The Use of Hyperbaric Oxygen Therapy in Small Animal Medicine
Hyperbaric oxygen therapy (HBOT) is the use of oxygen under pressure delivered in a specialized chamber built to withstand high internal pressure.
Hyperbaric oxygen therapy (HBOT) is the use of oxygen under pressure delivered in a specialized chamber built to withstand high internal pressure. The patient breathes 100% oxygen and the pressure within should know the chamber increases to more than one atmosphere of pressure. The most common type of chamber used in veterinary medicine is a monoplace chamber, which was initially made for humans, or a veterinary-specific chamber of similar size. Up to 3 animals can potentially be treated together in this size chamber; however, the risks and benefits of treating multiple patients simultaneously must be assessed on a case-by-case basis.
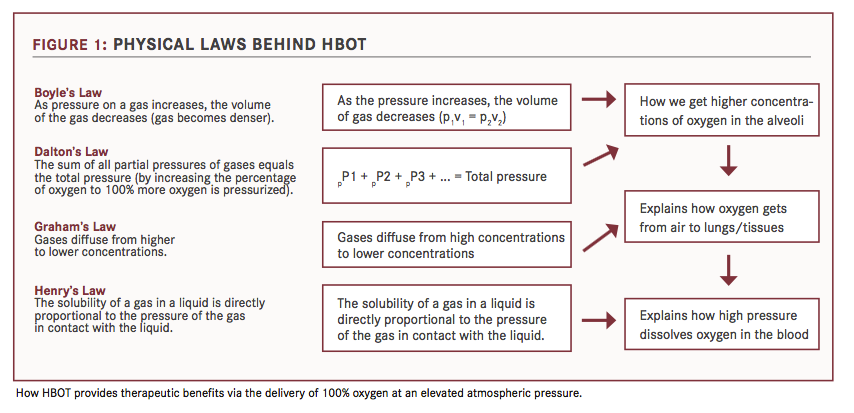
Understanding how HBOT works starts with a review of some of the important laws of physics and their resultant effects on the body. [FIGURE].
Direct Effects of Pressure
Pressure dissolves gas into solution, shrinks bubbles and decreases diffusion distances. At normal atmospheric pressure (measured at sea level as 1 atmosphere absolute or 1 ATA), arterial oxygen tension is 100 mm Hg and tissue oxygenation is 55 mm Hg. In 100% oxygen at 3 times atmospheric pressure, arterial oxygen tension is 2000 mm Hg and tissue oxygenation is 500 mm Hg. Oxygen dissolved in plasma results in oxygen transport and tissue survival without the need for hemoglobin.1
High oxygen gradients result in diffusion of oxygen into areas of low oxygen, which provides immediate help to ischemic and compromised tissue even with marginal or no blood flow. At elevated pressures, oxygen, nitrogen, and other gases will diffuse into solution and then be exhaled from the lungs.
