Antibiotics in canine GI disease: when to use and when to ditch
Antimicrobials may be prescribed due to convenience, habit or good intentions, but in the absence of evidence to support their use, they should be avoided in systemically healthy animals. Here’s why.
Ksenia / stock.adobe.com

Antibiotics are often prescribed for dogs with gastrointestinal (GI) signs. In fact, three studies surveying veterinary prescribing habits in the U.K. showed that antimicrobials were prescribed as first-choice therapy in 50% or more of dogs presenting with acute diarrhea.1-3 While antibiotics can certainly be beneficial or even lifesaving for some dogs with GI disease, for others these drugs are unnecessary and may even be harmful.
Potential adverse effects
Antimicrobial resistance. As antimicrobial resistance becomes an ever-pressing concern in modern human medicine, there has been a growing movement in veterinary medicine to promote appropriate and judicious use of antibiotics.4-6 Oral administration of antibiotics may lead to the rapid development of resistant strains in the GI tract; cross-resistance to other antimicrobial agents can also occur.7
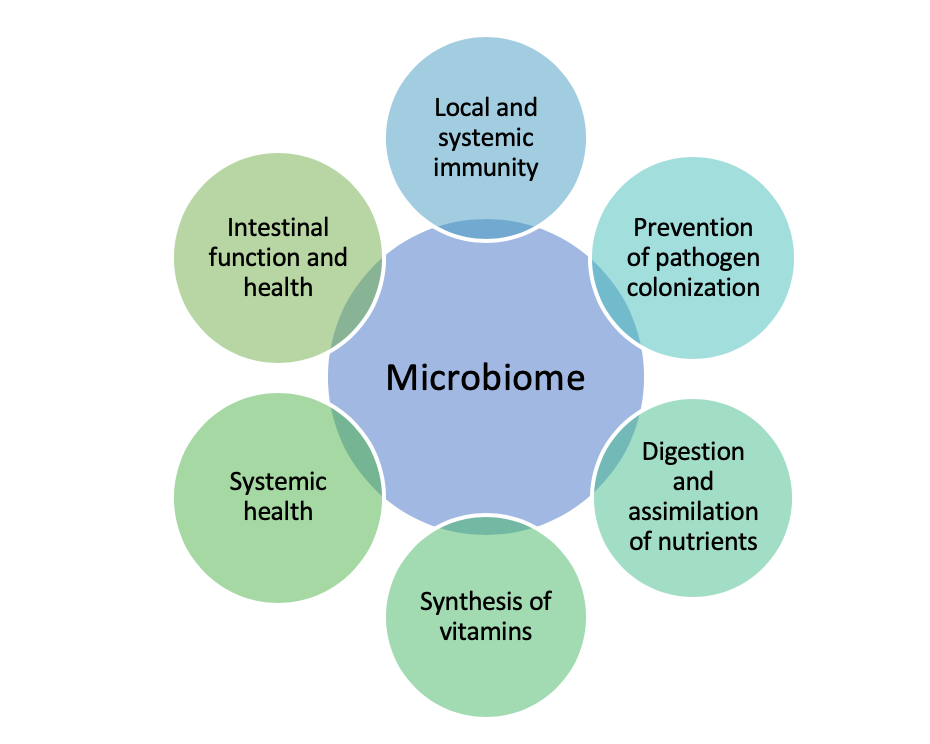
Effects on the microbiome. Opinions vary about the short- and long-term effects of antibiotics on the microbiome, which plays an important role in health and immunity, but it’s clear that concern is warranted (Figure 1). In one study, metronidazole was shown to cause a transient decrease in pathogenic bacteria and an increase in beneficial bacteria,8 but a different study showed that the fecal dysbiosis index was significantly increased in healthy dogs receiving metronidazole, indicating significant alterations in the microbiome structure and diversity, with some changes remaining up to 4 weeks after the completion of antibiotic administration.9 (The fecal dysbiosis index is a polymerase chain reaction [PCR] assay that quantifies the abundances of various bacterial groups, with values < 0 indicating a normal fecal microbiota and values > 0 indicating dysbiosis.)
