An update on diagnosing and treating primary lung tumors
The goal of this article is to describe the common histologic variants, clinical signs, biologic behavior, and newest options for early diagnosis and effective treatment of primary lung tumors in dogs and cats.
Although primary pulmonary neoplasms are rare findings in dogs and cats, the reported incidence may be increasing.1-6 This potential rise may reflect multiple factors, including increased exposure to environmental carcinogens, the availability of more sensitive diagnostic tools, a greater number of necropsies being performed, and improved animal healthcare services resulting in the increased longevity of companion animals.1,2,4,7
Through the growing appreciation for the human-animal bond, many pet owners now support the practice of preventive or early-detection medicine in companion animals for several disease processes, including cancer. The benefit of annual senior pet examinations, which include survey thoracic radiographs, may allow for the early diagnosis of lung cancer in asymptomatic animals. Although the prognosis is generally better for patients with small, well-differentiated, peripherally located lung tumors,2,3,8 additional prognostic factors should be considered for predicting survival outcomes in dogs and cats with pulmonary neoplasms.

Illustration by Bonnie Hofkin
Pneumonectomy remains the cornerstone of therapy for primary lung tumors, but novel adjunctive therapies (e.g. combination chemotherapy) are being developed and evaluated for improving local disease control. In addition to advances in detecting and treating primary lung tumor growth, new systemic therapies have been investigated for prolonging the disease-free interval, as well as palliating secondary bony metastasis.9-11
The goal of this article is to describe the common histologic variants, clinical signs, biologic behavior, and newest options for early diagnosis and effective treatment of primary lung tumors in dogs and cats.
PREDILECTION AND INCIDENCE
Primary lung tumors represent about 1% of newly diagnosed tumors in dogs and cats, although the overall incidence is much lower in cats (Table 1).4,6,7,12-14 Some studies suggest that these tumors may be more common. In a life span study in a closed beagle colony, the incidence of primary lung tumors correlated with increasing age.15 For all beagles, an overall incidence of primary lung tumor formation was 8.8%; the incidence reached as high as 25% in geriatric dogs at necropsy.15 The factors that may have contributed to the high incidence of primary lung tumors in this beagle colony were not identified but may have included genetic, dietary, and unique environmental factors specific to the closed colony.

Table 1: Comparison of Lung Cancer in People, Dogs, and Cats
Primary lung tumors occur most commonly in larger, older animals, with a mean age of 10 or 11 and 12 years in dogs and cats, respectively.2,4,5,8,12-14,16 Although no definitive breed or sex predilection has been identified, boxers represented 37% of all lung tumor patients in one study,12 and in a feline investigation, older females were more often affected than males.10,14
Similar to people in which chemical carcinogenesis plays a prominent role in the genesis of primary lung tumors, a causal link is suspected to exist between smoking households and primary lung tumors in dogs, especially in mesocephalic and brachycephalic breeds.17 Moreover, dogs living in urban environments more commonly have lung tumors than do dogs in rural settings.4 This apparent environmental effect could reflect the greater pollutants within an urban environment or may simply be due to the greater population density of animals receiving routine veterinary care.
In dogs, the right caudal lung lobe is the most common anatomical location of primary pulmonary neoplasia.5,6,8,10,13,16,18 This observed anatomical preference is thought to be a result of greater lung tissue mass, thereby increasing the likelihood for spontaneous mutations within the right caudal lung fields.12 In cats, the caudal lobes are also more commonly affected, but they tend to have an equal occurrence in the right and left lung fields.14
HISTOLOGIC CLASSIFICATION
Carcinomas are the most frequently diagnosed lung tumors, but consensus for the most common histologic subtype is lacking. This lack of agreement is partially attributed to researchers using differing classification schemes, precluding direct comparisons between historical and recent studies.
In veterinary medicine, the simplest classification scheme is by general cellular morphology, which includes adenocarcinoma, squamous cell carcinoma, and anaplastic carcinoma.6,19 Primary lung carcinomas can also be organized by topographical location, inclusive of bronchial, bronchoalveolar, or alveolar carcinoma.6,10 Confusingly, some studies categorize bronchoalveolar carcinoma into a separate cellular morphologic subtype altogether.5,8,14 Although organizing primary lung tumors by topographical location is useful in people, veterinary pathologists do not recommend this classification scheme in companion animals because of the advanced stage of the disease at the time of diagnosis, which makes determining the exact topographical origin of lung tumors extremely difficult.10,19 Instead, in veterinary studies, pulmonary carcinomas are generally divided into four subgroups—adenocarcinoma, squamous cell carcinoma, bronchial gland carcinoma, and alveolar cell carcinoma.4,10
Adenocarcinoma, regardless of tissue cell origin, is the most common histologic type in dogs and cats.2,4,10,12-14,16,19 In two studies, adenocarcinoma made up 74% to 77% of all primary lung tumors histologically examined.4,10 Other reports suggest adenocarcinoma is more common in people and cats and bronchoalveolar carcinoma is more common in dogs.5 Squamous cell carcinoma, which is the most common pulmonary neoplasm in people, is less common in companion animals, representing 6% and 4% of all of canine and feline lung tumors, respectively. Anaplastic carcinoma is the rarest morphologic subtype in dogs and cats,10 but it is still more common than primary mesenchymal lung tumors, which are extremely rare in dogs and cats.4,10,20
In a case report of four dogs with mesenchymal or mixed-cell-origin lung tumors, the age range was 4 to 15 years, with spayed females and castrated males in equal proportion.20 All tumors were in the right lung fields—two were hamartomas, one was a pulmonary chondroblastic osteosarcoma, and one was a biphasic pulmonary blastoma. Only the patient with the chondroblastic osteosarcoma had pulmonary metastasis visible on thoracic radiography. Both patients with hamartomas were alive at least one year post pneumonectomy.20 Other reports of canine sarcomas include an osteosarcoma, a chondrosarcoma, and a Spirocerca lupi-associated fibrosarcoma, with two of the three patients presenting with hypertrophic osteopathy.21-23
Pulmonary lymphomatoid granulomatosis is an extremely rare, diffuse disease of the canine lung that has a yet undetermined cause and may be immune-mediated or preneoplastic in origin.24-26 Fine-needle aspiration provides poor diagnostic yield with this disease process, and definitive diagnosis must be based on histologic examination. However, because of the historically rapid response to chemotherapy, empirical treatment may be used to aid in diagnosis.24 Of the primary neoplastic diseases of the lungs, pulmonary lymphomatoid granulomatosis carries the best prognosis.24,25
The anatomical location and histologic subtype of primary pulmonary tumors in dogs tend to share similar distribution patterns observed in people. Adenocarcinomas usually present as peripheral, solitary, well-defined masses (Figure 1), while bronchoalveolar carcinomas often manifest as peripheral multifocal densities (Figure 2).5,12,14,18 And primary lung squamous cell carcinomas tend to grow as solitary, hilar masses.10,12,14,18

1. A lateral thoracic radiograph of a 10-year-old castrated male German shepherd presented for evaluation of an intermittent, nonproductive cough of six months' duration. A soft tissue mass effect is identified in the left caudal lung field. The histologic diagnosis was pulmonary adenocarcinoma. (Photograph courtesy of Dr. Laura Garrett.)