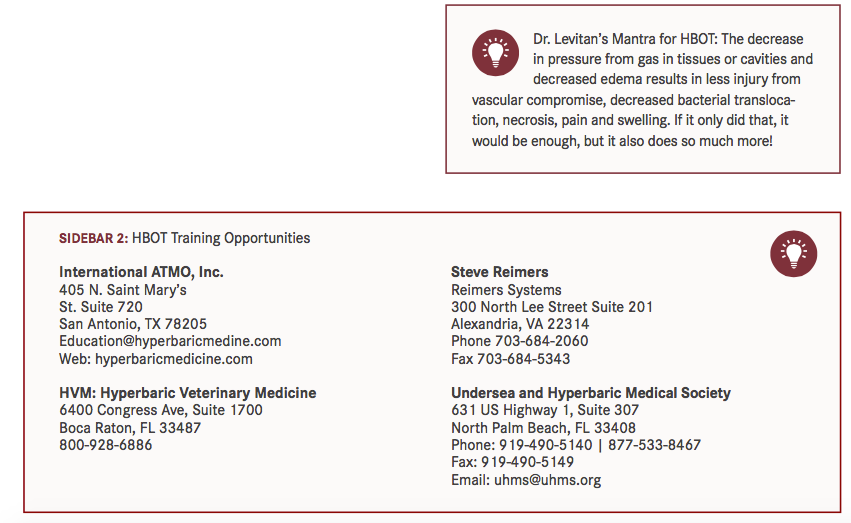
Compression from HBOT reduces all gas volumes, thereby relieving pressure from ileus, bloat, intraluminal gas accumulation, perioperative gastrointestinal obstruction, gas gangrene, emphysematous biliary or urinary bladder tissues and subcutaneous emphysema due to a reduction in gas volume, nitrogen diffusion into tissues and blood and a high gradient for nitrogen removal via respiration. The decrease in pressure from gas in tissues or cavities results in less injury from vascular compromise, and decreased bacterial translocation, necrosis, pain and swelling.2-8
Effects of 100% Oxygen Delivery Via Plasma
Infections, injury, and disease increase tissue demands for oxygen while such problems as anemia, toxins and hemorrhage can decrease the body’s ability to transport oxygen via hemoglobin. Additionally, conditions resulting in swell- ing and edema or vessel blockages increase the distance oxygen must travel to the tissues.
Delivery of 100% oxygen under pressure allows plasma to carry much more oxygen and reduces the importance of hemoglobin-based delivery.1 100% oxygen dissolved in plasma can be delivered from capillaries to tissues at least three times farther than delivered when carried by hemoglobin alone.1,9 And, increasing barometric pressure from 1.0 ATA to between 2.0 and 2.5 ATA increases the dissolved oxygen in plasma approximately 3-fold compared with a patient breathing room air. When the inhaled oxygen concentration is increased to 100% under the same increased pressure, the plasma oxygen concentration increases by almost 17-fold. In theory, with 100% oxygen at 2.5 ATA, enough oxygen can be dissolved in plasma to meet the normal requirements of the body at rest without the need for hemoglobin.1,9
Oxygen under pressure causes vasoconstriction by inducing smooth muscle contraction in all muscular vessels (arterial and venous), but not capillaries or lymphatics, and decreasing bleeding/oozing from vessels while allowing lymphatic channels to continue to clean up and remove edema. The increased partial pressure of oxygen in plasma and the increased CO2 in damaged tissues (CO2 is a more potent vasodilator than oxygen is a vasoconstrictor), offset the vasoconstriction so that tissue oxygenation remains high and microvascular blood flow improves.3
Medical Benefits of High Oxygen Tissue Levels
High oxygen levels reduce inflammation by mediating cytokines, prostaglandins, and nitric oxide, and have been shown to have direct bacteriostatic and bactericidal effects against gram positive, gram negative, aerobic and anaerobic microorganisms.3 High tissue oxygen levels have a synergistic antibiotic effect by aiding in the efficacy and action of aminoglycosides, sulfonamides, and cephalosporins, among others; inhibiting the growth of many fungal organisms; reducing free radical damage and reperfusion injury; and inhibiting toxins.10,11
Endorsement of HBOT in Human Medecine
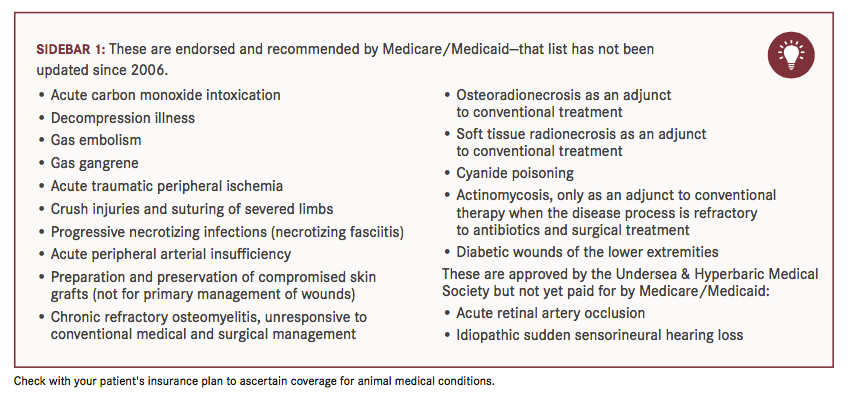
Although HBOT fell out of favor in the mid-1990s due to misuse and false claims, in the past 40 years, thousands of evidence-based scientific articles have elucidated its therapeutic value and the underlying cellular and physiologic mechanisms at work.12,13 The value of hyperbaric oxygen is now well appreciated in human medicine and accepted as treatment for many indications, 15 of which are routinely approved by Medicare and Medicaid [SIDEBAR 1].12 The Undersea and Hyperbaric Medical Society endorses its use for other conditions as well.
