume C, Seiler G, Porat-Mosenco Y, et al. Cystosonographic measurements of canine bladder tumours. Vet Comp Oncol 2010;8(2):122-126.
18. Naughton JF, Widmer WR, Constable PD, et al. Accuracy of three-dimensional and two-dimensional ultrasonography for measurement of tumor volume in dogs with transitional cell carcinoma of the urinary bladder. Am J Vet Res 2012;73(12):1919-1924.
19. Léveillé R, Biller DS, Partington BP, et al. Sonographic investigation of transitional cell carcinoma of the urinary bladder in small animals. Vet Radiol Ultrasound 1992;33(2):103-107.
20. Hanson JA, Tidwell AS. Ultrasonographic appearance of urethral transitional cell carcinoma in ten dogs. Vet Radiol Ultrasound 1996;37(4):293-299.
21. Ohtake A, Sato S, Saitoh C, et al. Effects of tamsulosin on hypogastric nerve stimulation-induced intraurethral pressure elevation in male and female dogs under anesthesia. Eur J Pharmacol 2004;497(3):327-334.
22. Ohtake A, Sato S, Sasamata M, et al. Effects of tamsulosin on resting urethral pressure and arterial blood pressure in anaesthetized female dogs. J Pharm Pharmacol 2006;58(3):345-350.
23. Sato S, Ohtake A, Hatanaka T, et al. Relationship between the functional effect of tamsulosin and its concentration in lower urinary tract tissues in dogs. Biol Pharm Bull 2007;30(3):481-486.
24. Weese JS, Blondeau JM, Boothe D, et al. Antimicrobial use guidelines for treatment of urinary tract disease in dogs and cats: antimicrobial guidelines working group of the International Society for Companion Animal Infectious Diseases. Vet Med Int 2011;2011:263768.
25. Weisse C, Berent A, Todd K, et al. Evaluation of palliative stenting for management of malignant urethral obstructions in dogs. J Am Vet Med Assoc 2006;229(2):226-234.
26. McMillan SK, Knapp DW, Ramos-Vara JA, et al. Outcome of urethral stent placement for management of urethral obstruction secondary to transitional cell carcinoma in dogs: 19 cases (2007-2010). J Am Vet Med Assoc 2012;241(12):1627-1632.
27. Blackburn AL, Berent AC, Weisse CW, et al. Evaluation of outcome following urethral stent placement for the treatment of obstructive carcinoma of the urethra in dogs: 42 cases (2004-2008). J Am Vet Med Assoc 2013;242(1):59-68.
28. Cerf DJ, Lindquist EC. Palliative ultrasound-guided endoscopic diode laser ablation of transitional cell carcinomas of the lower urinary tract in dogs. J Am Vet Med Assoc 2012;240(1):51-60.
29. Stone EA, George TF, Gilson SD, et al. Partial cystectomy for urinary bladder neoplasia: surgical technique and outcome in 11 dogs. J Small Anim Pract 1996;37(10):480-485.
30. Zhang Y, Frimberger D, Cheng EY, et al. Challenges in a larger bladder replacement with cell-seeded and unseeded small intestinal submucosa grafts in a subtotal cystectomy model. BJU Int 2006;98(5):1100-1105.
31. Peacock E. Healing and repair of peritoneum and viscera. In: Peacock E, ed. Wound repair. 3rd ed. Philadelphia: Saunders, 1984;438.
32. Stone E, Barsanti J. Urologic surgery of the dog and cat. Philadelphia: Lea and Febiger, 1992.
33. Saulnier-Troff FG, Busoni V, Hamaide A. A technique for resection of invasive tumors involving the trigone area of the bladder in dogs: preliminary results in two dogs. Vet Surg 2008;37(5):427-437.
34. Anderson WI, Dunham BM, King JM, et al. Presumptive subcutaneous surgical transplantation of a urinary bladder transitional cell carcinoma in a dog. Cornell Vet 1989;79(3):263-266.
35. Gilson SD, Stone EA. Surgically induced tumor seeding in eight dogs and two cats. J Am Vet Med Assoc 1990;196(11):1811-1815.
36. Higuchi T, Burcham GN, Childress MO, et al. Characterization and treatment of transitional cell carcinoma of the abdominal wall in dogs: 24 cases (1985-2010). J Am Vet Med Assoc 2013;242(4):499-506.
37. Beck AL, Grierson JM, Ogden DM, et al. Outcome of and complications associated with tube cystostomy in dogs and cats: 76 cases (1995-2006). J Am Vet Med Assoc 2007;230(8):1184-1189.
38. Upton ML, Tangner CH, Payton ME. Evaluation of carbon dioxide laser ablation combined with mitoxantrone and piroxicam treatment in dogs with transitional cell carcinoma. J Am Vet Med Assoc 2006;228(4):549-552.
39. Robat C, Burton J, Thamm D, et al. Retrospective evaluation of doxorubicin-piroxicam combination for the treatment of transitional cell carcinoma in dogs. J Small Anim Pract 2013;54(2):67-74.
40. Molnar T, Vajdovich P. Clinical factors determining the efficacy of urinary bladder tumour treatments in dogs: surgery, chemotherapy or both? Acta Vet Hung 2012;60(1):55-68.
41. Knapp DW, Richardson RC, Chan TC, et al. Piroxicam therapy in 34 dogs with transitional cell carcinoma of the urinary bladder. J Vet Intern Med 1994;8(4):273-278.
42. Knapp DW, Henry CJ, Widmer WR, et al. Randomized trial of cisplatin versus firocoxib versus cisplatin/firocoxib in dogs with transitional cell carcinoma of the urinary bladder. J Vet Intern Med 2013;27(1):126-133.