In cats, adenocarcinomas tend to manifest either as a well-circumscribed, cavitated mass in the center or periphery of the lobe or as a localized (lobar) alveolar pulmonary infiltrate that is often calcified (25% of cases). Bronchoalveolar carcinomas occur as pleomorphic, multifocal, or diffuse opacities located in the middle to peripheral portions of the affected lobes, with two-thirds of cases having pleural involvement on radiographs. Unlike in dogs or people, squamous cell carcinomas in cats show extreme variability in radiographic pattern but tend not to be hilar in origin.14

2. A lateral thoracic radiograph of an 8-year-old spayed female Labrador retriever presented for evaluation of a decreased appetite and lethargy of four weeks' duration. Multiple soft tissue opacities affecting the pulmonary parenchyma are identified, which were cytologically consistent with bronchoalveolar carcinoma. (Photograph courtesy of Dr. Laura Garrett.)
Despite certain growth and distribution patterns associated with primary lung tumors in companion animals, it remains impossible to definitively classify such tumors based purely on topographic anatomy, mostly because, as mentioned earlier, canine and feline neoplasms are often too advanced at diagnosis to identify their anatomical site of origin.5,12 This limitation has been underscored in several veterinary studies in which no correlation was found between a tumor's location and its histologic subtype. Thus, once a pulmonary mass has been identified on initial thoracic imaging, histologic or cytologic evaluation of the suspect lesion is absolutely necessary for definitive diagnosis.8,16,19
CLINICAL SIGNS
The clinical signs of primary lung tumors depend on many factors such as tumor invasiveness, the extent of lung tissue involvement, the presence of metastatic disease, and the occurrence of paraneoplastic syndromes.
Dogs
The most common sign in dogs is a nonproductive cough, occurring in 52% to 58% of dogs with a primary lung tumor.2,4,8,12 Other respiratory signs may include tachypnea, wheezing, exercise intolerance, and hemoptysis. Nonspecific signs in dogs are common and include lethargy, weight loss, and anorexia.2,4 Dyspnea may occur if a large portion of the lung is involved or if pneumothorax, pleural effusion, or concurrent disease (congestive heart failure or tracheal collapse) is present.1,8 Severe lameness and pain may also be a presenting complaint if hypertrophic osteopathy or bone metastasis has occurred.1,2,4,12 Despite many patients presenting with overt clinical signs associated with primary lung tumors, up to 30% of all dogs will have no signs of disease at the time of diagnosis.2,4,12
Cats
Clinical signs seen in cats with primary pulmonary neoplasia are extremely variable, but dyspnea, weight loss, lethargy, anorexia, weakness, and vomiting are frequently reported.16,27 In one study of 35 cats with primary lung tumors, about 25% of cats presented with lameness, likely resulting from digital skeletal metastasis associated with primary pulmonary carcinoma. Respiratory signs were noted in only one-third of the cats, and coughing was rarely reported.1 In contrast, another feline study found that all 86 cats had at least one clinical sign directly or indirectly related to their primary lung tumor, and 53 of the cats (61.6%) had signs of respiratory difficulty.16 In general, cats with primary lung tumors present with a wide range of clinical findings, and the absence of overt pulmonary signs should not preclude a primary lung tumor as a differential diagnosis.
DIAGNOSIS
Primary pulmonary neoplasms are usually an incidental finding in animals presented for general health checks or evaluation of nonspecific signs. Thoracic radiography is often the initial step in evaluating patients with respiratory disease, but radiographic patterns are not specific for a single disease process so further diagnostic tests are necessary.