Figure 1. Benefits of the gastrointestinal microbiome.
Fenbendazole has no significant effects on the microbiome of healthy dogs, 10 but tylosin, another commonly prescribed medication for GI disease, can have prolonged effects.11 In one study, healthy dogs receiving standard doses of oral tylosin had significantly increased fecal dysbiosis indices, persisting for at least 2 months in some dogs.12 Although none of the dogs in these studies had (or developed) GI signs, the effects of antibiotics on the microbiome warrant further investigation.
Long-term consequences. While we know antibiotic use affects the microbiome, we do not know the potential long-term consequences. Links have been found in humans between antibiotic exposure early in life and the development of various diseases, such as inflammatory bowel disease and allergies.13-15 Thus, it is reasonable to be concerned that antibiotic use in our own patients—especially young, growing dogs—might suffer similar consequences.
Antibiotics in specific conditions
Uncomplicated acute diarrhea in dogs has many possible causes, but a primary bacterial etiology is uncommon. Although diarrhea is often self-limiting, antibiotics are sometimes prescribed by practitioners in an effort to expedite recovery.
Studies evaluating whether antibiotics have a discernible effect on time to resolution of diarrhea in dogs have had mixed results. One study failed to identify a significant difference in time to recovery in dogs treated with metronidazole compared with placebo,16 and another found that metronidazole hastened resolution of diarrhea by about 1.5 days (both groups in this study recovered quickly).17 A large, retrospective observational study found that dietary modification and nutraceuticals (which included probiotics) were positively associated with resolution of acute diarrhea, but no such association was found with pharmaceutical agents (including antibiotics).3
Given that there is minimal (if any) proven benefit of antibiotic use in dogs with uncomplicated acute diarrhea, there is no basis to support the routine prescription and use of antibiotics in these cases.
