Got a pyoderma? Step away from the systemics
At least until you know you need them, that is. For bacterial overgrowth and superficial cases, topical therapy may be all you need for your veterinary patients.
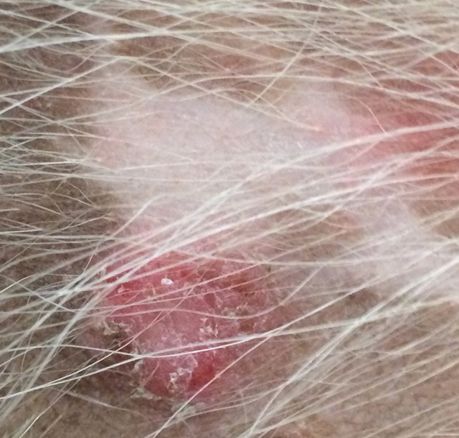
This ventral neck lesion shows erythema, alopecia, scale and lichenification. Cytologic examination showed a mixed bacterial overgrowth. Image copyright Dr. Craig Griffin.

Pyoderma is a straightforward bacterial overgrowth on the skin-or is it? Craig Griffin, DVM, DACVD, of Animal Dermatology Clinic in San Diego and a recent CVC speaker, maintains that while bacterial overgrowth on the skin can lead to pyoderma, they are not the same thing and should be treated differently. Furthermore, pyoderma in adult dogs is a progressive disease perpetuated by a long list of factors. If you don't address those factors, you're staring down the barrel of recurrent pyoderma or antibiotic resistance.
The predominant pathogen that causes pyoderma is Staphylococcus pseudintermedius, an overgrowth of normal flora that resides on the mucosal surfaces and hair coats of dogs. Staphylococcus schleiferi, Escherichia coli, and Cornynebacterium, Enterococcus and Pseudomonas species have also been identified on culture in dogs with pyoderma. But no matter the pathogen, clinical presentation is usually the same, Dr. Griffin says.
The medical definition of pyoderma is a bacterial skin inflammation marked by pus-filled lesions. So in order to call it pyoderma, you have to have pus, Dr. Griffin says. The classic lesions of pyoderma are pustules, furuncles, fistulas, crusts, papules, nodules and epidermal collarettes, though lichenification may also be a lesion of pyoderma. Diagnosis is confirmed with cytologic examination of the skin that shows neutrophils with bacteria, preferably intracellular.
In contrast, if you have a dog with red, itchy, dry skin and a preponderance of bacteria but no neutrophils, then you have a bacterial overgrowth. Because of concerns surrounding methicillin-resistant Staphylococcus (MRS) species, Dr. Griffin recommends that the treatment for bacterial overgrowth without evidence of inflammation differ from the classic pyoderma treatment.
Pustules, papules and crusts in a dog with bacterial folliculitis. Image copyright Dr. Craig Griffin.

Papule crusts and epidermal collarette in a dog with bacterial folliculitis. Image copyright Dr. Craig Griffin.
Hemorrhagic furuncles in a dog with folliculitis (note the surrounding erythematous papules) and furunculosis where the follicles have ruptured deeper in the dermis. Image copyright Dr. Craig Griffin.

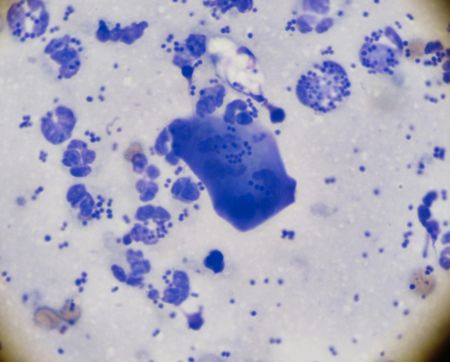
Cytology of superficial pyoderma with cocci and numerous neturophils most contain phagocytized intracellular cocci. The center large blue keratinocyte is present.