43. McMillan SK, Boria P, Moore GE, et al. Antitumor effects of deracoxib treatment in 26 dogs with transitional cell carcinoma of the urinary bladder. J Am Vet Med Assoc 2011;239(8):1084-1089.
44. Abbo AH, Jones DR, Masters AR, et al. Phase I clinical trial and pharmacokinetics of intravesical mitomycin C in dogs with localized transitional cell carcinoma of the urinary bladder. J Vet Intern Med 2010;24(5):1124-1130.
45. Greene SN, Lucroy MD, Greenberg CB, et al. Evaluation of cisplatin administered with piroxicam in dogs with transitional cell carcinoma of the urinary bladder. J Am Vet Med Assoc 2007;231(7):1056-1060.
46. Knapp DW, Glickman NW, Widmer WR, et al. Cisplatin versus cisplatin combined with piroxicam in a canine model of human invasive urinary bladder cancer. Cancer Chemother Pharmacol 2000;46(3):221-226.
47. Henry CJ, McCaw DL, Turnquist SE, et al. Clinical evaluation of mitoxantrone and piroxicam in a canine model of human invasive urinary bladder carcinoma. Clin Cancer Res 2003;9(2):906-911.
48. Knapp DW, McMillan SK. Tumors of the urinary system. In: Withrow SJ, Vail DM, Page RL, eds. Withrow and MacEwen's small animal clinical oncology. 5th ed. St. Louis: Saunders, 2013;572-582.
49. Mutsaers AJ, Widmer WR, Knapp DW. Canine transitional cell carcinoma. J Vet Intern Med 2003;17(2):136-144.
50. Knapp DW, Glickman NW, DeNicola DB, et al. Naturally-occurring canine transitional cell carcinoma of the urinary bladder. A relevant model of human invasive bladder cancer. Urol Oncol 2000:5(2);47-59.
51. Mitin T, Hunt D, Shipley WU, et al. Transurethral surgery and twice-daily radiation plus paclitaxel-cisplatin or fluorouracil-cisplatin with selective bladder preservation and adjuvant chemotherapy for patients with muscle invasive bladder cancer (RTOG 0233): a randomised multicentre phase 2 trial. Lancet Oncol 2013;14(9):863-872.
52. Ichinohe K, Ijima M, Usami T, et al. Complete remission of primary retroperitoneal transitional cell carcinoma after radiotherapy and oral chemotherapy: a case report. Ann R Coll Surg Engl 2013;95(2):e52-e54.
53. Jang NY, Kim IA, Byun SS, et al. Patterns of failure and prognostic factors for locoregional recurrence after radical surgery in upper urinary tract transitional cell carcinoma: implications for adjuvant radiotherapy. Urol Int 2013;90(2):202-206.
54. Zapatero A, Martin De Vidales C, Arellano R, et al. Long-term results of two prospective bladder-sparing trimodality approaches for invasive bladder cancer: neoadjuvant chemotherapy and concurrent radio-chemotherapy. Urology 2012;80(5):1056-1062.
55. Foroudi F, Pham D, Bressel M, et al. Bladder cancer radiotherapy margins: a comparison of daily alignment using skin, bone or soft tissue. Clin Oncol (R Coll Radiol) 2012;24(10):673-681.
56. Walker M, Breider M. Intraoperative radiotherapy of canine bladder cancer. Vet Radiol 1987;28(6):200-204.
57. Poirier VJ, Forrest LJ, Adams WM, et al. Piroxicam, mitoxantrone, and coarse fraction radiotherapy for the treatment of transitional cell carcinoma of the bladder in 10 dogs: a pilot study. J Am Anim Hosp Assoc 2004;40(2):131-136.
58. Nolan MW, Kogan L, Griffin LR, et al. Intensity-modulated and image-guided radiation therapy for treatment of genitourinary carcinomas in dogs. J Vet Intern Med 2012;26(4):987-995.
59. Parfitt SL, Milner RJ, Salute ME, et al. Radiosensitivity and capacity for radiation-induced sublethal damage repair of canine transitional cell carcinoma (TCC) cell lines. Vet Comp Oncol 2011;9(3):232-240.
60. Boria PA, Glickman NW, Schmidt BR, et al. Carboplatin and piroxicam therapy in 31 dogs with transitional cell carcinoma of the urinary bladder. Vet Comp Oncol 2005;3(2):73-80.
61. Schrempp DR, Childress MO, Stewart JC, et al. Metronomic administration of chlorambucil for treatment of dogs with urinary bladder transitional cell carcinoma. J Am Vet Med Assoc 2013;242(11):1534-1538.
62. Chun R, Knapp DW, Widmer WR, et al. Phase II clinical trial of carboplatin in canine transitional cell carcinoma of the urinary bladder. J Vet Intern Med 1997;11(5):279-283.
63. Chun R, Knapp DW, Widmer WR, et al. Cisplatin treatment of transitional cell carcinoma of the urinary bladder in dogs: 18 cases (1983-1993). J Am Vet Med Assoc 1996;209(9):1588-1591.
64. Arnold EJ, Childress MO, Fourez LM, et al. Clinical trial of vinblastine in dogs with transitional cell carcinoma of the urinary bladder. J Vet Intern Med 2011;25(6):1385-1390.
65. Marconato L, Zini E, Lindner D, et al. Toxic effects and antitumor response of gemcitabine in combination with piroxicam treatment in dogs with transitional cell carcinoma of the urinary bladder. J Am Vet Med Assoc 2011;238(8):1004-1010.
66. Kaye ME, Thamm DH, Weishaar K, et al. Vinorelbine rescue therapy for dogs with primary urinary bladder carcinoma. Vet Comp Oncol 2013; Epub ahead of print.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.