Thoracic radiography
The appearance of primary lung tumors varies from a solitary mass (Figure 1) to involvement of an entire lung lobe or multiple lobes (Figure 2), indicating metastatic disease or multicentric pulmonary tumors. Radiographic assessment may be confounded by atelectasis secondary to pneumothorax or pleural effusion. Pleural effusion may result from regional lymph node metastasis, extension of the tumor into the pleura, or concurrent disease such as congestive heart failure or other nonneoplastic processes such as hypertrophic cardiomyopathy, feline infectious peritonitis, and chylothorax.1,14 But keep in mind that pleural effusion devoid of neoplastic cells on cytologic examination does not necessarily rule out primary pulmonary neoplasia.14,19,28
In most patients without pleural effusion or severe concurrent thoracic disease, survey thoracic radiographs are considered a high-yield diagnostic test, often revealing a pulmonary mass when present.16 Differential diagnoses for pulmonary masses include primary lung tumors (77% in one study), granulomas, cysts, abscesses, infarcts, diaphragmatic hernias, and metastatic neoplasia.4,29
Cytology
Although the most accurate way to definitively diagnose a pulmonary mass is through surgery and histologic examination, other less-invasive diagnostic techniques, such as cytology, may be attempted first. Fine-needle aspiration appears to be the safest and most convenient method of harvesting cytologic samples for initial diagnosis (Figure 3). A recent study comparing cytologic and histologic diagnosis of pulmonary neoplasia revealed that cytologic samples retrieved with 25- to 27-ga needles showed agreement with histologic diagnosis in 82% of cases, with 100% specificity and 77% sensitivity.30 As would be expected, cytologic accuracy for diagnosing neoplasia is higher with ultrasound guidance vs. blind aspiration, as visualization of the suspect primary lung tumors is necessary to maximize appropriate sample collection (Figure 4).30 Fluoroscopy also facilitates the accurate and efficient retrieval of cellular samples from suspect pulmonary tumors.31
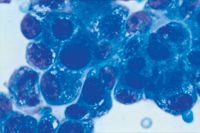
3. A photomicrograph of a cytologic sample revealing primary lung adenocarcinoma in a geriatric dog. A cohesive cell population is identified with cytologic criteria of malignancy including anisocytosis, anisokaryosis, multiple nucleoli, nuclear molding, and foamy cytoplasm (Wright's stain, 1,000X). (Photograph courtesy of Dr. Laura Garrett.)
Although fine-needle cytology with small-gauge needles (25 to 27 ga) appears safe and relatively accurate, studies using large-gauge needles (18 to 21 ga) demonstrate even greater correlation between cytologic and histologic results collected from suspect lung lesions.32 However, despite a higher cellular yield, the complication rate using 18- to 21-ga needles is reported to be 46%, with a fatality rate of 15%.32 In contrast, no substantial complications have been reported with using 22- to 25-ga needles in companion animals for retrieving cytologic samples from lung parenchymal lesions.33 Furthermore, in a recent human study no significant difference was identified in diagnostic sample retrieval using 18-, 22-, or 25-ga needles.34 These studies suggest that 22-ga needles should be sufficient to offer good diagnostic yield with a low complication rate.

4. A thoracic ultrasonogram in a dog with a peripherally located primary lung tumor demonstrates a hypoechoic lesion immediately adjacent to the thoracic wall (arrows). Ultrasound-guided fine-needle aspiration improves the chances of a diagnostic sample. (Photograph courtesy of Dr. Laura Garrett.)
In addition to needle size, the technique used for sampling is important, as fenestration (sampling without the use of negative pressure) has proved to be more effective than aspiration (using a syringe to create negative pressure). Although sample volume is decreased with fenestration, cellularity is improved because of less hemodilution.35
The limitations of fine-needle aspiration cytology include poor cell recovery, poor exfoliation of certain cell types (i.e. mesenchymal cells), failure to obtain a representative sample, and the inability to provide architectural information (i.e. vascular lesions or fibrosis).30 Other methods of obtaining cytology samples such as transtracheal wash and bronchoalveolar lavage offer poor diagnostic yield with primary pulmonary tumors when compared with fine-needle aspiration.4,16,30,36-38
Computed tomography
The correlation between tracheobronchial lymph node involvement and shorter remission times stresses the importance of computed tomography (CT) in the diagnostic work-up of dogs with primary lung tumors.2,3,7 In a study of 14 dogs with primary lung tumors, researchers evaluated the accuracy of CT vs. thoracic radiography in determining tracheobronchial lymph node involvement. CT had greater sensitivity and an increased predictive value for detecting tracheobronchial lymph node metastasis. The overall accuracy of CT in detecting lymph node metastasis was 93% compared with 57% for thoracic radiographs. False negative diagnoses made with thoracic radiographs may be attributable to the fact that the lymph nodes were still small (< 15 mm) or may have been obscured by surrounding structures, including the primary tumor itself.7
The sensitivity of CT is also superior in imaging metastatic pulmonary nodules when compared with thoracic radiography. CT was found to detect not only smaller pulmonary nodules (1 mm, compared with the minimum nodule size of 7 to 9 mm detectable on radiographs) but also a greater number of total nodules at more precise lobar locations (Figure 5). Radiographs failed to detect 90% of nodules detected on CT.39 These recent studies suggest that thoracic CT is rapidly becoming a mandatory diagnostic test performed before surgical removal of any primary tumor with potential pulmonary metastasis.

5. A thoracic computed tomographic image from a 12-year-old castrated male domestic shorthaired cat presented for evaluation of inappetence and weight loss. A cavitated mass (arrows) is identified in the periphery of the right caudal lung lobe. The mass was removed with thoracoscopic lung lobectomy, and the histologic examination results revealed a well-differentiated adenocarcinoma. (Photograph courtesy of Dr. Kristen O Dell-Anderson.)
