Talking to clients about Cushing's
Use these communication techniques to talk about a chronic but treatable disease like Cushing's.
Chronic diseases like hyperadrenocorticism can be hard for owners of afflicted dogs to swallow. Veterinary Economics Editorial Advisory Board member Jim Kramer, DVM, CVPM, has seen those client worries firsthand.
"There's fear, loss, loathing and grief with anything that can't be cured, akin to cancer," says Dr. Kramer, owner of Columbus Animal Hospital in Columbus, Nebraska.
Benchmark your diagnosticsWe talked to one dog owner, however, who found comfort in her veterinarian's diagnosis. The phrase that turned her fear of a disease she'd never heard of into hope for the future was "chronic but treatable."
"That was reassuring," she says. "Even though Cushing's disease wasn't the best thing in the world, we could deal with it."
Ultimately, it's up to you and your team to communicate about Cushing's disease and other adrenal conditions in a way that eases clients' minds and helps them confront their fears about the pet's future.
Seeing signs
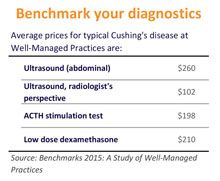
“In our hospital, when an animal has indications that make us think Cushing's is a reasonable possibility, we use the Low Dose Dexamethasone Suppression (LDDS) test to diagnose typical Cushing's disease,” Dr. Kramer says. Along with LDDS, they will often also do ultrasound evaluations of the adrenal glands.
The reality of Cushing's can be tough. Early signs may push loving but frustrated clients to rehome their dog.
The reality of Cushing's disease can be tough on pet owners. Early signs may push loving but frustrated clients to contemplate finding the dog a new home. "The dog urinates all over the house. It may be losing its hair," Dr. Kramer says. "The human-animal relationship can start to erode."
A helping hand
You empathize with your clients' struggles to remember to give medications for Cushing's disease and other ailments-and we do, too. So our art director, whose Dalmatian lived many years with Cushing's disease, designed customizable daily and weekly reminder checklists for your clients. Click here to download a PDF version of these handouts.
However, if clients have observed the signs that something's amiss, they're more likely to comply with your diagnostic recommendations. "By the time we're testing for Cushing's disease, which usually affects older dogs, most clients have already approved testing for other problems," Dr. Kramer says. "They've got some investment in solving the dog's problems."
Of course, a Cushing's diagnosis isn't the easy answer these pet owners are looking for. "They want it to be something simple, something that doesn't take continual treatment for the rest of the dog's life," he says. That's where repeating the mantra of "chronic but treatable" can be helpful, Dr. Kramer says.
Not seeing signs
But what if the unsettling physical changes don't appear? Another Veterinary Economics Editorial Advisory board member, Andrew Rollo, DVM, says this is the flip side of the disease.
"Clients can be in denial because their dog doesn't show the typical signs, like a pot belly," says Dr. Rollo, an associate at Madison Veterinary Hospital in Madison Heights, Michigan. "They don't appreciate the urgency of testing for Cushing's disease even when we see a steadily increasing ALP activity."
If the LDDS testing shows normal results, testing for what Dr. Kramer calls “Atypical Cushing's” commences, which requires more tests as well as more money. To keep the element of surprise out of the equation, Dr. Kramer explains Atypical Cushing's to pet owners before LDDS testing so they're prepared for it to at least be a possibility.
Diagnosing by process of elimination is often medically crucial but difficult to explain to pet owners.
Diagnosing by process of elimination is often medically crucial but sometimes difficult to explain to pet owners. "When a client finally gives the OK for the LDDS test, we have to tell them it may not give a definitive answer," Dr. Rollo says. "If it doesn't, we'll need to run the more expensive ACTH stimulation test. Will we be done then? Maybe not. Then we may have to ultrasound the adrenal glands and then run the ACTH test again 10 days after we start drug treatment."
Because a diagnosis can be difficult to pin down, Dr. Kramer tries to overcome clients' resistance to diagnostics with an effort to get the right answer. "Our clients sacrifice to care for their animals. We know that. And the best and least-expensive way to proceed is to get the right answer with the right tests," he says. Build that trust with clients, and the tests and treatments for hyperadrenocorticism can help create healthier patients, happier clients, and a bottom line that reflects your good business and good medicine.