Canine parvovirosis has a tropism for rapidly dividing cells, including those of the intestinal crypt epithelium, which leads to a severe enteritis. This, paired with the neutropenia that classically occurs with this disease, places patients at risk for bacterial and endotoxin translocation, which can result in bacteremia, systemic inflammatory response syndrome (SIRS) or multiorgan dysfunction. For this reason, broad-spectrum antibiotics are warranted in neutropenic patients suffering from canine parvovirus infection.
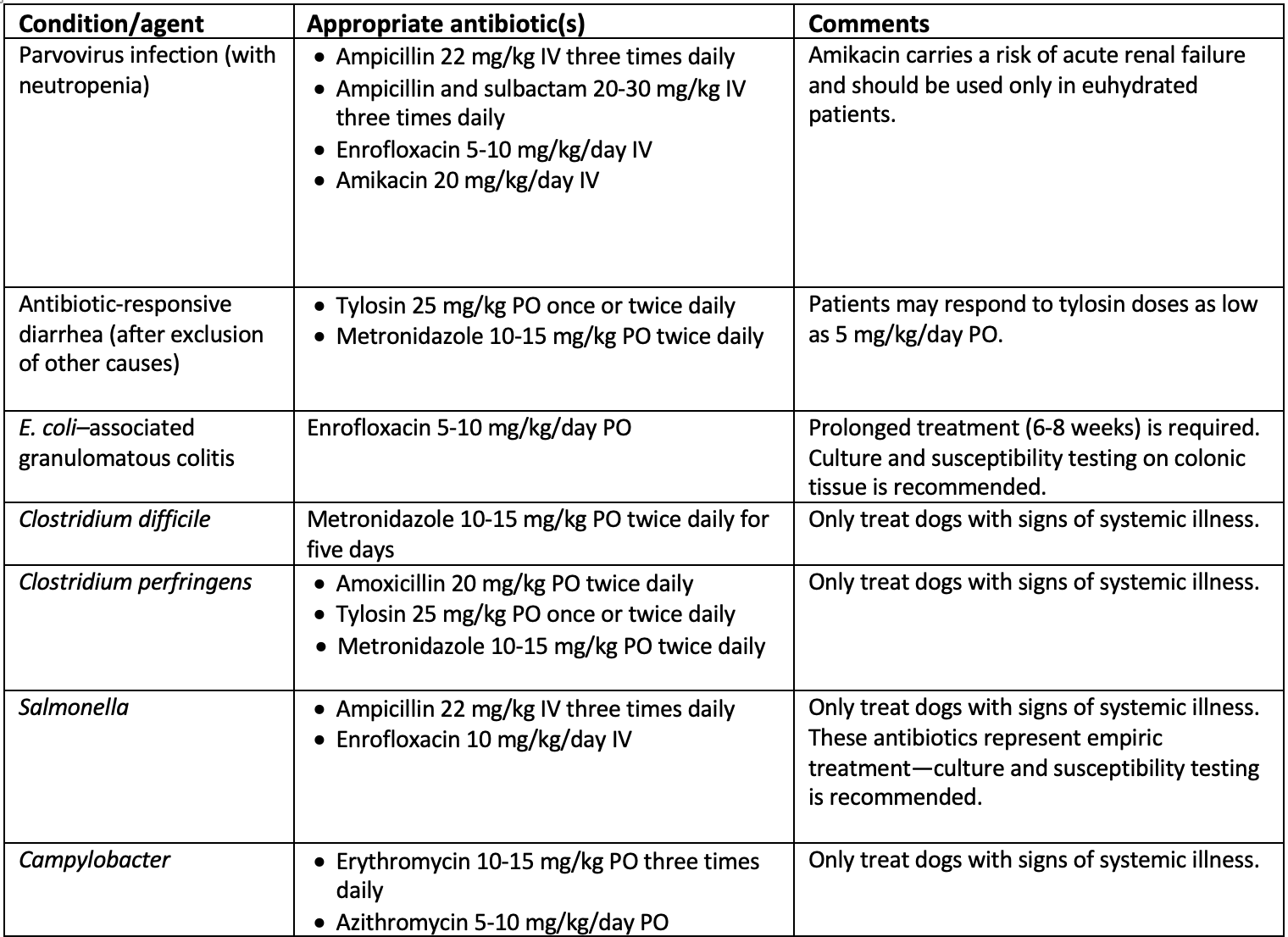
Typically, a beta-lactam antibiotic (ampicillin 22 mg/kg IV three times daily) is used, alone or in conjunction with enrofloxacin (5-10 mg/kg/day IV); see Table 1. Enrofloxacin may cause cartilage damage in young, growing animals, but this is rare with standard doses. Aminoglycosides can also be considered in well-hydrated dogs, but its use carries a risk of acute renal failure.
Table 1. Indications, antibiotic agents, and doses for treating GI disease in dogs
Acute hemorrhagic diarrhea syndrome (AHDS), formerly known as hemorrhagic gastroenteritis, is associated with a small intestinal overgrowth of Clostridium perfringens,18 although it should be noted that this organism is present consistently in the feces of healthy dogs. The netF toxin gene produced by C. perfringens might play an important role in the pathogenesis of this disease. Although there is no significant difference in C. perfringens encoding for the alpha toxin or enterotoxin between dogs with AHDS, parvovirus, or healthy controls, a significantly greater number of dogs with AHDS have the netF toxin gene.19 While the presence of netF gene in fecal samples supports C. perfringens–associated AHDS, there is no difference in outcome between netF-positive and netF-negative dogs. It should also be noted that there is a 10% to 12% prevalence of this gene in nonspecific diarrhea cases and healthy controls, and about 50% of dogs with AHDS are netF negative.
