Difficult bacterial urinary tract infections: recurrent infections
Any time bacteria are identified, a "breakthrough" infection should be suspected.
As discussed in last month's Diagnote, protocols designed to safely and effectively eliminate urinary tract infections (UTIs) should include:
- Detection and treatment of host defense abnormalities that allow bacteria to colonize and invade the urinary tract,
- Election of appropriate antimicrobial agents to eradicate microbial pathogens,
- Monitoring response to therapy at appropriate intervals. The objective of the third part of this series is to summarize therapeutic caveats that should be considered in managing patients with recurrent bacterial UTIs.
- Why is it important to differentiate recurrent bacterial UTIs as relapses or reinfection?
Recall that recurrent bacterial UTIs that occur following withdrawal of therapy may be classified as relapses or reinfection. Relapses are defined as recurrences of UTI caused by the same species of microbe (Table 1). In this situation, remission of clinical signs and eradication of bacteria from the urine is not associated with eradication of pathogenic bacteria from tissues of the urinary tract. Relapses usually emerge within several days to a few weeks after remission of clinical manifestations of UTI; the bacteria may have become more resistant to antimicrobial agents than prior to therapy. The pathogenesis of relapsing UTI likely involves failure to completely eliminate pathogenic bacteria before antimicrobic therapy is withdrawn. Relapses represent antimicrobial treatment failures associated with one or more causes (see Table 2). Relapses have the potential to cause significant morbidity if mismanaged.
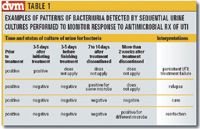
Table 1. Examples of patterns of bacteriuria detected by sequential urine cultures performed to monitor response to antimicrobial Rx of UTI
Reinfection are defined as recurrent infections caused by a different pathogen (Table 1). In this situation, bacteria have been eradicated from urine and surrounding tissue, but persistent dysfunction of one or more host defense mechanisms predisposes to infection with different uropathogens (Table 3). If superficial damage to tissues of the urinary tract induced by bacteria during the initial infection have time to heal, recurrence of clinical manifestations of reinfection often occur at a longer interval following cessation of therapy than relapses.

Table 2. Checklist of potential causes of recurrent UTIs due to relapses
Caveat: The therapeutic plan for relapses often differs from the therapeutic plan for reinfection. Therefore, it is important to compare results of bacterial culture of urine obtained prior to initiation of therapy to bacterial cultures of urine obtained during and/or after withdrawal of therapy.

Table 3. Checklist of potential causes of recurrent UTIs due to reinfection
How should relapsing UTIs be treated?
Relapse of UTI caused by the same pathogenic microbe would be expected to occur shortly after cessation of antimicrobial therapy. Therefore, the results of a urinalysis and culture should be re-evaluated approximately seven to 10 days following the discontinuation of therapy to detect recurrent relapses at a subclinical stage. Recovery of the same organism from urine that was sterile during anti-microbial therapy is presumptive evidence that antimicrobial therapy failed to eradicate the infection from adjacent tissue, and suggests lack of compliance with treatment recommendations, or deep-seated infection (Tables 2 and 4). If diagnostic efforts to find a predisposing cause have not yet been performed, they should be considered as essential at this time (Table 2).

