The toxic effects of disulfoton in pets
Cassidy, a 4-year old spayed female golden retriever, was playing in the yard while her owner was gardening. After about an hour of gardening, the owner noted Cassidy was shaking so badly that she could barely walk. Cassidy had thick ropes of saliva coming from her mouth and began to have watery diarrhea. In the car on the way to the veterinary clinic, Cassidy vomited some dirt. By the time they arrived at the clinic, Cassidy was weak and could not rise.

Are you ready to handle cases of dogs exposed to disulfoton, a pesticide commonly used on roses and other flowers? (GETTY IMAGES/CHIARA BENELLI)
A look at potential toxins
Four outdoor agents came to mind as possible forms of toxicosis:
> Organophosphorus-type pesticides
> Metaldehyde snail and slug killer
> Tremorgenic mycotoxins from moldy food
> Backyard mushrooms: Amanita species (isoxazole), psilocybin mushrooms
The owner recalled treating his roses about a month earlier with a fertilizer that stated it would control aphids, too. The owner also remembered sprinkling some granules for the slugs a few weeks previously. He called home and found out that the fertilizer contained 1% disulfoton, and the snail and slug bait he had used contained 2% metaldehyde. The owner did not see Cassidy ingest anything because he was busy with the roses.
Initial diagnostic steps
On physical examination, Cassidy was bradycardic (heart rate = 53 beats/min), profusely drooling, and tachypneic (respiratory rate = 60 respirations/min) with moderate dyspnea and moist lung sounds. She was still experiencing tremors and unable to get up. Her temperature was 105.5 F (40.8 C). She had vomited several more times and had bloody diarrhea after her temperature was taken.
A review of the suspected toxicants revealed that disulfoton (Di-Syston-Bayer CropScience) is an organophosphorus insecticide with a narrow margin of safety. Although the signs that Cassidy was experiencing were consistent with all of the suspected toxicants listed previously, bradycardia is commonly seen with only organophosphates.
An intravenous catheter was placed, and pretreatment blood samples were collected and placed in purple and red top tubes. Fluid therapy was instituted.
Blood samples for a complete blood count, an electrolyte panel, and a serum chemistry profile were submitted to the laboratory along with a purple top (EDTA) tube to measure the blood acetylcholinesterase concentration. The abnormal results are listed in Table 1.
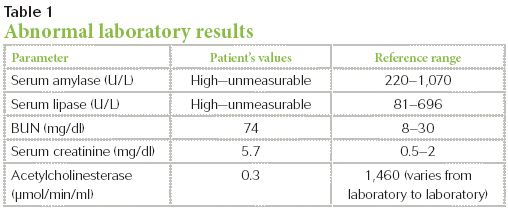
Table 1: Abnormal laboratory results
Definitive diagnosis and treatment
Cassidy was given atropine sulfate at a dose of 0.02 mg/kg intravenously with very little change in heart rate. This lack of response to a preanesthetic dose of atropine strongly suggested an exposure to a cholinesterase inhibitor such as disulfoton. Therapeutically, the atropine dose was increased to between 0.1 to 0.2 mg/kg intravenously and repeated as needed to control muscarinic effects until Cassidy's breathing and heart rate stabilized. This demonstrates that up to ten times the preanesthetic dose may need to be given to control muscarinic signs.
Her bloodwork revealed a depressed blood acetylcholinesterase concentration (< 25% of normal), strongly supporting a diagnosis of exposure to a cholinesterase inhibitor such as disulfoton. Cassidy's elevated amylase and lipase activities were also consistent with pancreatitis that often accompanies disulfoton ingestion.
Cassidy remained weak and ataxic despite her favorable response to atropine. She was given pralidoxime chloride (2-PAM, Protopam-Baxter) at a dose of 20 mg/kg intramuscularly b.i.d. After three doses, she was able to get up and move around safely on her own. Cassidy recovered from the muscarinic and nicotinic signs within 36 hours of her initial signs, but she experienced pancreatitis for another five days.
Discussion
Gardeners often use products to enhance the beauty of flowers and shrubs and decrease insect damage to vegetables.
Disulfoton is available as granules, spray, or spikes, and is often marketed specifically for pests against roses. It is often mixed with fertilizer or blood and bone meals before use. The insecticide is carried into the plant via the root system, moving to all parts of the plant through natural growth and sap movement. After about five days, feeding insects will consume the insecticide and die.1 It can last in the environment up to seven weeks.