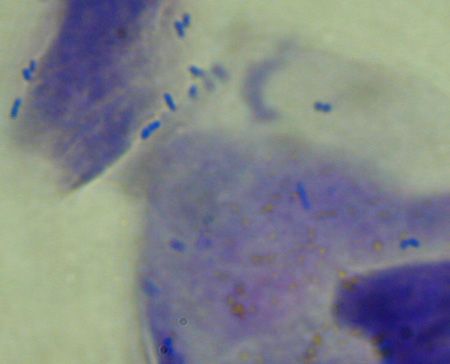
Bacterial overgrowth with lack of neutrophils but more bacterial rods than would be present on normal skin. Some cocci are also present. Image copyright Dr. Craig Griffin.
Predisposing and perpetuating factors
Veterinarians are well-versed in predisposing conditions such as atopy, obesity, endocrine disorders, inappropriate friction, pressure (callus) and alteration in skin microenvironment from traits such as skin folds-all factors that make a dog more likely to develop pyoderma. Drugs such as corticosteroids may also have an impact, Dr. Griffin suggests.
Perpetuating factors are pathologic changes in the skin due to pyoderma that make the condition more likely to continue. Folliculitis, common in pyoderma, often results in foci of alopecia, exposing the skin to ultraviolet radiation. That radiation or keratin released from follicular rupture may affect the local immune response, the hair follicle structure or cutaneous inflammation, Dr. Griffin says. Another perpetuating factor is fibrosis, which may be less apparent unless it occurs grossly. Perifollicular fibrosis often occurs at the microscopic level, and certain breeds (Doberman pinschers, bull and Staffordshire terriers, rottweilers) seem predisposed to excessive scarring that makes resolution of pyoderma more difficult. Perform a biopsy to identify scarring in these patients.
Dr. Griffin suggests that pyoderma may be a perpetuating factor in itself. He believes that the longer a dog has pyoderma, the more altered the skin barrier becomes and the harder the infection becomes to control. So does the presence of pyoderma result in changes that perpetuate the development of chronic inflammation, leading to more pyoderma? Some clinical observations support this theory, but studies are needed for definitive answers, Dr. Griffin says.
Treatment plan: A better way
Historically, canine pyoderma was treated using antibiotics chosen empirically and some topical therapy. This approach is no longer always appropriate or even reliable, Dr. Griffin says, especially in regions of the world areas where methicillin and multidrug Staphylococci resistance is becoming more common. One way veterinarians can fight the development of resistant bacterial infections is to adopt new approaches to treating bacterial overgrowth and pyoderma, Dr. Griffin says.
Superficial cases. For bacterial overgrowth, localized pyoderma or mild lesions, or to prevent recurrence of pyoderma while you're pursuing diagnostics for underlying conditions, Dr. Griffin says topical therapy alone-without systemic antibiotic therapy-is an appropriate approach.
Multiple studies have shown that topical therapy alone may resolve pyoderma, including cases involving methicillin-resistant Staphylococcus pseudintermedius (MRSP). More than 50% of these patients can have their infections eliminated, with the most success reported with chlorhexidine-containing shampoos.1-3
In one study, treatment with topical 4% chlorhexidine products showed resolution of clinical signs in all dogs and was found to be as effective in treating superficial pyoderma as systemic therapy with amoxicillin-clavulanic acid.4 Dr. Griffin recommends using topical products containing 3% or higher chlorhexidine with standalone products, or 2% or higher in combination products.
Think your clients will balk? Hear us out
Before you walk away from this article in disgust muttering, “There is no way my 86-year-old client is going to bathe a 75-pound dog daily,” I exhort you: keep an open mind.
Yes, your clients are likely to tell you that bathing is stressful for all parties involved, and their bathing facilities may be limited. However, if you explain why you're telling them to bathe their dogs (to minimize the development of resistant bacteria and reduce impact to the rest of the body) and how it benefits their pets (speeds healing, decreases the amount of time systemic microbials must be used, removes nasty crusts and makes the hair look healthier), I have found that nine times out of 10 pet owners get it. What's more, they actually do it!