There is no significant difference in the recovery and outcome of dogs treated with or without amoxicillin/clavulanic acid,20 and in a study evaluating the effects of a probiotic on the clinical course of AHDS, dogs made a rapid recovery without antibiotics.21 For this reason, unless evidence of sepsis exists (such as fever or toxic change of neutrophils on a leukogram), antimicrobials are unlikely to be necessary for the treatment of this syndrome.
Dogs with AHDS that do not receive antibiotics have a good prognosis and rapid recovery, despite roughly one-third of these patients meeting two or more SIRS criteria.22 This suggests that standard SIRS criteria alone may not be strict enough to guide appropriate use of antimicrobials.
Antibiotic-responsive diarrhea (ARD) describes a chronic (> 3 weeks) enteropathy for which no underlying cause is found and which is completely responsive to antibiotic treatment. Classically, ARD is seen in young, large-breed dogs, with German shepherds being overrepresented. It is characterized by chronic intermittent diarrhea as well as weight loss, a variable appetite, and possible vomiting.
The diagnosis is based on a positive response to therapy, exclusion of other diseases (e.g. exocrine pancreatic insufficiency in a young German shepherd with weight loss and diarrhea) and a demonstration of disease relapse when antibiotics are withdrawn. Excluding other diseases is important as many of them may improve temporarily with antibiotics; thus a positive response to therapy does not negate the need for appropriate workup.
About two-thirds of dogs with chronic enteropathies have food-responsive enteropathies, with ARD and steroid-responsive diarrhea making up the remaining third.23,24 Dogs with food-responsive diarrhea have better outcomes than dogs with either ARD or steroid-responsive disease. Therefore, an antibiotic trial should be considered only after a strict diet trial (hydrolyzed protein or novel protein diet) for a minimum of 3 weeks with no response.23
The antibiotics recommended for treatment of ARD are metronidazole (10-15 mg/kg PO twice daily) and tylosin (25 mg/kg PO once or twice daily). Some dogs respond specifically to tylosin,25 so it may make more sense to look to tylosin before metronidazole in an antibiotic trial for a chronic enteropathy. Response to therapy should be quick (within 2 weeks), and dogs with a positive response to tylosin at 25 mg/kg/day might respond to doses as low as 5 mg/kg/day.26 Thus, dose reduction can be considered following a positive response to the standard dose.
As noted earlier, ARD is definitely diagnosed when relapse occurs following antibiotic withdrawal and clinical signs resolve when the antibiotic is re-introduced.27 That said, not all dogs require lifelong therapy and periodic withdrawal of antibiotics should be attempted to determine whether ongoing therapy is necessary.
Escherichia coli–associated granulomatous colitis is characterized histologically by granulomatous inflammation with periodic acid-Schiff–positive macrophages. This disease classically is seen in young boxer dogs or French bulldogs.28 Patients usually present with a combination of colitis, hematochezia and weight loss.
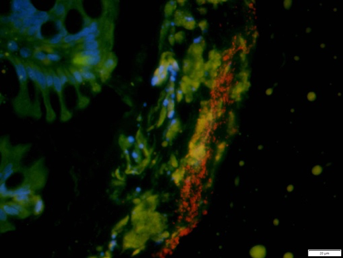
With the use of fluorescence in situ hybridization (FISH; Figure 2), mucosally invasive E. coli was identified as the likely cause of this disease. Long-term remission is associated with eradication of the bacteria.29,30 Typically, it is treated with a long course of fluoroquinolones, such as enrofloxacin (5-10 mg/kg/day for six to eight weeks). This disease has been identified in a variety of other breeds and even in cats, with reported remission with fluoroquinolone therapy.31 However, resistance of E. coli to fluoroquinolones has been demonstrated. Therefore, bacterial culture and sensitivity testing of the tissue is recommended. Due to the potential for the development of antimicrobial resistance, empiric therapy for this disease is not recommended.