METASTASIS AND STAGING
The presence of metastasis greatly affects prognosis, and appropriate clinical staging involves thoroughly investigating the common sites of pulmonary tumor dissemination. Pulmonary carcinomas tend to invade locally and spread through the lymphatic system to additional lung sites, hilar lymph nodes, and other thoracic tissues.2,3,5,12,15,16 Multiple tumor masses within the lung may indicate intrapulmonary metastasis or multicentric primary lung tumors.6 In addition to neighboring lung tissue, additional sites of metastasis include other lymph nodes, abdominal viscera, and the kidneys.12 Less common sites include the uvea, brain, and adrenal gland.40
In dogs, the rate of metastasis correlates well with the histologic type of tumor. The reported rate of metastasis is 50% for adenocarcinoma, with the most common sites of metastases being the tracheobronchial lymph nodes or other sites within the thoracic cavity.2,3,12,15 The metastatic rate is 90% for the more aggressive squamous cell carcinomas and anaplastic carcinomas.12
Primary pulmonary adenocarcinomas in cats appear to have a higher rate of metastasis than those in their canine counterparts and may be partially explained by a higher incidence of poorly differentiated adenocarcinomas in cats.5,10,16 In a study of 86 cats, 75.6% had evidence of metastatic disease at the time of diagnosis. Twenty-five cats (29%) had bronchial lymph node metastasis, while 40 cats (46.5%) had distant metastasis involving the pleural cavity or extrathoracic sites including the skeletal muscle, skin, liver, spleen, brain, kidneys, intestines, and bone.16 The mode of metastasis in feline primary lung tumors is poorly understood, but clinical evidence supports lymphatic and hematogenous routes of metastasis.41,42

6. An 11-year-old castrated male domestic longhaired cat presented for evaluation of recurrent nail bed infection and pain involving the third digit. Removal of the diseased toenail revealed a small, nonhealing wound. (Photograph courtesy of Dr. Laura Garrett.)
Although not a common site of metastasis for primary lung tumors in dogs, the digit is a frequent metastatic site in cats with primary lung tumors, specifically squamous cell carcinoma, and is referred to as lung-digit syndrome (Figures 6-9). In a study of 64 cats examined for lytic digital lesions, only eight had primary digital carcinoma, while the remaining 56 cats (87.5%) had digital metastases of a primary pulmonary carcinoma. The preponderance of digital cancers being metastatic foci greatly emphasizes the need for thorough staging, especially thoracic imaging, before amputating suspected digital tumors in cats.42

7. A radiograph of the right front foot of the cat in Figure 6 reveals bony destruction involving the third digit (long arrow) and soft tissue swelling (short arrows). (Photograph courtesy of Dr. Laura Garrett.)
PROGNOSTIC FACTORS
The World Health Organization's tumor, node, metastases (TNM) classification scheme for staging tumors has great value when predicting survival time.

8. A lateral thoracic radiograph of the cat in Figure 6 identifies a soft tissue opacity (arrows) involving the left caudal lung lobe. (Photograph courtesy of Dr. Laura Garrett.)
Dogs
Metastasis to the tracheobronchial lymph nodes is the single best predictor of remission and survival time for dogs with primary lung tumors treated with surgery.2,3 Median survival times in dogs with positive tracheobronchial lymph nodes based on histology range from 26 to 255 days, while patients with no lymph node involvement achieve median survival times ranging from 120 to 452 days.2,3,8 When lymph nodes were assessed before or during surgery, dogs with enlarged nodes survived a median of 60 days, while patients with normal size nodes had median survival times ranging from 285 to 345 days.3
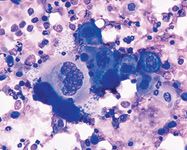
9. A fine-needle aspirate of a pulmonary mass identifies a cohesive population of basophilic, epithelial cells with squamous differentiation in a background of suppurative inflammatory cells. Multiple criteria of malignancy are evident, including anisocytosis and an increased nuclear to cytoplasmic ratio, consistent with primary pulmonary squamous cell carcinoma. Pulmonary squamous cell carcinoma is often associated with metastasis to the digits in cats. (Wright's stain, 500X). (Photograph courtesy of Dr. Laura Garrett.)
Several additional variables were found to affect prognosis when evaluated simultaneously, including histologic score, regional lymph node involvement, and detection of clinical signs (Table 2). For histologic score, patients with differentiated adenocarcinomas had median survival times ranging from 251 to 495 days, while patients with other tumor types survived between 44 and 240 days.2,3,8 In patients in which clinical signs were detected at presentation, median survival times ranged from 240 to 300 days, while asymptomatic dogs achieved much longer survival times ranging from 545 to 900 days.2,8 In one study, tumor size also showed some correlation to prognosis. Patients with a primary tumor size < 100 cm3 (5 cm diameter) had the greatest mean survival time of 20 months (median 17.5 months) compared with 7.8 months (median 8.5 months) for patients with tumors > 100 cm3.8
Table 2: Comparison of Canine Survival Times in Three Prognostic Studies
Cats
Because cats tend to have a higher incidence of poorly differentiated adenocarcinomas,10,16 it is not surprising that cats with primary lung tumors usually do not survive as long as dogs do. In a study of 21 cats treated with surgical resection, only histologic differentiation of the primary lung tumor had a significant correlation with survival time.27 Twelve cats with moderately differentiated tumors (57.1%) had a median survival time of 698 days, while nine cats with poorly differentiated tumors (42.9%) had a median survival time of 75 days. Although the study had inadequate power for statistical analysis of lymph node status, it did appear, as in dogs, that draining lymph node involvement may correlate with survival time, as 12 cats without enlarged tracheobronchial lymph nodes survived for a median of 412 days, whereas four cats with enlarged lymph nodes survived only a median of 73 days.27
In addition to histologic differentiation and lymph node enlargement, digital metastasis in cats with primary lung tumors is a poor prognostic finding. Cats with digital metastases have an average survival of 4.9 weeks (median 4 weeks) compared with a survival of 29.5 weeks (mean 12.5 weeks) in cats with primary digital squamous cell carcinoma.42
PARANEOPLASTIC SYNDROMES
In a retrospective study of 210 dogs with primary lung tumors, paraneoplastic syndromes were observed, but their frequency was low (< 6%): Six dogs had radiographic signs of hypertrophic osteopathy (2.9%) (Figure 10), two dogs were hypercalcemic, two dogs had a fever, and two dogs had tumor-induced secretion of adrenocorticotropic hormone (ACTH).4 From other investigations, the development of hypertrophic osteopathy in dogs with primary lung tumors has been reported to range from 4% to 17%.2,12 Overt lameness and pain in dogs with primary lung tumors may not always indicate hypertrophic osteopathy, as skeletal metastasis could also cause similar clinical signs of pain and discomfort. Other less frequent hematologic paraneoplastic syndromes associated with primary lung tumors in dogs include absolute erythrocytosis and leukocytosis.43,44

10. A lateral forelimb radiograph of a geriatric dog presented for evaluation of severe lameness and pain. Note the extreme periosteal proliferation consistent with hypertrophic osteopathy. The dog had a primary pulmonary carcinoma. (Photograph courtesy of Dr. Laura Garrett.)
