When things go wrong in cancer management: Managing adverse effects of cancer chemotherapy (Proceedings)
Most cytotoxic chemotherapy protocols in common veterinary use are designed to have a low risk of adverse effects.
Most cytotoxic chemotherapy protocols in common veterinary use are designed to have a low risk of adverse effects (AE). In general, less than 1 in 4 animals will have an unpleasant AE and only approximately 3 - 5% will have a serious AE, leading to hospitalization. There are several important consequences of a serious AE, including decreased quality of life, financial consequences (e.g., hospitalization and treatment), delay or reduction of subsequent effective treatments, and diminished client enthusiasm for continuation of therapy. With appropriate intervention, the risk of a treatment-associated fatality is less than 1 in 200. Should a serious AE occur, doses can be reduced, drugs can be substituted, or additional medications dispensed to minimize the likelihood of further AEs occurring. These changes are effective 90% of the time. Studies assessing clients' perceptions of medical treatment for cancer generally report a positive experience; most owners felt the treatment was worthwhile, that it resulted in improvement in the well-being of their pet, and that quality of life during treatment was good.
In practices where chemotherapy is administered, having a protocol in place for the treatment of patients experiencing AEs dramatically increases the likelihood of a good outcome and increased client satisfaction should one be encountered. It is the responsibility of the clinician to ensure the client understands the goals of therapy in each individual case before emotion, time and money are invested in therapy. Use of client education handouts explaining the potential toxicities, how to manage them and when to become concerned should be encouraged.
Breed Predisposition to Adverse Effects of Chemotherapy
Certain breeds, particularly collie breeds, are considered at risk for excessive toxicity from cancer drugs that are actively transported by the p-glycoprotein (P-GP) pump (e.g., vinca alkaloids, DOX, dactinomycin, and the taxanes). These breeds have a high frequency of a germline mutation of the MDR1 allele. This mutation diminishes the excretion of P-GP substrate chemotherapy drugs, leading to increased drug exposure to the patient. If a dog is homozygous for the mutant allele, they will be affected and at risk; if heterozygous, it is a carrier. The frequency of these mutations has been characterized in several breeds in different geographic locations and are presented in table 1. A genotyping assay (performed on cheek swabs) for mutation status is available through the laboratory of Dr. Katrina Mealey at Washington State University College of Veterinary Medicine. P-GP substrate drugs should be avoided if at all possible in dogs homozygous for the MDR1 mutation. If their use is unavoidable, significant dose reductions should be performed.
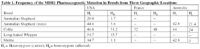
Table 1. Frequency of the MDR1 Pharmacogenetic Mutation in Breeds from Three Geographic Locations
The most commonly encountered AEs generally occur as a result of "collateral damage" to rapidly dividing cells by the cytotoxic agent. Both bone marrow stem cells and gastrointestinal crypt cells are rapidly dividing and thus sensitive to the antiproliferative effects of cytotoxic chemotherapy.
Hair Loss
Most breeds experience little or no hair loss; typically only the non-shedding breeds (poodles, old English sheepdogs, terrier breeds) loose significant amounts of hair although the owners may find more hair around the house. Hair loss from chemotherapy is non-itchy and nonpainful – it is a purely cosmetic change. Hair that is lost will typically begin to regrow following the completion of therapy. Cats may lose whiskers and the long, stiff "guard hairs" of their coat.
Gastrointestinal Effects
The majority are mild and self-limiting, however more severe episodes are occasionally encountered. Gastrointestinal (GI) toxicity may be secondary to direct damage to intestinal epithelial cells or via efferent nervous stimulation of the chemoreceptor trigger zone (CRTZ). Certain drugs, such as cisplatin, have the potential to cause nearly immediate nausea/vomiting due to the activity of the drug on the chemoreceptor trigger zone in the brain. More commonly, gastrointestinal effects are delayed as damage to the GI mucosa can result in irritation and inflammation that can lead to vomiting (so called delayed chemotherapy-induced nausea and vomiting [CINV]) and/or diarrhea, classically 2 to 5 days following chemotherapy administration. It typically manifests as inappetence, nausea, vomiting, and/or diarrhea beginning 3 to 5 days after therapy. The consequences of significant gastrointestinal adverse events are several fold and include dehydration, nutritional deficiency, delay of subsequent therapy, dose reduction, financial burden (i.e., hospitalization) and diminished client enthusiasm for continuation. The judicious use of antiemetics and antidiarrheals is recommended. If an animal is to be given a protocol with a high likelihood of creating nausea or vomiting or has had significant gastrointestinal events following a particular chemotherapy, sending the client home with 3 – 5 days of prophylactic therapy is indicated. The most effective class of antiemetics in people undergoing chemotherapy are the NK1 receptor antagonists; Cerenia® (Maropitant), recently receiving FDA approval for use in dogs also is a superior antiemetic in dogs receiving chemotherapy and has several advantages to off-label antiemetics used in the past. It is important to keep in mind that most side effects of chemotherapy are self-limiting and will resolve with minimal veterinary intervention. Most clients are able to perform the nursing care required to support animals through GI side effects. Typically, dose reductions of 20% are recommended for severe gastrointestinal toxicity at the time of the next scheduled treatment. Dose reductions should not be contemplated lightly as dose intensity is extremely important for antitumor response; therefore, if adverse effects can be abrogated by symptomatic treatments (antiemetics, antidiarrheals) rather than dose reduction, this should be attempted first.