Figure 2. Fluorescence in situ hybridization of the colonic tissue of an 11-year-old male castrated boxer. Note the abundant mucus-associated rods (red) with no adherent or invasive bacteria, indicating that this dog did not have E. coli–associated granulomatous colitis.
Enteropathogenic bacteria (and/or their toxins) are often detected today using fecal PCR panels, which allow for the identification of organisms such as Clostridium difficile, C. perfringens, Campylobacter spp. and Salmonella spp., among others. An ACVIM consensus article regarding enteropathogenic bacteria offers a more detailed discussion on this topic.6
As these organisms can be found in both healthy animals and in those with diarrhea, interpretation of the results of these panels can be confusing. For some organisms, identification of enterotoxin genes may be more helpful. Enterotoxin genes are produced by both C. perfringens and C. difficile and are found more frequently in dogs with diarrhea than in those without.
Clinically, many of these cases will present as self-limiting diarrhea that does not require antimicrobial therapy. In fact, overuse of antibiotics in these scenarios may promote drug-resistant organisms.
Conversely, if a patient presents with systemic signs of illness (e.g. fever, toxic changes or a degenerative left shift) and is diagnosed with an enteropathogenic bacteria, appropriate antibiotic therapy may be warranted.
Despite the zoonotic potential of Salmonella and Campylobacter spp., antimicrobial therapy is not indicated in nonclinical or mildly affected dogs. This recommendation remains the same even with an immunocompromised owner. In this case, appropriate husbandry and hygiene become the more important aspects of management.
Conclusions
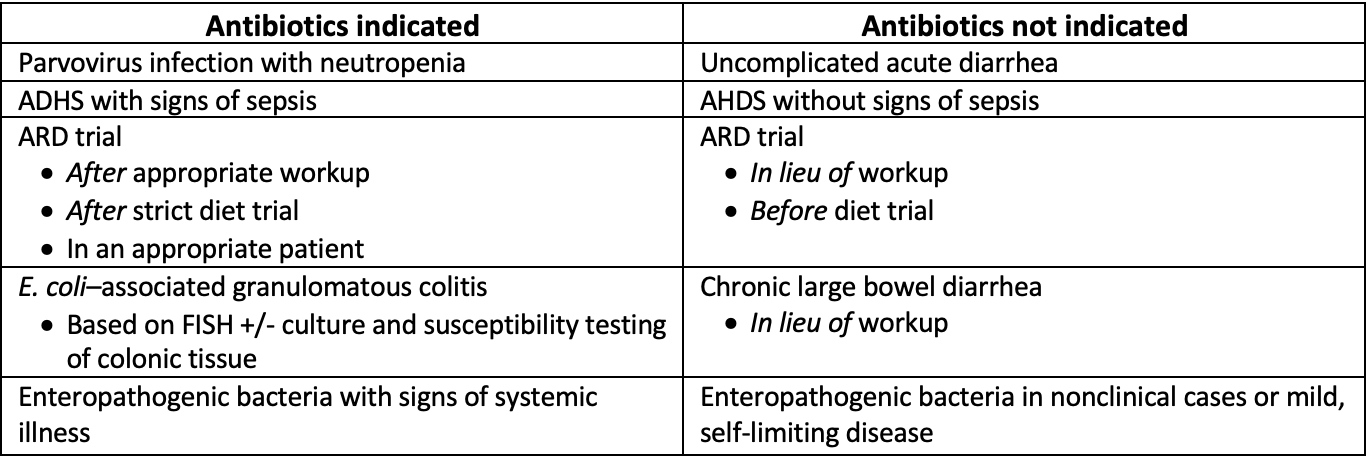
Despite the frequency of antibiotic use for GI disease in dogs, there are relatively few indications for prescribing antimicrobials in this context (Table 2). Overuse could result in antimicrobial resistance and may have long-reaching effects on the host microbiome. Therefore, in the absence of evidence to support their use, antibiotics should be avoided in systemically healthy animals. For systemically ill animals, clinical judgment should be used until more specific criteria are developed.