Paraneoplastic syndromes in cats occur even less frequently. In a study of 86 cats with primary lung tumors, none of the patients experienced paraneoplastic syndromes.16 Although lameness may be a common presenting sign (25% in one study), it is usually indicative of bone metastases rather than hypertrophic osteopathy.1 Single case reports of paraneoplastic syndromes have been suggested in cats, including marked leukocytosis in a cat with squamous cell carcinoma, hypercalcemia with bronchogenic adenocarcinoma, and thrombocytosis with bronchoalveolar carcinoma.45-47
TREATMENT
The treatment of choice for solitary primary pulmonary tumors in dogs and cats is wide surgical resection—either a complete lung lobectomy or a partial lobectomy if the tumor is in the periphery.27,48 However, in cats more often than dogs, even if a single pulmonary nodule is seen radiographically, it is not uncommon to find multiple small lesions at surgery, suggesting the importance of advanced diagnostic imaging (CT or magnetic resonance imaging) before surgery.1
Surgery
Given the advent of fiberoptic technologies and the training of surgical residents in noninvasive techniques, thoracoscopic lung lobectomy is becoming a more common surgical approach for managing lung tumors in companion animals. When compared with thoracotomy in people, the results of thoracoscopy are less tissue trauma, decreased morbidity, shorter hospitalization, and earlier return to normal activity.49 Adequate exposure of the thoracic cavity and access to the hilar lymph nodes may still require conventional thoracotomy, so thoracoscopic procedures are best suited for removing small, peripherally located masses.48
For conventional thoracotomy, a lateral intercostal surgical approach allows access to the primary bronchi for lobectomy of the side involved but prevents adequate examination of the opposite hemithorax. During thoracotomy, examine and palpate all accessible lung lobes and tracheobronchial lymph nodes for metastasis or multifocal primary masses. If the tracheobronchial lymph nodes appear enlarged, they should at least be biopsied and preferentially be extirpated.
Adjuvant chemotherapy
After the primary tumor and associated draining lymph nodes are removed, adjunctive chemotherapy may be warranted based on host factors (clinical stage) and tumor characteristics (histologic findings). Despite the availability of new chemotherapeutic drugs, few well-designed prospective studies have investigated the efficacy of one or multiple agents for treating primary pulmonary neoplasms in dogs and cats.
Vinorelbine, a semisynthetic derivative of vinca alkaloids, has recently been described for treating various neoplasms, including primary lung tumors, in dogs.50 Vinorelbine is widely distributed in all tissues except for the brain, with concentrations in the lungs reaching 13.8-fold higher than other vinca alkaloids.51 In one study, two of seven dogs with macroscopic bronchoalveolar carcinoma achieved a partial remission after vinorelbine treatment. Furthermore, in dogs with microscopic bronchoalveolar carcinoma (incompletely excised primary or lymph node metastases), vinorelbine's anticancer activity was suggested by the relatively durable survival times of 113, 196, and 730+ days in three dogs treated with surgery and systemic vinorelbine.50 Further investigations are warranted to determine the effectiveness of adjunctive vinorelbine for treating bronchoalveolar carcinomas as well as other pulmonary neoplasms in dogs.
In a study of 15 dogs with primary lung tumors treated by lobectomy, five dogs with advanced recurrent pulmonary carcinoma received one of three chemotherapy protocols: 1) cyclophosphamide, vincristine, and methotrexate, 2) vindesine alone, or 3) vindesine and cisplatin.8 Two dogs treated with vindesine and cisplatin showed partial responses, with greater than 50% reduction in radiographic lesions. Anorexia was the only side effect of the cyclophosphamide, vincristine, and methotrexate protocol, while reversible neurotoxicity was the only side effect of vindesine alone. In the dogs treated with vindesine and cisplatin, mild leukopenia and gastrointestinal upset were seen in both dogs, while only one dog experienced reversible peripheral neurotoxicity consisting of rear limb weakness and decreased patellar reflexes.8 The anecdotal favorable response observed in the two dogs treated with cisplatin and vindesine, along with this protocol's acceptable toxicity profile, warrants further studies examining this combination of chemotherapeutic agents for treating primary lung cancer, especially adenocarcinomas.8
THE FUTURE IN TREATMENT
Although complete surgical removal of primary lung tumors before metastasis offers the best hope for a cure, several promising treatment modalities are on the horizon.
Intensity-modulated radiation therapy
An alternative to conventional lung lobectomy in companion animals is the use of intensity-modulated radiation therapy (IMRT). This treatment modality allows the delivery of curative-intent megavoltage radiation to the neoplastic lesion. Excessive delivery of radiation to normal tissues is minimized by collimating multiple treatment beams in the radiation field to conform three-dimensionally to the geometry of the cancerous mass.52
In a case study, the effectiveness of IMRT for treating a primary bronchoalveolar carcinoma in a dog was assessed by using positron emission tomography combined with CT. After treatment with IMRT, the dog survived 22 months, only to be euthanized for clinical signs considered unrelated to the primary lung tumor or treatment with IMRT. This anecdotal case report demonstrates favorable clinical outcomes with combination IMRT and positron emission tomography and CT for the treatment and response-assessment of a primary lung tumor in a dog.52
Radiofrequency ablation
Another promising alternative to surgical removal of primary lung tumors is radiofrequency ablation (RFA). A heating electrode is directly inserted into the tumor percutaneously under the guidance of CT, and alternating electrical currents are passed through the electrode into the neoplastic mass with the intent of inducing tumor cell necrosis.
