Surgical oncology and pathology for the private practitioner
Bone aspirates are becoming increasingly more useful in diagnosis of ... bone lesions. needed
Surgery still remains one of the most effective options for the treatment of solid malignancies in dogs and cats. A wide excision either alone or in combination with adjuvant radiation therapy can be "curative" for malignancies that are locally invasive.
However, in order to optimize the results of surgery, there are a number of issues that need to be addressed for each patient, such as pre-surgical biopsies, pre-surgical imaging, surgical technique, biopsy submission and post-operative adjuvant therapy.
To biopsy or not to biopsy
Benign tumors can have a similar gross appearance to those that are malignant but have a completely different biologic behavior. Features of malignancy include local invasion and the potential for metastasis, both of which can significantly change the treatment plan as well as the prognosis. Locally invasive tumors such as soft-tissue sarcomas will require a much more aggressive resection, as well as adjuvant radiation therapy. Tumors that have a high metastatic potential may require adjuvant chemotherapy as well. In addition, systemic cancers can present with localized lesions and may best be treated with chemotherapy and/or other systemic therapies. Some owners may be less inclined to pursue treatment for those tumors that have a poor prognosis or that would require radiation therapy and/or chemotherapy following surgery. Being able to advise owners in regards to the extent of surgery and the potential for adjuvant therapies can help avoid unpleasant surprises.
All tumors should be considered potentially malignant. A pre-surgical diagnosis via aspirate or an incisional biopsy is highly recommended in most cases prior to definitive excision. Exceptions to this rule would be when the biopsy procedure is as risky as a definitive surgery or if the biopsy procedure would potentially jeopardize the chances of a successful surgical excision. From time to time there are lesions that cannot be definitively diagnosed via cytology or an incisional biopsy due to large areas of necrosis or inflammation. In these cases, an excisional biopsy may be required for a definitive diagnosis.
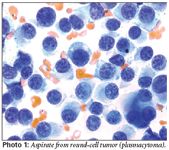
Round-cell tumors and carcinomas generally exfoliate well, so cytology is generally adequate in making a diagnosis for these tumors (Photos 1 and 2). Sarcomas do not always exfoliate well so an incisional biopsy may be required to diagnosis these tumors (Photo 3). If there is significant inflammation within a tumor, it may not be possible to determine if it is malignant or benign, given that reactive cells can have features that are suggestive of malignancy (Photo 4). There is the potential that lesions that appear to be benign on cytology are found to be malignant once removed. A common example of this is a mammary-gland tumor, so removal of any mammary mass is recommended regardless of the cytology results. Tumors that are growing rapidly or changing in appearance also should be removed despite a benign-appearing cytology.
Bone aspirates are becoming increasingly more useful in the diagnosis of lytic and proliferative bone lesions. An aspirate is less invasive, less painful, can be done on an outpatient basis and has a lower risk of fracture. In most cases, the only equipment required for an aspirate would be a 19G or 20G needle, a 10 cc syringe and a local anesthetic. Given the significant lysis associated with most bone lesions, it is not difficult to find a soft area for an aspirate. Ultrasound can be used to find a weak area in the cortex if there is still healthy bone present.
Bone cytology appears to have a high specificity for bone neoplasia, meaning that if a diagnosis of a malignancy is made, the diagnosis is likely to be accurate. However, if the sample is non-diagnostic or yields a reactive process, one should still consider the potential for neoplasia. If neoplasia is still suspected, then an alternative method of biopsy should be considered.

There are several ways to obtain an incisional biopsy, including a Tru-cut biopsy, punch biopsy or wedge biopsy. As would be expected, the larger the sample the pathologist receives, the more likely that the diagnosis will be accurate. In many cases, a Tru-Cut biopsy or a punch biopsy (Photo 6) can be done as an outpatient procedure with local anesthesia or light sedation.
Incorrectly performed biopsies can jeopardize the success of surgery.
It is important to orient the incision and biopsy tract in such a way that it can be excised with a definitive surgery.
Attention to hemostasis is also critical, because tumor cells can migrate into the surrounding tissues with blood.
Sizing up the tumor
Pre-surgical imaging has been discussed in previous articles on soft-tissue sarcomas and oral tumors.
The success or failure of a surgical procedure can be based on the ability to accurately determine the extent of the tumor prior to surgery.
For example, a hemipelvectomy may be required rather than a simple coxo-femoral disarticulation for those tumors that encroach upon the pelvis. There are those tumors where the visible disease is only a small portion of the tumor and knowledge of the tumor extent can predict an unsuccessful surgical procedure prior to surgery. In cases like these, it may be more appropriate to consider pre-operative radiation therapy or chemotherapy to see if the tumor can be downsized or consider palliative options instead.

Pre-operative staging would depend on the histologic tumor type. An aggressive surgery may not be for those patients that have metastatic disease at diagnosis. A CBC and chemistry profile should part of the routine pre-anesthetic screening. Three views of the thorax should be obtained in all patients suspected of having a malignant tumor prior to surgery. The only exceptions to this rule would be for some of the round-cell tumors such as mast-cell tumors that only rarely metastasize to the lung. It still is appropriate to obtain thoracic radiographs for all patients as a pre-anesthetic screen and to rule out other significant conditions.
Abdominal ultrasound should be considered part of the staging for those tumors that are likely to metastasize to regional lymph nodes (i.e. anal sac tumors) or for suspected round-cell tumors that are more likely to metastasize to the spleen or liver.
Lymph-node aspirates should be obtained for those tumors that commonly metastasize to lymph nodes or when there is lymph-node enlargement. If there is a concern for lymph-node metastasis, the lymph node can be removed either prior to or at the time of a definitive surgery.

Suggested Reading
Options for tumor imaging include radiographs, CT and MRI. Radiographs can be useful in determining the extent of bone involvement but are not good for soft-tissue imaging. There are limitations to radiographs even when imaging bone. Keep in mind there needs to be 50-percent bone loss prior to being able to visualize this on a radiograph. With the advent of CT and MRI, the role of radiographs in surgical planning has become limited. One indication would be the use of dental radiographs for evaluation of smaller oral tumors.
CT and MRI have become valuable tools for surgical planning. Information that can be obtained includes the extent of the tumor, involvement or proximity of normal tissues, the extent of margins that can be obtained and the presence of metastatic disease.
CT is used most commonly because it is more readily accessible and less expensive. CT is superior to MRI when evaluation of bone is needed. MRI's strengths are in evaluating soft-tissue involvement. MRI also is considered superior when evaluating lesions in the CNS. If not accessible, CT can still provide the necessary information for surgical planning.
Dr. Cronin earned her DVM degree from Cornell University in 1990. She completed an internship at the Animal Medical Center in New York and a medical oncology residency at North Carolina State University. She is a diplomate of the American College of Veterinary Internal Medicine in the specialty of oncology. After completing her residency, she was lecturer at the University of Pennsylvania Veterinary Teaching Hospital and a medical oncologist at Angell Memorial Animal Hospital in Boston. In 2001, she co-founded the New England Veterinary Oncology Group in Waltham, Mass.