MRSA, biosecurity and more (Proceedings)
All antibiotics select for resistance ... you look for it, you find it.
Basic comments about AB resistance
- All antibiotics select for resistance...you look for it- you find it....
- Antibiotics used in animal health just like all AB's
- AB resistance poses threat to human health
- Many factors that contribute to emergence and dissemination of antibiotic resistance
- Not possible to quantify 'attributable risk' for any of the complex factors that contribute to resistance
Microbes of resistance concern in horses
- Salmonella [3rd generation cephalosporins, fluoroquinolones]
- E. coli [same as above]
- Enterococci [ fluoroquinolones, gentamicin, vancomycin, macrolides]
- MRSA [3rd generation cephlosporins, fluoroquinolones, macrolides]
Factors that increase resistance
- Inadequate dosing
- Indiscriminate use of antibiotics
- Inadequate duration of therapy
- Noncompliant owners
- Close physical contact between horses & owners
- Public awareness- increasing attention in literature
- Evidence of bidirectional transfer
- Strong evidence of carrier states for both pets and humans
- MRSAs documented to arise from both human and veterinary hospitals

Patient file

Veterinary Microbiology
Salmonella
Gram-negative, flagellated facultatively anaerobic bacilli
Possessing 3 major antigens:
* H (flagellar): phase 1/phase 2
* O (somatic): surface of outer membrane, determined by specific sugar sequences on cell surface
* Vi : superficial antigen overlying the O antigen, present in only a few serovars (S typhi)
- Cell envelope contains complex LPS
- 2449 serotypes
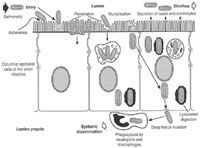
Pathogenesis
Pathogenesis:
1) ability to invade cells
2) complete LPS coat
3) ability to replicate intracellularly
4) elaboration of toxin(s)
Methicillin-Resistant Staphylococcus aureus (MRSA) in Horses
- Most important hospital associated pathogen in human medicine
- Increasingly reported in animals
- MRSA infection of horses + horse personnel is emerging problem
- Disease can occur in either species and interspecies transmission propagates MRSA
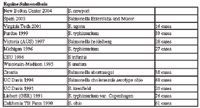
Equine Salmonellosis
MRSA Background
- S.aureus- commensal microbe in humans- considered 'normal' microflora of skin, nares...
- Long recognized as opportunistic pathogen w/ dz's ranging from superficial soft-tissue to bacteremia and toxic shock syndrome
- Commensal microflora not well understood in horses- nasal colonization of S.aureus occurs in + 7% of horses
- Resistance result from B-lactamase- thus development of methicillin- microbes now resistant to this class of AB's. MRSA emerged in 1960's
Emergence & Diagnosis of MRSA
- ID of S.aureus straightforward- ID of MRSA requires more testing (3-7days)
- MRSA infection in horses first in 1990's- post-op wound infection in vet hospital.
- Several strains and have adapted to survive in horses
- Concern over transmission of MRSA between horses and people
MRSA risk factors
- Recent contact with health care system
- Admission to long-term care facility
- Hospitalization- ICU
- Surgery
- Antimicrobial tx- (fluoroquinolones)
- Immunosuppression + debilitating dz
- Administration of ceftiofur or aminoglycosides also reported
Treatment and Management
- Currently no objective information regarding management of clinical MRSA in veterinary species
- No indication that antimicrobial therapy useful for decolonizing horses (increased risk of AB resistance)
MRSA in horse personnel
- High prevalence of MRSA colonization in horse farm personnel – 13% (Weese et al)
- 1 colonized person on each farm with colonized horse
- Zoonotic MRSA reported- Very disturbing!
- Study at 2005 ACVIM meeting (417 tested) 3.8% small animal vets, 13.8% large animals colonized...84.6% of large animal vets carried horse-associated MRSA
Biosecurity at VTH
- SOP's established and strictly adhered to;
- "Yellow Dot" status is reserved for patients at high risk for acquiring infections due to poor immune status. The biosecurity status may be changed to "green dot" as the patient's condition improves.
- Examples: critically ill, immuno-compromised, unvaccinated (non-infectious, neonatal animals < 30d of age), Failure-of-passive-transfer foals, neonatal patients or those requiring intensive care.
- "Green Dot" Status is reserved for patients with no historical, physical or laboratory evidence of contagious disease.
- Examples: Patients presenting for elective surgical procedures, non-infectious disease work-ups, minor trauma, or ancillary diagnostics.
- "Blue dot" status is reserved for animals demonstrating undifferentiated neurological signs that are not considered to be contagious.
- Examples: Equine protozoal myelopathy (EPM), neurologic (non-repiratory) EHV-1, wobblers, animals for which rabies is being considered as a differential.
- "Orange Dot" status is reserved for patients with infectious diseases that are considered to be mildly or moderately contagious to other patients or personnel.
- Examples: Animals originating from a farm with a history of salmonellosis but that have not individually tested positive or that lack GI signs, those for which infectious disease is being considered as a differential, horses that continually reflux but do not exhibit a fever, leukopenia or diarrhea.
- "Red Dot" status is reserved for patients known or suspected to have highly contagious diseases. Patients should be placed directly into LA-ISO after being examined.
- Examples: Patients with a previous history of salmonellosis, those exhibiting clinical signs which include a fever, leukopenia, and/or diarrhea, Other equine examples: strangles, cryptosporidiosis. Food / fiber animal examples: salmonellosis, tuberculosis, Johne's disease, cryptosporidiosis, all calves with diarrhea, caseous lymphadenitis.
Minimizing Antimicrobial Resistance
- Awareness that compliance with prescribed regimens is critical!
- Looking beyond clinical resolution (microbiological cure if possible)
- Looking beyond specific patient to future population
- Coordination between health care professionals (vet and human)
- Attention to nursing, husbandry, animal-human contact and movement