In a study using animal models, transmissible venereal tumor fragments were injected into the lungs of five dogs, and the patients were subsequently subjected to site-directed RFA. After treatment, the dogs were euthanized, and lung lesions were histologically evaluated. All tumor lesions demonstrated complete thermal coagulative necrosis with no evidence of viable tumor cells. The damage to normal lung parenchyma involved only a narrow zone of hemorrhagic necrosis surrounding each ablated lesion.
The efficacy of RFA on primary pulmonary masses suggests that animals with metastatic pulmonary nodules may also benefit from this treatment modality. Such a supposition is supported by one study in which electrode placement in the epicenter of the cluster of nodules was adequate for complete nodule ablation.53
Localized therapy
The localized delivery of chemotherapeutic agents or cytokines to the thoracic cavity or lung parenchyma may allow for enhanced anticancer effects within the immediate tumor microenvironment.
Intracavitary chemotherapy. The clinical effectiveness of intracavitary cisplatin administration (50 mg/m2) has been investigated in six dogs with malignant cavitary effusions.54 In three dogs with pleural mesothelioma, complete resolution of cancerous effusions was achieved after a maximum of two treatments. These favorable anecdotal findings warrant further exploration of intracavitary chemotherapeutic strategies for managing the clinical consequences associated with primary or metastatic lung tumors.
A more recent study evaluated the effectiveness of intracavitary mitoxantrone or carboplatin for treating thoracic or abdominal carcinomatosis, sarcomatosis, or mesothelioma in patients with and without malignant effusions. In dogs treated with intracavitary chemotherapy, the median survival time was 332 days, compared with only 25 days in untreated dogs.55 These findings derived from a small population of cancer-bearing dogs also suggest that intracavitary chemotherapy exerts some beneficial anticancer effects.
Inhaled chemotherapy. Although intracavitary chemotherapy may increase the concentration of drug within the pleural space and at the visceral surface of the lung, the attainment of higher drug concentrations within the pulmonary parenchyma is better achieved through inhalation therapy. In a recent study, either doxorubicin or paclitaxel was delivered by aerosolization to 28 dogs with either primary or metastatic pulmonary neoplasia.56 Tumor regression occurred in 25% of dogs treated, with one patient demonstrating partial regression of metastatic hilar lymphadenopathy. Although typical toxicities of systemic doxorubicin chemotherapy (myelosuppression, nausea, and vomiting) were not seen, acute local pulmonary effects (intermittent, nonproductive cough) were noted in about half the dogs.
An important finding in this study was that dogs receiving inhalation doxorubicin on the same day as systemic doxorubicin did not experience any increase in systemic toxicosis, suggesting that inhaled doxorubicin exerted its effects locally.56 Thus, combining two different routes of chemotherapy administration may exert superior anticancer effects without added toxicity.56,57
Inhaled cytokines. Similar to the delivery of inhaled chemotherapy, the aerosol delivery of liposome-encapsulated IL-2 produced clinical responses in dogs with osteosarcoma metastases, with two of four patients achieving complete remission of their metastatic disease.57 Disappointingly, two dogs with primary lung tumors did not respond as well, with one achieving stable disease and the other experiencing progressive disease. Nonetheless, this study demonstrates that antitumor immune responses may be augmented through the delivery of aerosolized cytokines.57
SUMMARY
Primary lung tumors are uncommon in dogs and rare in cats. Most patients will not present with overt clinical signs of respiratory distress, but more commonly primary lung tumors will be incidental findings or will be the cause of nonspecific signs of illness, including weight loss and lethargy. Several predictive factors including tumor histologic subtype, size, and lymph node involvement have been demonstrated to aid in patient prognostication. Conventional therapeutic recommendations should include surgical resection of the primary tumor and draining lymph nodes, followed by adjuvant chemotherapy. In the near future, specialized local therapies such as IMRT and RFA may provide alternatives to surgery, and aerosolized chemotherapy may be used in conjunction with systemic drug administration to enhance overall anticancer effects. The net effect of these newer therapeutic options would be to provide longer disease-free intervals and survival times in dogs and cats with primary lung tumors.
Kerry C. Rissetto, DVM*
Pamela W. Lucas, DVM
Timothy M. Fan, DVM, PhD, DACVIM (small animal internal medicine, oncology)
Department of Veterinary Clinical Medicine
College of Veterinary Medicine
University of Illinois
Urbana, IL 61802-4714
*Current address: Department of Veterinary, Medicine and Surgery, College of Veterinary Medicine, University of Missouri-Columbia, Columbia, MO 65211
REFERENCES
1. Mehlhaff CJ, Mooney S. Primary pulmonary neoplasia in the dog and cat. Vet Clin North Am Small Anim Pract 1985;15(5):1061-1067.
2. McNiel EA, Ogilvie GK, Powers BE, et al. Evaluation of prognostic factors for dogs with primary lung tumors: 67 cases (1985-1992). J Am Vet Med Assoc 1997;211(11):1422-1427.
3. Ogilvie GK, Weigel RM, Haschek WM, et al. Prognostic factors for tumor remission and survival in dogs after surgery for primary lung tumors: 76 cases (1975-1985). J Am Vet Med Assoc 1989;195(1):109-112.
4. Ogilvie GK, Haschek WM, Withrow SJ, et al. Classification of primary lung tumors in dogs: 210 cases (1975-1985). J Am Vet Med Assoc 1989;195(1):106-108.
