Separation anxiety: The worry over worry
How to handle varied levels of investment in alleviating this common veterinary behavior problem.

(Getty Images)You've just finished your annual visit appointment, and the dog's owner begins with an “Oh, by the way” line. You know what's coming, yet your mind is swimming with the string of appointments waiting as well as medications that need to be made up for the last client, and there is an emergency call you have to take. Now this person wants you to cure his or her dog of what seems like separation anxiety in the one minute you have left for the visit. What you say next depends on many things, including the emotional and financial investment the owner puts in the pet.
In my opinion, it is in the patient's best interest for veterinarians to first offer what they think is the best approach to treating any condition, and this includes behavioral issues. Alternative strategies can be presented if the client thinks the ideal approach is not a direction that they can pursue. It would be wrong for a veterinarian to assume what the client will choose ahead of time. We cannot predict or anticipate-nor should we-what a person's level of attachment or financial investment would be with a particular patient at a particular point in time.
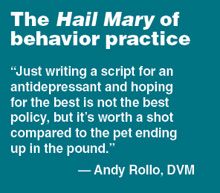
However, if it is a situation in which there is not adequate time to manage a behavior problem presented by a client, such as when the issue is presented at the end of an annual visit, there is nothing wrong with a veterinarian suggesting a treatment option that does not involve a lot of time to explain or risk to the patient. This would be an ideal time to recommend a nutraceutical or pheromone product. It is IMPERATIVE in these instances that the veterinarian explain that there are other options as well and these can be explored in more depth during a scheduled behavior visit.
My recommended separation anxiety treatment plans
1. The best option: “I'm all in!”
Perform a full physical examination.
Perform laboratory testing, including a complete blood count (CBC), serum chemistry profile, thyroid profile and urinalysis, as well as additional testing if indicated by the initial test results.
Start behavior modification immediately. Have the client ignore the pet's attempts to solicit attention since anxious dogs often use person contact to manage anxiety, and this strategy is not available to the pet when it is away from the owner. All contact should be on the owner's initiative.
No interactions should occur between the owner and pet for 30 minutes before departure to help the pet adapt to the owner not being present. The only exception would be the presentation of a treat-dispensing device or other long-lasting treat at the time of departure to keep the pet's attention during the departure.
To reinforce relaxed behavior, the owner should ignore the dog when arriving at home until the pet is relaxed.
The owner should habituate the pet to departure cues. This involves performing any departure activities that the pet seems to show increased anxiety over at times when the owner has no intention of leaving so that these activities do not serve as a reliable predictor of departures.
Implement independence training, which involves teaching the dog to remain in a resting area while the owner gradually leaves the room and reinforces relaxed behavior. This often involves using a mat or bed for the dog to remain on during these exercises.
Implement graduated departures from the home. This involves the owner gradually increasing the time of departure from the home while reinforcing relaxed behavior as he or she returns. The owner may begin by just moving to the door, then gradually opening the door, then leaving for a few seconds and gradually increasing this time. Usually the goal is to be gone for two hours with a relaxed response by the dog. At this point, most patients can be left for more normal periods. In addition, the owner often has to use a bridge cue to indicate to the dog that these departures are practice departures (such as using a visual indicator like a light or an olfactory one like a room freshening spray). Later, this cue can be used when the dog is ready for an actual departure to help with the transition.
Note: I typically only do graduated departures if there is a failure to respond to the initial treatment plan. This can be a complicated and tedious process for the owner to perform, and there is good evidence to show that if too many items are included with the initial treatment plan, many owners get overwhelmed and fail to follow through on the overall plan.
Prescribe anti-anxiety medications. There are a few options here, and primarily I would start with either an selective serotonin reuptake inhibitor (SSRI) such as fluoxetine or a tricyclic antidepressant such as clomipramine. Additional medications can be added if needed such as trazodone. If you prescribe medication, be sure to perform a follow-up CBC and serum chemistry profile six to eight weeks after beginning the medication.
It is a great idea to have the owner videotape the dog when alone to help confirm the diagnosis as well as to monitor progress.
2. Next option: “Whoa, doc! That's a lot of steps!”
As always, making a diagnosis is critical to treatment. Regardless of what is decided as to treatment options, you must verify the diagnosis. Thus, gathering a patient history is vital. Ask:
• Who-Who is present when the behavior is occurring. Is the dog truly alone or perceiving that it is alone? Or does the dog readily have access to the primary attachment figure?
• What-What behaviors are being seen or found?
• When-When is the behavior occurring? When the dog is alone, or not? And during what type of departures, such as during the week or weekends, work departures or in the evening when the owner has to go out again?
• Where-Where is the damage or elimination occurring in the house? Near exit points, which can indicate a need to reconnect or a need to get to the elimination area outside that door? Scattered about the house, which can occur when a dog is frantic? Or is there a mess of stool or urine in a consistent area suggesting a housesoiling issue? Again, video is very helpful here to confirm the diagnosis.
If you've established a diagnosis of separation anxiety but the owner cannot invest the time or resources into the full treatment plan, keep the behavior suggestions simple.
First, change the departure and arrival routine as outlined above. I feel this is the single most helpful piece of behavioral advice you can give.
Second, try to extinguish the anxious response to departure cues by using the advice to habituate to departure cues.
Prescribe anti-anxiety medication. Be sure to perform laboratory work before and after initiating treatment.
3. Next option: “Just the basics please, doc.”
Your first goal is do no harm, and your second is to let clients know there are other options if the following suggestions fail to be helpful.
Have clients videotape the dog to get an idea what is going on and, if the initial treatment plan is not helpful, to determine if in fact this is really separation anxiety you are dealing with.
Recommend neutraceuticals (such as L-theanine, tryptophan, alpha-casozepine or melatonin) or appeasing pheromones or a ThunderShirt (ThunderWorks) or Anxiety Wrap (The Company of Animals).
Recommend herbal remedies such as Bach flower or lavender.
I prefer to think of these options in the same way I think of the use of antihistamines for the management of atopy. Most of the time, they are not helpful. However, they are easy to try, safe and, in a small percentage of dogs, can be helpful. Also, as in managing atopy, it is often a combination of items that ultimately proves to be helpful and not a single medication or behavior modification step.
And, finally, COMMUNICATE with your clients. How will you know what works unless you ask? Behavior is about management, not cure. It also shows you care about the progress your patient is making. And, in the end, that's what really makes veterinarians the best doctors on the face of the planet!
John Ciribassi, DVM, DACVB
Chicagoland Veterinary Behavior Consultants