HBOT is also used to treat disease states not routinely endorsed by insurance even though varying degrees of efficacy have been demonstrated. These include severe sepsis, cerebral edema, burns, hepatic necrosis, pancreatitis, clostridial infections, head trauma, stroke and many more. There are also more controversial uses, not likely to be recommended by all physicians. These include treatment of nonvascular causes of chronic brain issues such as autism, Alzheimer’s disease and cognitive dysfunction associated with age.12,13
HBOT in Veterinary Medecine
HBOT has been tested on animals for many years. The earliest documentation of therapeutic use was in 1998. Since then, sporadic treatment reports have appeared in the veterinary literature. Currently, there are around 44 HBOT chambers being used for pets, and over 1000 being used for humans in the United States.
HBOT is especially useful in conditions already approved for human therapy [SIDEBAR 1] but, in my experience, there are other indications. Some cases detailing the use of HBOT are included below.
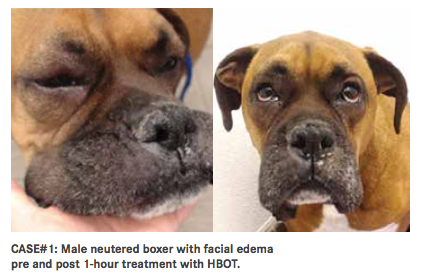
CASE #1: An 8-year-old male neutered boxer recovering from surgical debridement of necrotic pancreatic tissue developed edema from an allergic reaction to a fresh-frozen plasma transfusion. Instead of steroids, he received only HBOT therapy for 1 hour at 2 ATA. The result was reversal of the allergic reaction.
CASE #2: A 3-year-old female mixed breed dog presented with a severe degloving wound to the left rear leg. After cleaning and debriding the wound, supplemental HBOT therapy was instituted at 2.5 ATA for 1 hour twice daily for 3 days, followed by treatment at 2 ATA for 45 minutes twice daily for 2 days before being reduced to every other day for 2 days, along with other supportive care. The end result was rapid migration of healthy granulation tissue and new skin and hair growth.

CASE #3: A 7-year-old male intact corgi with lymphoma suffered an undetected extravasation event after chemotherapy with Adriamycin. The patient presented 40 days post treatment with severe swelling, tissue necrosis and compartment syndrome resulting in nerve entrapment with knuckling of the left forepaw. It was determined that standard immediate post-extravasation event treatment with dexrazoxane and sargramostim would likely be ineffectual and so HBOT was instituted at 2 ATA for 1 hour twice daily for 10 days, followed by 36, almost daily, additional treatments at the same dose for a total of 52 days. At the end of treatment, the wounds were healed and the corgi was walking normally. No adverse effects on cancer therapy were noted as he survived for 20 additional months before succumbing to lymphoma.

We have also seen improvement in patients affected by intervertebral disk disease, pancreatitis, burns, smoke inhalation, ischemic stroke, spider/snake bites, head trauma, and many other conditions. HBOT has also been used as adjunctive post-operative therapy in orthopedic cases in order to reduce swelling and speed healing. As a general rule, HBOT is most effective for acute conditions, although it has been shown to lessen pain and improve function in osteoarthritis, chronic intervertebral disk disease, long-term management of aspergillosis and many others. There are no established treatment regimens currently available, although anecdotal recommendations and guidelines abound. Many recommendations are extrapolated from human medicine. The number of treatments, frequency, and duration varies according to results, the owner’s personal schedule, and cost.