5. Wilson DW, Dungworth DL. Tumors of the respiratory tract. In: Meuten DJ, ed. Tumors of domestic animals. 4th ed. Ames: Iowa State Press, 2002;380-392.
6. Withrow SJ. Tumors of the respiratory system: lung cancer. In: Withrow SJ, Vail DM, eds. Withrow and MacEwen's small animal clinical oncology. 4th ed. Philadelphia, Pa: WB Saunders Co, 2007;517-525.
7. Paoloni MC, Adams WM, Dubielzig RR, et al. Comparison of results of computed tomography and radiography with histopathologic findings in tracheobronchial lymph nodes in dogs with primary lung tumors: 14 cases (1999-2002). J Am Vet Med Assoc 2006;228(11):1718-1722.
8. Mehlhaff CJ, Leifer CE, Patnaik AK, et al. Surgical treatment of pulmonary neoplasia in 15 dogs. J Am Anim Hosp Assoc 1984;20:799-803.
9. Milner RJ, Farese J, Henry CJ, et al. Bisphosphonates and cancer. J Vet Intern Med 2004;18(5):597-604.
10. Moulton JE, von Tscharner C, Schneider R. Classification of lung carcinomas in the dog and cat. Vet Pathol 1981;18(4):513-528.
11. Fan TM, de Lorimier LP, Charney SC, et al. Evaluation of intravenous pamidronate administration in 33 cancer-bearing dogs with primary or secondary bone involvement. J Vet Intern Med 2005;19(1):74-80.
12. Brodey RS, Craig PH. Primary pulmonary neoplasms in the dog: a review of 29 cases. J Am Vet Med Assoc 1965;147(12):1628-1643.
13. Nielsen SW, Horava A. Primary pulmonary tumors of the dog: a report of sixteen cases. Am J Vet Res 1960;21:813-830.
14. Koblik PD. Radiographic appearance of primary lung tumors in cats. Vet Radiol 1986;27:66-73.
15. Hahn FF, Muggenburg BA, Griffith WC. Primary lung neoplasia in a beagle colony. Vet Pathol 1996;33(6):633-638.
16. Hahn KA, McEntee MF. Primary Lung tumors in cats: 86 cases (1979-1994). J Am Vet Med Assoc 1997;211(10):1257-1260.
17. Reif JS, Dunn K, Ogilvie GK, et al. Passive smoking and canine lung cancer risk. Am J Epidemiol 1992;135(3):234-239.
18. Suter PF, Carrig CB, O'Brien TR, et al. Radiographic recognition of primary and metastatic pulmonary neoplasms of dogs and cats. Vet Radiol Ultrasound 1974;15:3-24.
19. Barr F, Gruffydd-Jones T, Brown P, et al. Primary lung tumors in the cat. J Small Anim Pract 1987;28:1115-1125.
20. Watson AD, Young KM, Dubielzig RR, et al. Primary mesenchymal or mixed-cell-origin lung tumors in four dogs. J Am Vet Med Assoc 1993;202(6):968-970.
21. Seiler RJ. Primary pulmonary osteosarcoma in dog with associated hypertrophic osteopathy. Vet Pathol 1979;16(3):369-371.
22. Weller RE, Dagle GE, Perry RL, et al. Primary pulmonary chondrosarcoma in a dog. Cornell Vet 1992;82(4):447-452.
23. Stephens LC, Gleiser CA, Jardine JH. Primary pulmonary fibrosarcoma associated with Spirocerca lupi infection in a dog with hypertrophic pulmonary osteoarthropathy. J Am Vet Med Assoc 1983;182(5):496-498.
24. Postorino NC, Wheeler SL, Park RD, et al. A syndrome resembling lymphomatoid granulomatosis in the dog. J Vet Intern Med 1989;3(1):15-19.
25. Fitzgerald SD, Wolf DC, Carlton WW. Eight cases of canine lymphomatoid granulomatosis. Vet Pathol 1991;28(3):241-245.
26. Berry CR, Moore PF, Thomas WP, et al. Pulmonary lymphomatoid granulomatosis in seven dogs (1976-1987). J Vet Intern Med 1990;4(3):157-166.
27. Hahn KA, McEntee MF. Prognosis factors for survival in cats after removal of a primary lung tumor: 21 cases (1979-1994). Vet Surg 1998;27(4):307-311.
28. Biery DN. Differentiation of lung diseases of inflammatory or neoplastic origin from lung disease in heart failure. Vet Clin North Am 1974;4:711-721.
29. Reif JS. Solitary pulmonary lesions in small animals. J Am Vet Med Assoc 1969;155(5):717-722.
30. DeBerry JD, Norris CR, Samii VF, et al. Correlation between fine-needle aspiration cytopathology and histopathology of the lung in dogs and cats. J Am Anim Hosp Assoc 2002;38(4):327-336.
31. McMillan MC, Kleine LJ, Carpenter JL. Fluoroscopically guided percutaneous fine-needle aspiration biopsy of thoracic lesions in dogs and cats. Vet Radiol 1988;29:195-197.
32. Teske E, Stokhof AA, van den Ingh TS, et al. Transthoracic needle aspiration biopsy of the lung in dogs and cats with pulmonic disease. J Am Anim Hosp Assoc 1991;27:289-294.
33. Wood EF, O'Brien RT, Young KM. Ultrasound-guided fine-needle aspiration of focal parenchymal lesions of the lung in dogs and cats. J Vet Intern Med 1998;12(5):338-342.
34. Unver E, Yilmaz A, Aksoy F, et al. Does needle size affect yield of transthoracic needle biopsy in malignant pulmonary lesions? Comparison of 18-, 22-, and 25-gauge needles in surgical specimens. Respirology 2006;11(5):648-651.