Table 2. When to use (or avoid) antibiotics
AHDS = acute hemorrhage diarrhea syndrome, ARD = antibiotic-responsive diarrhea, FISH = fluorescence in situ hybridization.
References
1. German AJ, Halladay LJ, Noble PJ. First-choice therapy for dogs presenting with diarrhoea in clinical practice. Vet Rec 2010;167:810-814.
2. Jones PH, Dawson S, Gaskell RM, et al. Surveillance of diarrhoea in small animal practice through the Small Animal Veterinary Surveillance Network (SAVSNET). Vet J 2014;201:412-418.
3. Singleton DA, Noble PJM, Sanchez-Vizcaino F, et al. Pharmaceutical prescription in canine acute diarrhoea: a longitudinal electronic health record analysis of first opinion veterinary practices. Front Vet Sci 2019;6:218.
4. Lappin MR, Blondeau J, Boothe D, et al. Antimicrobial use guidelines for treatment of respiratory tract disease in dogs and cats: Antimicrobial Guidelines Working Group of the International Society for Companion Animal Infectious Diseases. J Vet Intern Med 2017;31:279-294.
5. Weese JS, Blondeau J, Boothe D, et al. International Society for Companion Animal Infectious Diseases (ISCAID) guidelines for the diagnosis and management of bacterial urinary tract infections in dogs and cats. Vet J 2019;247:8-25.
6. Marks SL, Rankin SC, Byrne BA, et al. Enteropathogenic bacteria in dogs and cats: diagnosis, epidemiology, treatment, and control. J Vet Intern Med 2011;25:1195-1208.
7. Schmidt VM, Pinchbeck G, McIntyre KM, et al. Routine antibiotic therapy in dogs increases the detection of antimicrobial-resistant faecal Escherichia coli. J Antimicrob Chemother 2018;73:3305-3316.
8. Igarashi H, Maeda S, Ohno K, et al. Effect of oral administration of metronidazole or prednisolone on fecal microbiota in dogs. PLoS One 2014;9:e107909.
9. Suchodolski JS, Olson E, Honneffer J, et al. Effects of hydrolyzed protein and metronidazole on the fecal microbiome and metabolome in healthy dogs. J Vet Intern Med 2016;30:1407-1519.
10. Fujishiro MA, Lidbury JA, Pilla R, et al. Evaluation of the effects of anthelmintic administration on the fecal microbiome of healthy dogs with and without subclinical Giardia spp. and Cryptosporidium canis infections. PLoS One 2020;15:e0228145.
11. Suchodolski JS, Dowd SE, Westermarck E, et al. The effect of the macrolide antibiotic tylosin on microbial diversity in the canine small intestine as demonstrated by massive parallel 16S rRNA gene sequencing. BMC Microbiol 2009;9:210.
12. Manchester AC, Webb CB, Blake AB, et al. Long-term impact of tylosin on fecal microbiota and fecal bile acids of healthy dogs. J Vet Intern Med 2019;33:2605-2617.
13. Kronman MP, Zaoutis TE, Haynes K, et al. Antibiotic exposure and IBD development among children: a population-based cohort study. Pediatr 2012;130:e794-803.
14. Ni J, Friedman H, Boyd BC, et al. Early antibiotic exposure and development of asthma and allergic rhinitis in childhood. Pediatr 2019;19:225.
15. Ungaro R, Bernstein CN, Gearry R, et al. Antibiotics associated with increased risk of new-onset Crohn's disease but not ulcerative colitis: a meta-analysis. Am J Gastroenterol 2014;109:1728-1738.
16. Shmalberg J, Montalbano C, Morelli G, et al. A randomized double blinded placebo-controlled clinical trial of a probiotic or metronidazole for acute canine diarrhea. Front Vet Sci 2019;6:163.