Oral medications for diarrhea such as loperamide (0.08 mg/kg PO TID) may be used as well. Some animals with chemotherapy-associated diarrhea may respond to oral metronidazole (15 - 25 mg/kg daily) for 5 days.
Neutropenia and Sepsis
Neutropenia is likely to be seen 7-10 days after the administration of most chemotherapy drugs. Exceptions to this rule include vinblastine and paclitaxel, which can cause neutropenia as early as 4-5 days after administration, and carboplatin, which can occasionally cause neutropenia as late as 2-3 weeks following administration. Most companion animals have a low risk of infection if their neutrophil count remains greater than 1,000/uL.The severity of neutropenia and associated sepsis can be extremely variable, ranging from clinically silent to overwhelming and fatal. Compounding the potential seriousness of this, the timing of chemotherapy induced neutropenia usually occurs concurrently with the height of gastrointestinal damage from chemotherapy. Gastrointestinal changes can include micro-ulcerations and loss of the normal "feeder layer" of desquamated cells, saliva and mucous. These changes create a favorable environment for bacterial overgrowth, translocation, and invasion by aerobic gram negative bacilli and gram positive cocci.
Classification of Neutropenia
Patients with chemotherapy induced neutropenia are classified into two categories based on clinical presentation. Category I Neutropenia: This is the most common type encountered and represent animals that show no outward signs of illness; they continue to eat and drink and do not have a fever. Category II Neutropenia: These are patients that present with neutropenia and are clinically ill including inappetence, depression and fever.
Managing Category I Neutropenia
Asymptomatic patients with less than 1,000 neutrophils/uL can be managed on an outpatient basis. In these patients, the risk of nosocomial infection probably outweighs the benefit associated with hospitalization. Prophylactic oral antibiotics have been shown to decrease the risk of bacteremia and sepsis-associated mortality in afebrile neutropenic human cancer patients. A broad-spectrum oral antibiotic that spares normal anaerobic gastrointestinal flora such as trimethoprim-sulfa (7.5 mg/kg BID) or a fluoroquinalone (e.g., enrofloxacin, 5-10 mg/kg SID) should be prescribed for a 5-7 day course. Anaerobe-sparing antibiotics are preferred as they help prevent aerobic gram negative bacilli and gram positive cocci overgrowth and invasion in the chemotherapy weakened gastrointestinal tract. The owner should be instructed to monitor the patient's temperature once or twice daily at home. If the patient becomes clinically ill or the temperature exceeds 103.5o C, hospitalization may be required. Afebrile patients with mild neutropenia (>1,000/uL) generally require no treatment.
Managing Category II Neutropenia
Septic patients are often febrile, as mentioned above. Other physical abnormalities could include tachycardia, injected mucous membranes, slow or prolonged capillary refill, or weak pulses. Initial minimum database should include a complete blood count (CBC) and platelet count with manual differential, serum biochemistry profile, and urinalysis. Urinalysis may reveal a quiet sediment, however urinary tract infections cannot be ruled out as neutropenia can result in the absence of white blood cells in the urine. Some clinicians will empirically culture the urine of neutropenic, potentially septic patients. A coagulation profile is indicated in an animal with unquestionable signs of septic shock, as varying degrees of disseminated intravascular coagulation can be present and must be treated aggressively. In animals presenting with respiratory signs or with a history of vomiting prior to presentation, thoracic radiographs to identify a nidus of infection are indicated. Recent human studies suggest that there is no benefit to obtaining "screening" thoracic radiographs in the asymptomatic neutropenic, septic patient. Febrile or systemically ill patients should be hospitalized for 24-hour care. The first line of treatment for these patients is intravenous crystalloid therapy; a fluid rate of 1.5 times maintenance is reasonable after correction of any existing fluid deficit. It is common for fever and clinical status to improve significantly after several hours of fluid therapy. Clinical experience suggests that most bacteria implicated in septic veterinary cancer patients are sensitive to commonly used antibiotics. Intravenous coverage for both gram-positive and gram-negative organisms should be employed. Unlike the scenario outlined above for afebrile neutropenic patients, both anaerobic and aerobic bacteria should be targeted in the sick, febrile neutropenic patient. Typical drug combinations might include a penicillin/aminoglycoside combination such as ampicillin (22 mg/kg IV TID) and amikacin (10 mg/kg IV/IM/SQ SID) (assuming renal function is adequate) or first-generation cephalosporin/fluoroquinolone combination such as cefazolin (20 mg/kg IV TID) and enrofloxacin (5-10 mg/kg IV or IM SID). Antipyretics are almost never necessary, and may make interpretation of response to therapy difficult.