Organophosphorus insecticides cause an increase in the neurotransmitter acetylcholine at the neuromuscular junction by binding to acetylcholinesterase via competitive inhibition. This results in accumulation of acetylcholine in preganglionic neurons of the parasympathetic and sympathetic nervous systems and the neuromuscular junction.
Acetylcholine also serves as the neurotransmitter in the postganglionic parasympathetic nervous system. The resulting excess acetylcholine results in muscarinic and nicotinic signs. The muscarinic signs ("SLUDDE") include salivation, lacrimation, urination, diarrhea, dyspnea, and emesis. Nicotinic signs may include tremors, seizures, weakness, and, potentially, paralysis.2
Death from organophosphorus compounds such as disulfoton can occur due to hypoxia from excessive bronchial secretions, bronchoconstriction, arrhythmias, and centrally mediated respiratory paralysis and failure. Pancreatitis is often a common complication associated with disulfoton exposures.
Blood or plasma cholinesterase activity can help to confirm disulfoton exposure. This should be obtained in a purple top tube (EDTA).3 Acetylcholinesterase concentrations less than 50% of normal strongly suggest an organophosphorus or a carbamate exposure.
A preanesthetic dose of atropine can be used as a test at 0.02 mg/kg intravenously. Monitor the patient's heart rate before administering the atropine and immediately afterward. The expected response if disulfoton was involved should be no significant change in heart rate or bronchial secretions.3
Treatment of organophosphorus intoxication requires atropine, which competitively inhibits the effects of acetylcholine at the postsynaptic membrane. The dose of atropine required to control muscarinic signs is 0.1 to 0.2 mg/kg and is repeated as needed.
Pralidoxime is considered antidotal to the nicotinic signs associated with organophosphorus toxicosis.4 It needs to be given before "aging" occurs (irreversible binding of organophosphorus to acetylcholinesterase, which occurs to different degrees and at different rates, depending on the organophosphorus agent), but this drug is not widely available. The dose is 10 to 20 mg/kg given intramuscularly b.i.d. Doses up to 50 mg/kg given intravenously, intramuscularly, or slowly intravenously at varying intervals have been reported.5 If there is no response after three doses, discontinue use since the value of additional doses is doubtful. Methocarbamol (55 to 220 mg/kg intravenously to effect) or diazepam (0.1 to 0.5 mg/kg intravenously) can also be used to control muscle tremors, shaking, and seizures.
Some affected individuals will have predominantly nicotinic signs. Atropine is not indicated in these cases. Pralidoxime should be used early in these cases to bind preferentially to the organophosphorus before the organophosphorus binds irreversibly with acetylcholinesterase. Discontinue the pralidoxime if nicotinic signs worsen shortly after administration or if no improvement is seen after three doses. Nicotinic signs can also be treated with methocarbamol, diazepam, or barbiturates along with supportive care. Full recovery may take several days or weeks until the body synthesizes new acetylcholinesterase.
The potential associated pancreatitis is thought to be secondary to direct cellular damage and obstruction of pancreatic ducts.6 Treatment of this pancreatitis is the same as traditionally acquired pancreatitis.
Symptomatic animals usually recover within two to five days, with no long-term sequelae expected.
Helen Myers, DVM, ASPCA Animal Poison Control Center, 1717 S. Philo Road, Suite 36 Urbana, IL 61881.
To view the references for this article, visit dvm360.com/DisulfotonRefs.
About the ASPCA Animal Poison Control Center (APCC)

The ASPCA Animal Poison Control Center (APCC) is a 24-hour animal emergency consultation service that provides treatment and diagnostic recommendations to animal owners and veterinarians regarding animal poisoning cases 24 hours a day, 7 days a week, 365 days a year. Since 1978, the veterinary staff at the APCC has experience of handling more than 2 million animal poisoning cases involving pesticides, herbicides, plants, human and animal drugs, heavy metals, and many other potentially hazardous chemicals. A $65 consultation fee may apply. This includes follow-up consultations for the duration of the case. If you think your animal may have ingested a potentially poisonous substance, call (888) 426-4435. Additional information can be found online at
www.aspca.org/apcc
.