A recent study suggests that, depending on the formulation, residual antibacterial activity can last for a week after an animal is bathed with 2% or 3% chlorhexidine shampoo.1 Depending on the shampoo formulation, hair length, severity of disease, and perpetuating factors, the client may only need to bathe the dog twice a week.
Teaching owners to catch when their dogs have bacterial overgrowth on their skin will reduce the development of pyoderma and perpetuating factors, leading to healthier patients and happier clients.
Reference
1. Kloos I, Straubinger RK, Werckenthin C, et al. Residual antibacterial activity of dog hairs after therapy with antimicrobial shampoos. Vet Dermatol 2013;24(2):250-e54.
Cleaning the skin promotes desquamation, which removes surface bacteria and yeast as well as irritants and allergens, normalizes keratinization, and can improve barrier function. Anti-inflammatory ingredients or even just cool water can also be used to help decrease inflammation. Moisturizing and cooling the skin will also decrease pruritus. In general, Dr. Griffin recommends bathing the pet frequently-every other day is preferred though some cases do respond to twice-weekly bathing, especially if topical antiseptic sprays are used between baths. Two times a week is generally effective in preventing recurrent pyoderma and bacterial overgrowth. Daily bathing is required in some cases for complete resolution.
Have a patient with chronic or recurrent bacterial overgrowth secondary to poorly controlled perpetuating factors? Dr. Griffin advises teaching your client to recognize the signs of bacterial overgrowth (mainly odor and possibly red skin, scaling or pruritus) and instructing them to bathe the dog with an antiseptic shampoo before pyoderma develops-or give a standing order to bathe the dog weekly.
Profound cases. Systemic antibiotic therapy is required to treat deep pyoderma, some recurrent pyoderma and pyoderma with perpetuating factors; it's also necessary in cases of poor or non-existent compliance with topical therapies. Here are some guidelines:
> Combine systemic with topical therapy where possible.
> Choose antibiotics based on impression cytology, along with the results of culture and sensitivity testing.
> Keep in mind that most pyoderma therapy should be instituted for at least three to four weeks. If you're using topical therapy as well, use your judgment about whether to decrease the duration of systemic therapy.
When designing a treatment plan for both pyoderma and bacterial overgrowth, Dr. Griffin says, you must identify, reverse or control any perpetuating factors, or your chance of success is limited-and the chance of an irritated client is high. Recurrent or chronic pyoderma? Time to go hunting for perpetuating factors as well as predisposing factors.
Some treatments may need to be directed at reversing pathologic changes in the skin, or the patient may require long-term therapy until the body naturally remodels or reverses those changes. You may need to consider surgical removal of localized fibrotic or granulomatous lesions. Long-term pentoxifylline may help reverse scarring in cases with widespread lesions not amenable to surgical therapy, Dr. Griffin says. Glucocorticoids have been used in some cases with residual granulomas, but Dr. Griffin recommends corticosteroids be used only after antibiotic therapy has eliminated the bacteria and the granulomas are sterile based on culture. The sooner you stop and control perpetuating factors, the better the dog will be long term.
References
- Bryan J, Frank LA, Rohrbach BW, et al. Treatment outcome of dogs with methicillin-resistant and methicillin-susceptible Staphylococcus pseudintermedius pyoderma. Vet Dermatol 2012;23(4):361-e365.
- Loeffler A, Cobb MA, Bond R. Comparison of a chlorhexidine and a benzoyl peroxide shampoo as sole treatment in canine superficial pyoderma. Vet Rec 2011;169(10):249-254.
- Murayama N, Nagata M, Terada Y, et al. Efficacy of a surgical scrub including 2% chlorhexidine acetate for canine superficial pyoderma. Vet Dermatol 2010;21(6):586-592.
- Borio S, Colombo S, La Rosa G, et al. Effectiveness of a combined (4% chlorhexidine digluconate shampoo and solution) protocol in MRS and non-MRS canine superficial pyoderma: A randomized, blinded, antibiotic-controlled study. Vet Dermatol 2015;26(5):339-344.