Table 4. Checklist of compliance problems and solutions
If the relapse occurred following a brief period of therapy, continue treatment for a longer period. If the relapse occurred 10 or more days following therapy, repeat therapy with a different antimicrobial agent selected on the basis of susceptibility tests. Then, continue therapy for a longer period (three to four weeks). The procedures to evaluate treatment efficacy described above should be repeated.
Caveat: Relapses are indicative of antimicrobic treatment failure, and are of considerable significance in terms of potential morbidity. Special consideration should be given to the likelihood that the drug selected will reach therapeutic concentrations at the site of infection in the urinary tract.
How should UTIs caused by reinfection be treated?
Provided the urinary tract has had sufficient time to repair damaged tissues, reinfection caused by different pathogenic microbes would be expected to occur later following discontinuation of treatment than a relapse (Table 1). Therefore the results of a urinalysis and culture should be re-evaluated approximately two to three weeks after cessation of antimicrobial therapy.
Detection of frequent reinfection following antimicrobial therapy warrants evaluation of the patient for one or more predisposing causes (Table 3). The goal is to correct the predisposing cause. reinfection should be managed by choosing antimicrobial agents on the basis of antimicrobial susceptibility tests. Each product should be used for a sufficient period of time (three to five days) to evaluate its effectiveness in sterilizing urine.
Caveat: Elimination of bacterial pathogens associated with reinfection may require therapy of shorter duration (10 to 14 days) than recurrences associated with relapses. In fact, treatment of reinfection with therapeutic doses of antibiotics for long periods is usually not warranted. Why? Because, when recurrences due to reinfection occur the antimicrobial drugs are effectively eradicating bacterial pathogens. Infrequent reinfection (two or three times per year) may be treated as single episodes (i.e. short course of a suitable antimicrobial agent).
How can frequent reinfection be minimized?
In some patients with recurrent UTIs, it may be impossible to identify and/or correct underlying disorders in host defenses that permit bacteria to infect the urinary tract (Table 3). The result is often frequent reinfection. In such cases it may be helpful to provide low-dose (so-called preventative) antibacterial therapy for six months or more with bacteriocidal drugs primarily eliminated in urine.
Drugs that have been used for this purpose include amoxicillin, ampicillin cephalexin and trimethoprim-sulfadiazine. Consider selection of drugs to use for preventative therapy on the basis of results of the most recent antimicrobial susceptibility test. Reduced dosages (about one-third to one-half of the therapeutic dosage) of drugs excreted in high concentration in urine may be used provided there has been complete eradication of bacterial pathogens by therapeutic dosages of appropriate drugs. Logically, low-dose preventive antimicrobial therapy would be inappropriate for management of patients with recurrent bacterial UTI due to relapses, since they have persistent infection.
It is best to give one daily preventive dose of the antibiotic at a time when the drug is likely to be retained in the urinary tract for six to eight hours (for example, prior to bedtime). Even though this preventive dosage regimen does not result in MICs throughout the day, low concentrations of some drugs augment innate host defenses.
In some patients, this strategy appears to interfere with production of fimbriae by some uropathogens. This in turn interferes with the ability of potential pathogens to adhere to and colonize uroepithial cells.
During preventative therapy, urine samples collected by cystocentesis should be recultured at appropriate intervals (so-called surveillance cultures). Samples should not be collected by catheterization, as catheters may cause iatrogenic infection. Urine samples should not be collected by voiding as it may be impossible to distinguish bacterial contaminants in voided samples from pathogens.
Surveillance cultures of urine for bacteria should be performed at shorter intervals initially (after first week of treatment and, if sterile, after the fourth week of treatment). If there are no signs of bacteria-induced urinary tract disease, and the urine is sterile, surveillance intervals may be extended to every eight to 12 weeks.
Any time bacteria are identified, a "breakthrough" infection should be suspected. Recurrences during prophylactic therapy may be associated with poor compliance (Table 4).
Compare bacterial culture results to previous bacterial isolates to determine whether a relapse or reinfection has occurred. The recurrent infection should be treated for an appropriate period with therapeutic dosages (so-called "full dose") of an antimicrobial drug selected on the basis of susceptibility tests. Once the infection has been eradicated and the associated inflammatory response subsides, preventative therapy may be resumed.
Following six to nine months of consecutive negative urine cultures and urinalysis results indicating that the host defenses are functioning adequately, therapy may be discontinued on a trial basis to determine if re-infection will occur. If abnormalities in host defenses have healed, UTI may not recur. If UTI develops within a short period, the procedures outlined above should be repeated.
Caveat: Bacterial infections should be eradicated from the urinary tract prior to prophylactic therapy. Therefore, low-dose preventative antimicrobial therapy would be inappropriate for management of patients with recurrent bacterial UTI due to relapses since by definition viable bacteria are still present in the urinary tract.
Dr. Osborne, a diplomate of the American College of Veterinary Internal Medicine, is professor of medicine in the Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Minnesota.