The majority of patients will respond rapidly to therapy, and neutrophil counts may rise very rapidly as well. Most will be afebrile within 12-24 hours, and can be discharged when they are afebrile and their neutrophil count is shown to be rising. In patients that do not respond clinically during the first 24-48 hours, further diagnostics to identify a potential nidus of infection and to collect samples for bacterial culture and antibiotic sensitivity should be performed. Additional tests include thoracic radiographs, abdominal ultrasound and echocardiography, and at least 2 sets of blood cultures. In those patients that do not respond rapidly, antibiotic coverage can be broadened while waiting for culture results. Anaerobic coverage may be broadened with the addition of metronidazole (15 mg/kg IV BID), and/or a second- or third-generation cephalosporin can be considered. Should protracted (>72h) neutropenia be encountered, a bone marrow aspirate may be useful, especially in patients with hematopoietic neoplasia where there is the possibility of bone marrow infiltration (myelophthisis).
There is continued debate as to the clinical utility of recombinant human granulocyte colony-stimulating factor (G-CSF, Neupogen®). Some clinicians will routinely utilize G-CSF for febrile, neutropenic patients; others will utilize it in cases of severe neutropenia where neutrophil count is less than some arbitrary value (500/uL or 100/uL, for example). Others will utilize G-CSF only if neutropenia persists for longer than 72 hours. Most human studies have suggested no benefit in terms of length of hospitalization or mortality rate if G-CSF is employed after neutropenic fever has developed, and in the authors' hands, G-CSF is almost never necessary.
Prevention of subsequent neutropenic events
Dose reductions are not to be considered lightly as dose intensity is extremely important for antitumor response. Generally, a dose reduction by 20% is recommended if the neutrophil count is ≤ 500/μL at the nadir or < 1500/μL at the next scheduled treatment interval (which should be delayed until a the neutrophil count rebounds to >1500/μL). Occasionally, one particular drug or drug class in not tolerated by an individual patient and substitutions are made. Dose reductions are sometimes also made based on the clients level of comfort with the severity of AEs.
Perivascular Necrosis
Several chemotherapeutic agents (e.g., doxorubicin [DOX], the vinca alkaloids, actinomycin D) are vesicants that can cause tissue damage if delivered extravascularly. Administration of vesicants should be through a perfectly placed "first stick" intravenous catheter. Dogs undergoing vesicant infusions should be constantly observed until completion of the infusion to ensure a patent catheter and successful infusion. Doxorubicin is an extremely potent vesicant; if extravasated, it is extremely damaging. Surgical treatment, including immediate debridement of the extravasated tissues and potentially amputation, may be required. The free-radical scavenging drug dexrazoxane (Zinecard®, Pfizer), marketed for the prevention of DOX-associated cardiotoxicity, has been shown to abrogate the tissue damage associated with extravasation if given immediately after extravasation (and possibly within 3 hours of infusion) in mice. Anecdotally, IV administration of dexrazoxane at 10 times the dose of DOX within 3 hours and again at 24 and 48 hours after extravasation may significantly reduce local tissue injury. Additionally, the application of 99% DMSO topically, every 8 hours for 2 weeks may abrogate some the effects.
Anaphylaxis
Several chemotherapeutic agents are capable of producing immediate anaphylaxis or anaphylactoid reactions in patients. These include asparaginase, DOX and, in particular, the taxanes. The shock organs of the dog are the gastrointestinal tract and skin, and these two organs are most severely affected during and immediately after administration. The lung is the shock organ in the cat. Should adverse acute drug reactions occur during infusion of DOX (e.g. pruritus, facial edema, wheals, erythema of skin and mucous membranes, head shaking, vomiting, restlessness, dyspnea), the administration is stopped, diphenhydramine (3-4 mg/kg IM) and dexamethasone SP (0.5–1.0 mg/kg IV) are administered. When the reaction subsides, administration can be resumed at a slower rate. Asparaginase can result in anaphylaxis, usually within 60 minutes of injection; therefore, animals should be monitored for hypersensitivity reactions for 60 minutes following drug administration. The likelihood of these reactions increases with multiple asparaginase injections. For animals demonstrating anaphylaxis from a previous drug treatment, it is prudent to premedicate with diphenhydramine and dexamethasone 15 to 20 minutes prior to subsequent treatments.