Safety and Training for HBOT
Overall, HBOT chambers are easy to use but can be dangerous to both the patient and the operator. Patient contraindications include certain lung pathologies, fever, and predisposition to seizures. There is also danger in prolonged exposure to 100% oxygen. However, because 100% oxygen is extremely flammable, operators must pay meticulous attention to its proper use. In February 2012, a horse-specific monoplace chamber in Florida exploded, killing the patient and the attendant. The cause was probably a spark created when the horse became agitated and kicked a metal plate on the inside of the chamber. Operators need to be aware that although rare, these accidents can happen and so proper training [SIDEBAR 2] and thorough adherence to safety precautions are musts.14
If you do decide to offer hyperbaric oxygen to patients, it should be made affordable and accessible. You should also invest in specialized training [SIDEBAR 2]. It is an adjunctive therapy, and you must be prepared to treat the entire patient and any underlying or comorbid conditions. For more information on how to start, visit the Veterinary Hyperbaric Medical Society website at www.vhbot.org, or email them at info@vhbot.org.
Dr. Levitan is a diplomate of the American College of Veterinary Internal Medicine. She received a Veterinariae Medicinae Doctoris from the University of Pennsylvania School of Veterinary Medicine. A board-certified specialist in small animal internal medicine, Dr. Levitan has also performed clinical research; lectured and taught courses in ultrasound, endoscopy and laparoscopy; published in veterinary journals; and serves as a consultant for many businesses.
References:
- Boerema I, Meijne NG, Brummelkamp WH, et al. Life without blood. J Cardiovasc Surg. 1960;182:133.
- Tibbles PM, Edelsberg JS. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334(25):1642—16
- Gill AL, Bell CNA. Hyperbaric oxygen: its uses, mechanisms of actions and outcomes. Q J Med. 2004;97:385—395
- Ambiru S, Furuyama N, Aono M, et al. Hyperbaric oxygen therapy for the treatment of postoperative paralytic ileus and adhesive intestinal obstruction associated with abdominal surgery: experience with 626 patients. Hepatogastroenterology. 2007;54(79):1925—1929.
- Yokota T, Suda T, Tsukioka S, et al. The striking effect of hyperbaric oxygenation therapy in the management of chronic idiopathic intestinal pseudo-obstruction. Am J Gastroentrol. 2000;95:285—288
- Al-Waili NS, Butler GJ. Effects of hyperbaric oxygen on inflammatory response to wound and trauma: possible mechanism of action. ScientificWorldJournal. 2006;6:425—441.
- Piantadosi CA. Pulmonary gas exchange, oxygen transport, and tissue oxygenation. In: Neuman TS, Thom SR, eds. Physiology and Medicine of Hyperbaric Oxygen Therapy. Philadelphia, PA: Saunders Elsevier; 2008: 133—185.
- Nylander G, Nordström H, Eriksson E. Effects of hyperbaric oxygen on oedema formation after a scald burn. Burns Incl Therm Inj. 1984;10(3):193—196.
- Bitterman H. Bench-to-bedside review: oxygen as a drug. Crit Care. 2009;13(1):205.
- Al-Waili NS, Butler GJ. Effects of hyperbaric oxygen on inflammatory response to wound and trauma: possible mechanism of action. ScientificWorldJournal. 2006;6:425—441.
- Jain KK. HBO therapy in infections. In: Jain KK, ed. Textbook of Hyperbaric Medicine. 5th ed. Cambridge, MA: Hogrefe & Huber Publishers, Inc.; 2009: 135—148.
- Centers For Medicare & Medicaid services. CMS.GOV. https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?ncdid=12&ver=3
- Undersea & Hyperbaric Medical Society. https://www.uhms.org/resources/hbo-indications.html
- Ocala Star Banner. http://www.ocala.com/news/20120216/report-released-on-hyperbaric-chamber-explosion