35. Menard M, Papageorges M. Ultrasound corner technique for ultrasound-guided fine needle biopsies. Vet Radiol Ultrasound 1995;36:137-138.
36. Hawkins EC, DeNicola DB, Kuehn NF. Bronchoalveolar lavage in the evaluation of pulmonary disease in the dog and cat. J Vet Intern Med 1990;4(5):267-274.
37. Norris CR, Griffey SM, Samii VF, et al. Comparison of results of thoracic radiography, cytologic evaluation of bronchoalveolar lavage fluid, and histologic evaluation of lung specimens in dogs with respiratory tract disease: 16 cases (1996-2000). J Am Vet Med Assoc 2001;218(9):1456-1461.
38. Norris CR, Griffey SM, Samii VF, et al. Thoracic radiography, bronchoalveolar lavage cytopathology, and pulmonary parenchymal histopathology: a comparison of diagnostic results in 11 cats. J Am Anim Hosp Assoc 2002;38(4):337-345.
39. Nemanic S, London CA, Wisner ER. Comparison of thoracic radiographs and single breath-hold helical CT for detection of pulmonary nodules in dogs with metastatic neoplasia. J Vet Intern Med 2006;20(3):508-515.
40. Castellano MC, Massone AR, Idiart JR. Primary pulmonary adenocarcinoma metastatic to the uvea, brain and adrenal gland in a dog. J Vet Med A Physiol Pathol Clin Med 2006;53(4):194-197.
41. Ibarrola P, German AJ, Stell AJ, et al. Appendicular arterial tumor embolization in two cats with pulmonary carcinoma. J Am Vet Med Assoc 2004;225(7):1065-1069, 1048-1049.
42. van der Linde-Sipman JS, van den Ingh TS. Primary and metastatic carcinomas in the digits of cats. Vet Q 2000;22(3):141-145.
43. Bertazzolo W, Zuliani D, Pogliani E, et al. Diffuse bronchiolo-alveolar carcinoma in a dog. J Small Anim Pract 2002;43(6):265-268.
44. Sharkey LC, Rosol TJ, Grone A, et al. Production of granulocyte colony-stimulating factor and granulocyte-macrophage colony-stimulating factor by carcinomas in a dog and a cat with paraneoplastic leukocytosis. J Vet Intern Med 1996;10(6):405-408.
45. Anderson TE, Legendre AM, McEntee MM. Probable hypercalcemia of malignancy in a cat with bronchogenic adenocarcinoma. J Am Anim Hosp Assoc 2000;36(1):52-55.
46. Dole RS, MacPhail CM, Lappin MR. Paraneoplastic leukocytosis with mature neutrophilia in a cat with pulmonary squamous cell carcinoma. J Feline Med Surg 2004;6(6):391-395.
47. Hogan DF, Dhaliwal RS, Sisson DD, et al. Paraneoplastic thrombocytosis-induced systemic thromboembolism in a cat. J Am Anim Hosp Assoc 1999;35(6):483-486.
48. Lansdowne JL, Monnet E, Twedt DC, et al. Thoracoscopic lung lobectomy for treatment of lung tumors in dogs. Vet Surg 2005;34(5):530-535.
49. Lin J, Iannettoni MD. The role of thoracoscopy in the management of lung cancer. Surg Oncol 2003;12(3):195-200.
50. Poirier VJ, Burgess KE, Adams WM, et al. Toxicity, dosage, and efficacy of vinorelbine (Navelbine) in dogs with spontaneous neoplasia. J Vet Intern Med 2004;18(4):536-539.
51. Krikorian A, Rahmani R, Bromet M, et al. Pharmacokinetics and metabolism of Navelbine. Semin Oncol 1989;16(2 suppl 4):21-25.
52. Ballegeer EA, Forrest LJ, Jeraj R, et al. PET/CT following intensity-modulated radiation therapy for primary lung tumor in a dog. Vet Radiol Ultrasound 2006;47(2):228-233.
53. Ahrar K, Price RE, Wallace MJ, et al. Percutaneous radiofrequency ablation of lung tumors in a large animal model. J Vasc Interv Radiol 2003;14(8):1037-1043.
54. Moore AS, Kirk C, Cardona A. Intracavitary cisplatin chemotherapy experience with six dogs. J Vet Intern Med 1991;5(4):227-231.
55. Charney SC, Bergman PJ, McKnight JA, et al. Evaluation of intracavitary mitoxantrone and carboplatin for treatment of carcinomatosis, sarcomatosis, and mesothelioma, with or without malignant effusions: a retrospective analysis of 12 cases (1997-2002). Vet Comp Oncol 2005;3:171-181.
56. Hershey AE, Kurzman ID, Forrest LJ, et al. Inhalation chemotherapy for macroscopic primary or metastatic lung tumors: proof of principle using dogs with spontaneously occurring tumors as a model. Clin Cancer Res 1999;5(9):2653-2659.
57. Khanna C, Vail DM. Targeting the lung: preclinical and comparative evaluation of anticancer aerosols in dogs with naturally occurring cancers. Curr Cancer Drug Targets 2003;3(4):265-273.
58. Dorn CR, Taylor DO, Frye FL, et al. Survey of animal neoplasms in Alameda and Contra Costa Counties, California. I. Methodology and description of cases. J Natl Cancer Inst 1968;40(2):295-305.
59. Theilen GH, Madewell BR. Tumors of the respiratory tract and thorax. In: Theilen GH, Madewell BR, eds. Veterinary cancer medicine. Philadelphia, Pa: Lea and Febiger, 1979;341-346.
60. Clements DN, Hogan AM, Cave TA. Treatment of a well differentiated pulmonary adenocarcinoma in a cat by pneumonectomy and adjuvant mitoxantrone chemotherapy. J Feline Med Surg 2004;6(3):199-205.