17. Langlois DK, Koenigshof AM, Mani R. Metronidazole treatment of acute diarrhea in dogs: A randomized double blinded placebo-controlled clinical trial. J Vet Intern Med 2019;34:98-104.
18. Unterer S, Busch K, Leipig M, et al. Endoscopically visualized lesions, histologic findings, and bacterial invasion in the gastrointestinal mucosa of dogs with acute hemorrhagic diarrhea syndrome. J Vet Intern Med 2014;28:52-58.
19. Sindern N, Suchodolski JS, Leutenegger CM, et al. Prevalence of Clostridium perfringens netE and netF toxin genes in the feces of dogs with acute hemorrhagic diarrhea syndrome. J Vet Intern Med 2019;33:100-105.
20. Unterer S, Strohmeyer K, Kruse BD, et al. Treatment of aseptic dogs with hemorrhagic gastroenteritis with amoxicillin/clavulanic acid: a prospective blinded study. J Vet Intern Med 2011;25:973-979.
21. Ziese AL, Suchodolski JS, Hartmann K, et al. Effect of probiotic treatment on the clinical course, intestinal microbiome, and toxigenic Clostridium perfringens in dogs with acute hemorrhagic diarrhea. PLoS One 2018;13:e0204691.
22. Moberg FS, Bjornvad CR, Lorentzen C, et al. Dogs with acute haemorrhagic diarrhoea syndrome not receiving antibiotics have a good prognosis despite initial high AHDS-score and systemic inflammation. Presented at the 29th European College of Veterinary Internal Medicine–Companion Animals Congress, September 2019.
23. Volkmann M, Steiner JM, Fosgate GT, et al. Chronic diarrhea in dogs - retrospective study in 136 cases. J Vet Intern Med 2017;31:1043-1055.
24. Allenspach K, Culverwell C, Chan D. Long-term outcome in dogs with chronic enteropathies: 203 cases. Vet Rec 2016;178:368.
25. Westermarck E, Frias R, Skrzypczak T. Effect of diet and tylosin on chronic diarrhea in beagles. J Vet Intern Med 2005;19:822-827.
26. Kilpinen S, Spillmann T, Westermarck E. Efficacy of two low-dose oral tylosin regimens in controlling the relapse of diarrhea in dogs with tylosin-responsive diarrhea: a prospective, single-blinded, two-arm parallel, clinical field trial. Acta Vet Scand 2014;56:43.
27. Kilpinen S, Spillmann T, Syrja P, et al. Effect of tylosin on dogs with suspected tylosin-responsive diarrhea: a placebo-controlled, randomized, double-blinded, prospective clinical trial. Acta Vet Scand 2011;53:26.
28. Manchester AC, Hill S, Sabatino B, et al. Association between granulomatous colitis in French bulldogs and invasive Escherichia coli and response to fluoroquinolone antimicrobials. J Vet Intern Med 2013;27:56-61.
29. Mansfield CS, James FE, Craven M, et al. Remission of histiocytic ulcerative colitis in boxer dogs correlates with eradication of invasive intramucosal Escherichia coli. J Vet Intern Med 2009;23:964-969.
30. Craven M, Mansfield CS, Simpson KW. Granulomatous colitis of boxer dogs. Vet Clin North Am Small Anim Pract 2011;41:433-445.
31. Leal RO, Simpson K, Fine M, et al. Granulomatous colitis: more than a canine disease? A case of Escherichia coli-associated granulomatous colitis in an adult cat. JFMS Open Rep England: 2017:2055116917731168.
Drs. Grimes and Lidbury work in the Department of Small Animal Clinical Sciences at Texas A&M University. Dr. Lidbury is affiliated with the Gastrointestinal Laboratory, which offers the canine fecal dysbiosis index and fecal enteropathogen testing on a fee-for service basis.
